Abstract
Purpose
We evaluated the usefulness of the nuclear matrix protein 22 BladderChek (NMP22BC) test for the screening and follow-up of bladder cancer.
Materials and Methods
From February 2006 to September 2009, we enrolled 1,070 patients who had hematuria or who were being followed up for bladder cancer. We compared the sensitivity and specificity of the NMP22BC test with those of urine cytology.
Results
The sensitivity of the NMP22BC test (77.5%) was significantly higher than that of urine cytology (46.3%). The specificity of the NMP22BC test was 88.8%, compared with 97.9% for urine cytology. The sensitivity of the NMP22BC test (81.8%) in non-muscle-invasive bladder cancer was higher than that of cytology (36.4%). However, the sensitivity of the NMP22BC test and of urine cytology in invasive bladder cancer were 57.1% and 92.9%, respectively. The sensitivity of the NMP22BC test was higher for low-grade bladder cancer (83.9%) than for high-grade (62.5%), and the sensitivity of cytology was higher for high-grade bladder cancer (66.7%) than for low-grade (37.5%). Follow-up bladder cancer was detected in 262 patients. The sensitivity of the NMP22BC test in that group (72.7%) was decreased and the specificity (91.7%) was increased. The sensitivity of cytology (54.5%) in the follow-up group was increased and the specificity (95.6%) was decreased. The presence of pyuria was significantly associated with the lower specificity of the NMP22BC test.
Conclusions
The greater sensitivity of the NMP22BC test may be more useful for the diagnosis of non-muscle-invasive bladder cancer and low-grade bladder cancer than for the diagnosis of invasive or high-grade bladder cancer. If the NMP22BC test is performed in the absence of pyuria, it may play a compensatory role for urine cytology.
More than 95% of bladder cancers are transitional cell carcinomas that originate from transitional epithelial cells. Most detected cases are non-muscle-invasive bladder cancer that can be completely resected by transurethral bladder tumor resection. Nonetheless, the recurrence rate is high, and non-muscle-invasive bladder cancer can occasionally progress to invasive bladder cancer or metastatic bladder cancer. Therefore, early diagnosis and comprehensive, regular follow-up have an important influence on the prognosis of bladder cancer [1].
Cystoscopy and urine cytology are usually performed for the early detection of bladder cancer and in the assessment of recurrence. However, cystoscopy causes pain and discomfort in patients, and in cases of small tumors or carcinoma in situ, a diagnosis may not be readily made. Urine cytology has the advantage of high specificity, but it also has shortcomings: its sensitivity for well-differentiated or low-grade disease is low and may differ depending on examiners [2].
To overcome such shortcomings of the existing diagnostic methods for bladder cancer, diverse tumor markers have been investigated [3-5]. For example, the nuclear matrix protein (NMP)-22 test detects nuclear matrix protein in urine. This protein is produced during cell division and is associated with transitional epithelial cancer [6]. Recently, the NMP22BladderChek (NMP22BC) test (Matritech, USA) was developed and approved by the US Food and Drug Administration to be used for the diagnosis of bladder cancer and for follow-up tests. The previously used NMP22 test applied enzyme-linked immunosorbent assays (ELISAs), which were performed in laboratories, and involved the collection of several samples. Thus, the urine samples had to be stored refrigerated, the test period could be long, and additional equipment and personnel were required for reading the results. Accordingly, although it was approved in 1996, the NMP22 test saw limited use in clinics. The NMP22BC test that we used in the present study can be performed immediately after collecting a patient's urine in an outpatient clinic. Thus, it has the advantage that the results can be readily obtained and additional tests can be done immediately. Here we assessed the efficacy of the NMP22BC test in the diagnosis of bladder cancer as well as for follow-up, and compared the results with those for urine cytology and microscopic urine analysis.
We studied 1,070 patients who visited our hospital for hematuria or for follow-up for bladder cancer from February 2006 to September 2009. We performed the NMP22BC test, urine cytology applying Tripath thin-layer technology, and microscopic urine analysis. Of the 1,070 patients, 650 were male and 420 were female; the patients' mean ages were 59.0±15.3 years and 59.8±14.3 years, respectively. Of the 1,070 patients, 262 were being followed up for bladder cancer; the mean age of this subgroup was 65.2±13.0 years, and the group included 192 males and 70 females. Of the 1,070 cases, 80 were diagnosed as having bladder cancer by this study. To minimize false-positives, patients with a past history of urinary tract infection, cystitis, or urolithiasis were excluded. For upper urinary tract evaluation, the findings were confirmed by ultrasonography or intravenous pyelography or abdomen computed tomography. For macroscopic hematuria evaluation, the findings were confirmed by cystoscopy. Microscopic urine analysis was done for all patients.
NMP22BC tests were done according to the recommendations of the manufacturer. Urine was collected after being retained in the bladder for longer than 2 hours. Drops of fresh urine were applied to the NMP22BC kit within 2 hours of collection, and the results were read after 30 minutes. Results showing a vertical line in both the control window and the test window were read as positive. A vertical line appearing in the control window indicated that the test was performed correctly. The test was effective in all subjects. The diagnosis of bladder cancer was confirmed by histological tests after resection, and the degree of cell differentiation was determined by application of the 1998 World Health Organization/International Society of Urological Pathology (WHO/ISUP) standard.
To explain false-positives on the NMP22BC test in patients without bladder cancer, microscopic urine analysis was performed on a specimen identical to the one used for the NMP22BC test, and the factors that could give rise to a false-positive result were analyzed. Variables for the assessment of the efficiency of the test were calculated as follows. Sensitivity was calculated as true positive/(true positive+false negative)×100, and specificity was calculated as true negative/(true positive+false positive)×100. For statistical calculations, we used SPSS version 12.0 (SPSS, USA). We used the chi-square test, the Fisher's exact test, and the McNemar test, and p-values less than 0.05 were considered to be significant.
The results of the NMP22BC testing were positive for 173 cases (16.2%) out of a total of 1,070 patients; for urine cytology, the results were positive for 58 cases (5.4%). The sensitivity of the NMP22BC test was 77.5%, which was higher than the sensitivity of urine cytology, which was 46.3%. The specificity of the NMP22 test was 88.8%, which was lower than the 97.9% specificity of urine cytology (Table 1). A total of 880 patients visited our hospital for hematuria; the sensitivity (80.9%) of the NMP22BC test was increased in this group but the specificity (87.9%) of the test was decreased; for urine cytology, the sensitivity (40.4%) in this group was decreased but the specificity (98.6%) was increased (p<0.01) (Table 2).
For the 262 patients under follow-up observation, the sensitivity (72.7%) of the NMP22BC test was decreased but the specificity (91.7%) was increased. For urine cytology, by contrast, the sensitivity (54.5%) was increased in the follow-up group but the specificity (95.6%) was decreased (but this difference was not statistically significant) (p>0.05) (Table 3). During the study, 80 patients (7.5%) were diagnosed with bladder cancer. Among the 80 cases, 66 had non-muscle-invasive bladder cancer and 14 had invasive bladder cancer. Among the diagnosed patients, the sensitivity of the NMP22BC test for non-muscle-invasive bladder cancer was 81.8%, which was higher than the 36.4% sensitivity for urine cytology (p<0.01). However, for the 14 patients with invasive cancer, the sensitivity of urine cytology was 92.9%, which was higher than the 57.1% sensitivity of the NMP22BC test, but this difference was not statistically significant (p>0.05) (Table 4).
When bladder cancer was classified according to differentiation grade, there were 56 low-grade cases and 24 high-grade cases. When sensitivity was calculated according to tumor grade, the NMP22BC test had a sensitivity of 83.9% and urine cytology had a sensitivity of 37.5% for low-grade cancer (p<0.01); for high-grade tumors, the sensitivity of the NMP22BC test was 62.5% and that for urine cytology was 66.7% (the difference was not statistically significant; p>0.05) (Table 5).
To evaluate the cause of the low false-positive rate for the NMP22BC test, microscopic urine analysis was done on an identical urine specimen. For the 990 patients who were not diagnosed as having bladder cancer, and based on the white blood cells (WBC) detected by microscopic urine analysis (5 WBC/high power field (HPF)), the specificity of the NMP22BC test was increased to 92.7% for the group with ≤5 WBC/HPF but decreased to 66.9% for the group with >5 WBC/HPF.
Among the 990 patients, 808 had hematuria. The specificity of the NMP22BC test was 59.2% in the hematuria group with >5 WBC/HPF and 89.6% in the hematuria group with ≤5 WBC/HPF (p<0.01). Likewise, in patients undergoing follow-up for bladder cancer, the specificity of the NMP22BC test was 90.8% in the group with >5 WBC/HPF and 47.7% in patients with ≤5 WBC/HPF (Table 6).
Among the 990 patients who were not diagnosed as having bladder cancer, the specificity of urine cytology increased to 98.6% in the overall group with ≤5 WBC/HPF but decreased to 94.0% in the overall group with >5 WBC/HPF. In the hematuria group, the specificity of urine cytology was 98.3% in those with >5 WBC/HPF and 87.5% in those with ≤5 WBC/HPF (p<0.01). Likewise, in the patients undergoing follow-up for bladder cancer, the specificity of urine cytology was 95.0% in those with >5 WBC/HPF and 89.3% for cases with ≤5 WBC/HPF (Table 7).
Because of the high recurrence rates and progression of bladder cancer, diagnosis and follow-up observations are critical. Urine cytology has been performed as a general test for the diagnosis of bladder cancer. However, depending on disease stage and differentiation grade, urine cytology shows low sensitivity (30-50%) [7-9]. Even among patients treated for bladder cancer and undergoing follow-up, satisfactory results have not been obtained by regular cystoscopic examination or by urine cytology (except in a few cases). Hence, additional tests are needed. Diverse studies have been conducted to develop methods that can diagnose bladder cancer readily by using a patient's urine. Such biomarkers include the detection of hematuria, bladder tumor antigen (BTA) stat, BTA-TRAK, NMP22, BLCA-4 and BCLA-1, survivin, cytokeratin, HA-HAase test, microsatellite analysis, telomerase, uCyt, and the Urovysion test applying fluorescence in situ hybridization (FISH) [3]. When used as screening tests in high-risk patients, these tests have been shown to be effective for early detection and to reduce costs [3].
NMP is present in low concentrations in urine and in normal cells. However, in tumor cells, it is increased 80-fold. Thus, in cases of bladder cancer, it is excreted in urine in high concentrations. The target antigen NMP22 or nuclear mitotic apparatus (NuMA) protein of the NMP22BC test is present within epithelial cells and during cell division. It aids in the production of the spindle and the reformation of the nucleus [10]. The NMP22BC test (Matritech) was developed as one such tumor marker, and numerous institutions have reported studies conducted on it [3-5,11]. The previously used NMP22 test method using ELISA is performed in laboratories after the collection of several specimens. Hence, urine samples must be stored refrigerated. Because the test cannot be conduced until all specimens are collected, the test period is longer, and additional equipment and personnel are required for reading the results. Although it was approved by the US Food and Drug Administration in 1996, it is not actually used in clinics. The NMP22BC used in our study has the advantage that the test can be performed immediately after the collection of urine from a patient in an outpatient clinic, and thus rapid results can be obtained, and the value of additional tests can be decided on immediately.
In our study, the sensitivity of the NMP22BC test performed on 1,070 patients who visited our hospital for hematuria or for follow-up observation of bladder cancer was 77.5%, and the specificity was 88.8%. In other studies, Grossman et al reported a sensitivity of 55.7% and a specificity of 85.7% for the NMP22BC test [12]. Tomera et al conducted a prospective study of 1,300 patients with epithelial cell tumor symptoms or risk factors and performed NMP22BC tests, urine cytology, and cystoscopy [13]. For all disease stages, the sensitivity of the NMP22BC test was higher than the sensitivity of urine cytology; as the degree of cell differentiation increased, the sensitivity became higher [12].
In our study, the sensitivity of the NMP22BC test was 81.8% for non-muscle-invasive bladder cancer, which was higher than the sensitivity of 36.4% for urine cytology (p<0.01). For invasive cancer, the sensitivity of the NMP22BC test was 57.1%, which was lower than the 92.9% sensitivity of urine cytology; however, this difference was not statistically significant (p>0.05). The sensitivity of the NMP22BC test for low-grade bladder cancer was 83.9% and for high-grade bladder cancer it was 62.5%. For urine cytology, sensitivity was 37.5% for low-grade bladder cancer and 66.7% for high-grade bladder cancer (p>0.05). Our results differ from other reports showing that, depending on disease stage and the differentiation grade of tumors, the sensitivity of the NMP22 test tends to be increased [13].
It thus appears that the NMP22BC test may be useful for the diagnosis of non-muscle-invasive bladder cancer as well as for low-grade cancer rather than for invasive and highly differentiated cancer, although additional studies are required. In our study, the sensitivity of urine cytology was 46.3% and the specificity was 97.9%, which is similar to the sensitivity (40-62%) and specificity (94-100%) of urine cytology reported elsewhere [4]. Among the 1,070 patients, 880 were seen for hematuria evaluation and 262 for follow-up of bladder cancer. The sensitivity and specificity of both groups showed trends similar to those of the overall group. Differences between the NMP22BC test and urine cytology in the group of follow-up patients were not statistically significant (Table 3). This finding of no significant difference in the cancer follow-up group is thought to be due to the small number of patients. Therefore, additional research is needed.
It is well known that for follow-up observation, the NMP22 test has the advantages of being noninvasive and being readily performed. However, it is not considered to be a method that can replace cystoscopy, and the most important reason for this may be its low specificity [9]. To explain the low specificity of the NMP22BC test, we performed leukocyte analysis by microscopic urine testing by using the same specimen that had been used for the NMP22BC test. In cases with fewer than 5 white blood cells/HPF, the specificity of the NMP22BC test improved to 92.7% in the overall group. Also, the presence of pyuria in the group with hematuria and the group being followed up for bladder cancer was significantly associated with a lower specificity of the NMP22BC test (Table 6). According to urine cytology, the existence of pyuria contributed to the low specificity in all three groups (Table 7). Atsü et al also reported that cases with hematuria and pyuria are associated with false-positives, which agrees with our findings [14]. The evaluation of hematuria was eliminated because our study included patients with hematuria. However, the low specificity of the NMP22BC test could not be explained completely by the above results. The exclusion of cases with inflammation within the bladder or infection, cases with a history of mechanical manipulation within the bladder, cases with foreign material within the bladder including urinary catheter insertion, and cases with tumors other than bladder cancer in the urogenital system could reduce the false-positive rate [15,16]. Sharma et al reported that when the above criteria were applied, the specificity and positive predictive rates of the NMP22BC test increased from 82% and 38.9% to 95.6% and 87.5%, respectively [17]. In our study, results with these exclusion criteria could not be obtained, and additional studies are required.
The greater sensitivity of the NMP22BC test may be useful for the diagnosis of non-muscle-invasive and low-grade bladder cancer but not for the diagnosis of invasive and high-grade bladder cancers. Pyuria is one condition that decreases the specificity of the test. Thus, if the test is done for patients without pyuria, it may play a useful, compensatory role relative to urine cytology.
Figures and Tables
TABLE 2
NMP22 BladderCheck test and urine cytology in patients who were seen for hematuria evaluation

TABLE 3
NMP22 BladderCheck test and urine cytology in patients who were seen for follow-up of bladder cancer

TABLE 4
NMP22BladderChek test and urine cytology for detecting bladder cancer according to tumor stage
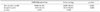
TABLE 5
NMP22BladderChek test and urine cytology for detecting bladder cancer according to tumor grade

References
1. Heney NM, Ahmed S, Flanagan MJ, Frable W, Corder MP, Hafermann MD, et al. Superficial bladder cancer: progression and recurrence. J Urol. 1983. 130:1083–1086.
2. Park JO, Moon DG, Cheon J, Kim JJ, Yoon DK. Urinary NMP (nuclear matrix protein) 22 in screening and post-treatment follow-up bladder cancer. Korean J Urol. 1999. 40:551–556.
3. Lokeshwar VB, Habuchi T, Grossman HB, Murphy WM, Hautmann SH, Hemstreet GP 3rd, et al. Bladder tumor markers beyond cytology: International Consensus Panel on bladder tumor markers. Urology. 2005. 66:6 Suppl 1. 35–63.
4. Bassi P, De Marco V, De Lisa A, Mancini M, Pinto F, Bertoloni R, et al. Non-invasive diagnostic tests for bladder cancer: a review of the literature. Urol Int. 2005. 75:193–200.
5. Quek ML, Sanderson K, Daneshmand S, Stein JP. New molecular markers for bladder cnacer detection. Curr Opin Urol. 2004. 14:259–264.
6. Miyanaga N, Akaza H, Ishikawa S, Ohtani M, Noguchi R, Kawai K, et al. Clinical evaluation of nuclear matrix protein 22 (NMP22) in urine as a novel marker for urothelial cancer. Eur Urol. 1997. 31:163–168.
7. Murphy WM, Emerson LD, Chandler RW, Moinuddin SM, Soloway MS. Flow cytometry versus urinary cytology in the evaluation of patients with bladder cancer. J Urol. 1986. 136:815–819.
8. Murphy WM, Soloway MS, Jukkola AF, Crabtree WN, Ford KS. Urinary cytology and bladder cancer. The cellular features of transitional cell neoplasms. Cancer. 1984. 53:1555–1565.
9. Kwon DH, Hong SJ. The clinical utility of BTA TRAK, BTA stat, NMP22 and urine cytology in the diagnosis of bladder cancer: a comparative study. Korean J Urol. 2003. 44:721–726.
10. Landman J, Chang Y, Kavaler E, Droller MJ, Liu BC. Sensitivity and specificity of NMP-22, telomerase, and BTA in the detection of human bladder cancer. Urology. 1998. 52:398–402.
11. Glas AS, Roos D, Deutekom M, Zwinderman AH, Bossuyt PM, Kurth KH. Tumor markers in the diagnosis of primary bladder cancer. A systematic review. J Urol. 2003. 169:1975–1982.
12. Grossman HB, Messing E, Soloway M, Tomera K, Katz G, Berger Y, et al. Detection of bladder cancer using a point-of-care proteomic assay. JAMA. 2005. 293:810–816.
13. Tomera KM. NMP22BladderChek test: point-of-care technology with life-and money-saving potential. Expert Rev Mol Diagn. 2004. 4:783–794.
14. Atsü N, Ekici S, Oge O, Ergen A, Hascelik G, Ozen H. False-positive result of the NMP22 test due to hematuria. J Urol. 2002. 167:555–558.
15. Chang SH, Kim YH, Kim ME. Urinary survivin test compared to the nuclear matrix protein (NMP)-22 test and urine cytology for the diagnosis of bladder cancer. Korean J Urol. 2006. 47:1041–1045.
16. Kim H, Chang SG, Kim JI. Significance of urinary NMP22 in patients with bladder tumor as a diagnostic test. Korean J Urol. 1998. 39:450–453.
17. Sharma S, Zippe CD, Pandrangi L, Nelson D, Agarwal A. Exclusion criteria enhance the specificity and positive predictive value of NMP22 and BTA stat. J Urol. 1999. 162:53–57.
18. Ozer G, Altinel M, Kocak B, Yazicioglu A, Gonenc F. Value of urinary NMP-22 in patients with renal cell carcinoma. Urology. 2002. 60:593–597.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download