Abstract
Purpose
Because acute bacterial prostatitis (ABP) is an urgent condition of the prostate but prostatic massage is contraindicated at the onset of ABP, clinical symptoms and urine tests are used for diagnosis. In this study, we compared the clinical symptoms and treatment outcomes of patients with negative urine culture results, to whom only empirical antibiotics were administered, with those of patients with positive urine culture results.
Materials and Methods
Patients were divided into two groups according to the results of urine culture. Then, the clinical symptoms and course of each group were analyzed. In addition, age, symptoms, antibiotics, mean inpatient and outpatient length of treatment, and the treatment outcome of each group were also analyzed.
Results
Of the total 144 patients, the positive urine culture group consisted of 51 patients (35.4%) and the most frequent bacterial strain causing ABP was reported to be Escherichia coli. Fever and storage symptoms were significantly more common in the positive urine culture group than in the negative urine culture group (p=0.031 and 0.047, respectively). Only inpatient treatment was significant longer in the positive urine culture group than in the negative urine culture group (p<0.05). The mean length of treatment of inpatients was 4.8±2.6 days and 6.2±2.9 days in the two groups, respectively. No sequelae such as prostatic abscess or chronic prostatitis were found in either group.
Acute bacterial prostatitis (ABP) is a rare disease that makes up only 5% of prostatitis, and it is possible to diagnose the disease by clinical symptoms. In addition, it is also known as being a rather easy disease to cure [1]. The most frequent bacteria causing ABP have been reported to be Escherichia coli (E. coli), and Enterococcus, Proteus, Pseudomonas, Klebsiella, and Serratia species have also been reported [2-4]. Antimicrobial treatment should be initiated immediately in patients with ABP after blood and urine cultures have been obtained.
Initially, parenteral administration of high doses of bactericidal antibiotics, such as a broad-spectrum penicillin derivative, a third-generation cephalosporin with or without an aminoglycoside, or a quinolone, are required until the fever and other signs and symptoms of infection subside. After initial improvement, a switch to an oral regimen, a quinolone, is appropriate and should be prescribed for at least 4 weeks. In less severe cases, a quinolone may be given orally for 2 to 4 weeks [5].
To treat ABP effectively, we should administer empirical antibiotics first and then decide what to use by the results of antibiotics sensitivity tests of urine culture. If the urine culture test is negative, however, we can only administer empirical antibiotics.
In this study, we compared the clinical symptoms and treatment outcomes of patients with negative urine culture results, to whom only empirical antibiotics were administered, with those of patients with positive urine culture results.
A retrospective analysis of 144 patients diagnosed as having ABP between 2005 and 2009 was performed. Patients were divided into two groups, the negative urine culture group (group 1) and the positive urine culture group (group 2), according to the results of urine culture, and the characteristics and antibiotic use of each group were analyzed. In addition, the microbiological spectrum and antibiotics susceptibility of each group were analyzed.
ABP was diagnosed in all patients according to clinical features (fever, problems with voiding) and the results of laboratory tests. Patients with ABP symptoms and a positive urine culture result, or those with compatible signs but with a negative urine culture result, were selected. Because there are a few reports showing that chronic diseases (e.g., diabetes mellitus, hypertension) do not influence ABP, patients with chronic diseases were included in this study [6]. Patients with other causes of urinary tract infection (e.g., pyelonephritis, sexually transmitted infection) and those who had a history of prostate cancer at the time of diagnosis were excluded. Patients with compatible signs but negative urine culture results due to previous antibiotics use were excluded. In the case of patients who were treated in another hospital before, we used the urine culture result of the previous hospital.
Clinical symptoms and a detailed history were taken together with a physical examination and laboratory investigations. Treatment parameters and microbiology results were documented.
The clinical features considered were as follows: presenting symptoms (fever, pain, dysuria, urinary retention, voiding symptoms, storage symptoms), laboratory investigations (urine analysis, urine culture), and treatment parameters (antibiotic treatment, mean length of treatment). Voiding symptoms (e.g., weak stream, abdominal straining, hesitancy, incomplete bladder emptying, intermittency, and terminal dribbling) and storage symptoms (e.g., frequency, nocturia, and urgency or urge incontinence) were checked by patients' history taking. Many patients complained about dysuria, so we investigated them separately. Urinary retention was defined as more than 400 ml of residual urine. Fever was defined as body temperature >37.5℃. Pyuria was defined as >4 white blood cells (WBCs)/high power field. We divided patients into 5 groups according to urine WBC results. Urine WBC count of 0-2 was considered grade 1, WBC count of 3-5 was considered grade 2, WBC count of 6-10 was considered grade 3, WBC count of 11-20 was considered grade 4, and higher WBC counts were considered as grade 5. We then analyzed the mean pyuria grade. Patients with bacteriuria in their urine were placed into group 2. Microbial susceptibility was determined by using the agar diffusion method according to the guidelines of the National Committee for Clinical Laboratory Standards. Results were analyzed according to two subgroups: urine culture negative and urine culture positive. Results were analyzed by using the chi-square test, Student's t-test, and Wilcoxon rank sum test. A p-value<0.05 was considered statistically significant.
Group 1 consisted of 93 patients (64.6%) and group 2 consisted of 51 patients (35.4%). The mean age of each group was 51.3±14.2 years (range, 23-75 years) and 56.6±16.7 years (range, 20-86 years), respectively.
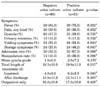
Fever was the most common clinical symptom in both groups. Only fever and storage symptoms were significantly higher in group 2 than in group 1 (p=0.031 and 0.047, respectively). For the mean length of treatment, only inpatient treatment was significantly longer in patient group 2 than in group 1 (p<0.05). Concerning other features, we found no statistically significant differences (Table 1).
Twenty-eight patients in group 1 and 17 patients in group 2 received antibiotics single therapy. Quinolone was used most often: 13 patients (46.4%) in group 1 and 6 patients (35.3%) in group 2. Combination therapy, on the other hand, was received by 65 patients in group 1 and 34 patients in group 2. The combination of a third-generation cephalosporin+aminoglycoside was used most often: 33 patients (50.8%) in group 1 and 10 patients (29.4%) in group 2 (Table 2). In group 2, there were no cases of antibiotics replacement because of resistance.
When the groups were classified according to the presence or absence of prior manipulation, we found that in about 18.8% (27/144) of patients, ABP was secondary to manipulation of the lower urinary tract. Regardless of manipulation, it appeared that 93 patients (64.6%) showed negative urine culture results and 51 patients (35.4%) showed positive urine culture results. E. coli was the most common causative bacteria and no distinct difference in the type of pathogens was noted. Enterococcus, Staphylococcus, Proteus, Pseudomonas, and Klebsiella species were also reported (Table 3).
Of the isolated pathogens, the susceptibility of E. coli to cephalosporin and aminoglycoside was ≥80%. Susceptibility to 2nd- or 3rd-generation cephalosporin, ciprofloxacin, and amikacin showed a relatively high sensitivity rate (Table 4). No sequelae such as prostatic abscess or chronic prostatitis were found in either group.
ABP, which is diagnosed clinically and from urine culture, can be a serious infection. It is usually caused by uropathogens and is associated with fever and chills; rectal, lower back, and perineal pain; and urinary urgency, frequency, and dysuria. The voided urine shows pyuria, microscopic hematuria, and bacteriuria. Prostatic swelling can produce acute urinary retention. Malaise, arthralgia, and myalgia are common symptoms [7,8]. Moreover, prostatic massage and transrectal ultrasonography (TRUS) are not recommended during the early phase of ABP because it is painful for the patient and may lead to bacteremia and sepsis [9]. Most physicians also recommend supportive measures including intravenous hydration and catheter drainage if the patient cannot void [10].
ABP is a kind of febrile urinary tract infection (UTI), but the uropathogens causing UTI do not have correlation with ABP. In addition, fever, pain, and lower urinary tract symptoms (LUTS) were almost the same in groups 1 and 2.
The comparison of the two groups showed that the admission rate, manipulation rate, and mean pyuria grade were lower in group 1, but only the mean length of inpatient treatment was statistically significant (Table 1).
In this study, it was decided that complaining of fever, pain, and LUTS was an admission indication. The mean length of treatment with parenteral antibiotics was 4.8±2.6 days in group 1 and 6.2±2.9 days in group 2.
In the outpatient department after discharge, the mean length of treatment for oral antibiotics was 13.9±11.3 days in group 1 and 13.7±11.1 days in group 2. On the other hand, there was no significant difference in the total length of treatment for inpatients after discharge, which were 18.7±10.5 days and 19.9±11.5 days, respectively. Because we used combination therapy for inpatients whose symptoms were rather serious, we could get a rapid effect. Compared with outpatients who received only single therapy, however, there was not much of a difference in the total length of treatment.
Nowadays, the rate of prostatitis caused by prostate biopsy or catheterization during transurethral surgery is increasing, and these invasive procedures in the lower urinary tract can cause lymphatic or hematogenous spread of infection [2].
Of the total 144 patients, 18.8% (27) of the patients had a history of prior manipulation of the lower urinary tract, mostly prostatic biopsy (51.9%; 14/27) or catheterization (22.2%; 6/27). In group 2, E. coli was detected in 28 patients (54.9%). A total of 19 patients (54.3%) were reported in the group without manipulation and 9 patients (56.3%) were detected in the group with manipulation. In this study, no specific sequelae were noted after manipulation, which was probably caused by exhaustive empirical antibiotics before manipulation. In other papers, the prostatic abscess rate was reported to be 3.1% and the chronic prostatitis rate was reported to be 4.2% [6]. In this study, most of the patients we followed up for more than 6 months were completely cured, but 15 patients who were lost to follow-up still have a possibility of sequelae.
A prostatic abscess may require drainage in addition to antimicrobial treatment. It can be drained through the urethra, through the perineum, and through the rectum [11]. Occasionally, anaerobes or mixed infections may be responsible for the abscess. Cultures should always be obtained, and if fungi are suspected, the laboratory should be informed. Most treatment regimens should include an agent effective against anaerobes.
The most serious complication of TRUS-guided biopsy is bacterial infection. After biopsy, the reported incidence of bacteremia is 16% to 73% and that of bacteriuria is 36% to 44%. Most often, the bacteria diagnosed in either the urine or blood are E. coli [12]. Antibiotic prophylaxis with various drug protocols before biopsy has generally been accepted to reduce infection-related complications. Several studies have shown that quinolone derivatives are effective in lowering the incidence of infectious complications [13-15]. However, some studies have reported patients developing quinolone-resistant infections after prostate biopsy [16,17]. Because quinolone has a broad spectrum, the increase in the use of these drugs has led to resistance. Ciprofloxacin susceptibility was reported in a survey of the antimicrobial susceptibility of uropathogens responsible for female acute uncomplicated cystitis conducted by the Korean Association of Urogenital Tract Infection and Inflammation (KAUTII) in 2006 [18]. Such a result probably reflects the increase in resistant bacteria owing to the excessive use of ciprofloxacin. The guideline for the treatment of urinary tract infection of the Infectious Disease Society of America (IDSA) published in 1999 does not recommended a specific antibiotic for empirical treatment when the local level of resistance among E. coli strains exceeds 20%. The IDSA also emphasized that physicians should obtain information about local resistance rates [19]. In this context, it is very important to select proper antibiotics considering the distinct characteristics of the area and antibiotics resistance.
In a recent guideline for antibiotic treatment of ABP, the administration of cephalosporin or a quinolone alone or in combination with an aminoglycoside was recommended [20]. This study shows that most commonly, antibiotic combination therapy for ABP includes a cephalosporin and an aminoglycoside. For single antibiotic administration, a quinolone is most often preferred (Table 2). In group 2, there was not much of a difference in antibiotics sensitivity between empirical antibiotics, which were used at first, and antibiotics that were used according to the results of urine culture. In addition, there were no cases of antibiotics replacement because of resistance, which proves that empirical treatment is sufficient.
In conclusion, the results of the present study suggest that there is no large difference in clinical symptoms and treatment outcome between empirical therapy and therapy considering urine culture results. Therefore, our results suggest that rapid diagnosis and early use of empirical broad-spectrum antibiotics play an important role in the treatment of ABP.
Because this study was a retrospective study, there could be selection bias. Another limitation is that we did not follow a regular treatment protocol but instead administered different antibiotics depending on the physician's experience. Furthermore, for better study we should not neglect the fact that each physician may have a different view on treatment and we should not be biased as we put more importance on combination therapy.
Group 1 consisted of 93 patients (64.6%), and there was no large difference in clinical symptoms and treatment outcome. In the treatment of ABP, the use of empirical antibiotics can be expected to have sufficient effects regardless of bacterial culture. However, it is hard to determine the causative bacteria of ABP by urine culture results alone.
Figures and Tables
References
1. Neal DE Jr. Nickel JC, editor. Acute bacterial prostatitis. Textbook of prostatitis. 1999. 1st ed. Oxford: Isis Medical Media;115–121.
2. Ha US, Kim ME, Kim CS, Shim BS, Han CH, Lee SD, et al. Acute bacterial prostatitis in Korea: clinical outcome, including symptoms, management, microbiology and course of disease. Int J Antimicrob Agents. 2008. 31:Suppl 1. S96–S101.
3. Lee JY, Kim SJ, Ahn HS. The value of serum prostate-specific antigen in the diagnosis and follow-up of acute prostatitis. Korean J Urol. 2001. 42:800–803.
4. Crawford ED, Haynes AL Jr, Story MW, Borden TA. Prevention of urinary tract infection and sepsis following transrectal prostatic biopsy. J Urol. 1982. 127:449–451.
5. Naber KG, Bergman B, Bishop MC, Bjerklund-Johansen TE, Botto H, Lobel B, et al. Urinary Tract Infection (UTI) Working Group of the Health Care Office (HCO) of the European Association of Urology (EAU). EAU guidelines for the management of urinary and male genital tract infections. Eur Urol. 2001. 40:576–588.
6. Cho IR, Lee KC, Lee SE, Jeon JS, Park SS, Sung LH, et al. Clinical outcome of acute bacterial prostatitis, a multicenter study. Korean J Urol. 2005. 46:1034–1039.
7. Hua VN, Schaeffer AJ. Acute and chronic prostatitis. Med Clin North Am. 2004. 88:483–494.
8. Krieger JN, Nyberg L Jr, Nickel JC. NIH consensus definition and classification of prostatitis. JAMA. 1999. 282:236–237.
9. Vahlensieck W Jr, Hofstetter AG. Weider W, Madsen PO, Schiefer HG, editors. Acute prostatitis and prostatic abscess. Prostatitis. 1994. 1st ed. Berlin: Springer-Verlag;133–148.
10. Schaeffer AJ. Diagnosis and treatment of prostatic infections. Urology. 1990. 36:5 Suppl. 13–17.
11. Naber KG, Weidner W. Armstrong D, Cohen J, editors. Prostatitis, epididymitis and orchitis. Infectious disease. 1999. 3rd ed. London: Mosby;1–58.
12. Lindert KA, Kabalin JN, Terris MK. Bacteremia and bacteriuria after transrectal ultrasound guided prostate biopsy. J Urol. 2000. 164:76–80.
13. Aron M, Rajeev TP, Gupta NP. Antibiotic prophylaxis for transrectal needle biopsy of the prostate: a randomized controlled study. BJU Int. 2000. 85:682–685.
14. Sieber PR, Rommel FM, Agusta VE, Breslin JA, Huffnagle HW, Harpster LE. Antibiotic prophylaxis in ultrasound guided transrectal prostate biopsy. J Urol. 1997. 157:2199–2200.
15. Kapoor DA, Klimberg IW, Malek GH, Wegenke JD, Cox CE, Patterson AL, et al. Single-dose oral ciprofloxacin versus placebo for prophylaxis during transrectal prostate biopsy. Urology. 1998. 52:552–558.
16. Shigehara K, Miyagi T, Nakashima T, Shimamura M. Acute bacterial prostatitis after transrectal prostate needle biopsy: clinical analysis. J Infect Chemother. 2008. 14:40–43.
17. Feliciano J, Teper E, Ferrandino M, Macchia RJ, Blank W, Grunberger I, et al. The incidence of fluoroquinolone resistant infections after prostate biopsy--are fluoroquinolones still effective prophylaxis? J Urol. 2008. 179:952–955.
18. Kim ME, Ha US, Cho YH. Prevalence of antimicrobial resistance among uropathogens causing acute uncomplicated cystitis in female outpatients in South Korea: a multicentre study in 2006. Int J Antimicrob Agents. 2008. 31:Suppl 1. S15–S18.
19. Warren JW, Abrutyn E, Hebel JR, Johnson JR, Schaeffer AJ, Stamm WE. Guidelines for antimicrobial treatment of uncomplicated acute bacterial cystitis and acute pyelonephritis in women. Infectious Diseases Society of America (IDSA). Clin Infect Dis. 1999. 29:745–758.
20. Naber KG, Bishop MC, Bjerklund-johansen TE, Botto H, Cek M, Grabe M, et al. EAU guideline office. The management of urinary and male genital tract infections. European Association of Urology Guidelines. 2006. Arnhem: Drukkerij Gelderland;1–126.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download