Abstract
Purpose
Percutaneous nephrolithotomy (PCNL) is the procedure of choice for treating large renal stones. Pneumatic lithotripsy (Lithoclast®) is effective regardless of the stones' composition, and ultrasonic lithotripsy allows the aspiration of small debris during lithotripsy. We investigated the efficacy and safety of PCNL via Lithoclast® alone or combined with ultrasonic lithotripsy.
Materials and Methods
Thirty-five (group A) and 39 (group B) patients underwent Lithoclast® PCNL and combination therapy, respectively, from May 2001 to March 2010, and the two groups were compared in terms of stone size, location, and composition; operative time; average number of treatments; hospital days; hemoglobin loss; ancillary procedures; rate of device failure; and initial and total stone-free rates.
Results
The two groups did not differ significantly in preoperative stone size, location, or composition; the average number of treatments; or the initial and overall stone-free rates. However, combination therapy was associated with a significantly lower operative time (181±50 vs. 221±65 min, respectively, p=0.004), number of hospital days (11.6±3.8 vs. 14.2±4.4 days, respectively, p=0.009), and average hemoglobin loss (1.12±0.61 vs. 1.39±1.02 g/dl, respectively, p=0.013). Transfusions were required in 6 patients (4 and 2 in each group, respectively), but there were no significant complications related to percutaneous access. There were 2 (5.7%) mechanical failures (Lithoclast® probe fracture) in the group A and 5 (12.8%) in the group B (2 cases of suction tube obstruction, 3 cases of overheating).
Conclusions
The combination of ultrasonic lithotripter and Lithoclast® is more effective than Lithoclast® alone because it significantly decreases operative time, hemoglobin loss, and the hospital stay. This may reflect the superior power of Lithoclast® and the ability to aspirate the debris during ultrasonic lithotripsy.
Fernstrom and Johansson first removed a renal calculus through a nephrostomy tract in 1976, and percutaneous nephrolithotomy (PCNL) is now accepted as the procedure of choice for those patients who have large renal stones (>2 cm in diameter), infected stones, or lower calyceal stones with obstruction or anatomical variations in the renal collecting system as well as for those patients in whom prior extracorporeal shock wave lithotripsy (ESWL) has failed [1]. ESWL of larger stone masses results in many stone fragments that rarely pass down the ureter spontaneously without causing an obstruction.
In recent decades, endoscopic technology and operative techniques have consistently advanced, which has increased the success rate (>90%) of PCNL and decreased the associated complications and morbidity [2]. Consequently, a wide range of lithotripsy techniques are currently available. One of these is ultrasonic lithotripsy, in which the stones are fragmented while suction is applied simultaneously [3]. This technique induces minimal tissue injury and could be considered as a standard modality for PCNL. However, the fragmentation process can be laborious, especially if the stone is large or dense, and continuous irrigation is needed to prevent the probe from overheating. Pneumatic lithotripsy may be more suitable for harder stones because it is more powerful than the other lithotripsy techniques and it can minimize tissue injury when applied cautiously. However, a disadvantage of this technique is that the stone fragments must be extracted with graspers, which is highly time-consuming.
Little has been published about the use of ultrasonic lithotripters for PCNL in Korea. The objective of this study was therefore to compare the effectiveness of pneumatic lithotripsy combined with ultrasonic lithotripsy with the effectiveness of pneumatic lithotripsy alone.
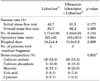
A review of medical records between May 2001 and March 2010 identified 74 patients who had undergone PCNL by the same experienced surgeon. Details of the patients and the procedures and the postoperative clinical results and complications were recorded. Of the 74 patients, 35 (group A) underwent PCNL with Lithoclast® (Richard Wolf GmbH, Knittlingen, Germany), and 39 (group B) underwent simultaneous combination therapy with Lithoclast® and an ultrasonic lithotripter (Richard Wolf GmbH, Knittlingen, Germany). The patients were randomly assigned to receive PCNL performed by pneumatic lithotripsy or a combination of ultrasonic and pneumatic lithotripsy. Because the ultrasonic device was set up in our hospital in 2006, a few group A patients underwent PCNL with the Lithoclast® only since 2006. There were no significant differences between the two groups in terms of the mean patient age (55.9±14.5 vs. 54.5±13.3 years, respectively, p=0.660) (Table 1). The inclusion criteria included the presence of large (>2 cm) renal stones, low-pole stones, and partial and complete staghorn calculi. The exclusion criteria were a patient age below 18 years, the presence of a coagulopathy, and pregnancy.
The stone size and type were documented preoperatively. Before the operation, all the patients were subjected to intravenous urography (IVU) or computed tomography (CT), and if needed, an assessment of renal function was done by dimercaptosuccinic acid scanning. The urine culture had to be sterile and antibiotics were given 12 hours before the operation.
For the group A patients, lithotripsy was performed by using a Lithoclast®, and lithotripsy was continued until the stone had fragmented into pieces small enough to be removed directly by a two- or three-pronged grasper. For the group B patients, lithotripsy was usually first initiated with a few bursts of the Lithoclast®, after which the ultrasonic lithotripter was used. At the end of the operation, a nephrostomy tube (a 20 Fr self-retaining balloon catheter) was placed and maintained until the hematuria disappeared.
A number of parameters were recorded. The success of PCNL treatment was evaluated by two categories: 1) the initial stone-free rate, which was defined as no visible residual calcification or remnant calcification smaller than 4 mm in diameter (clinically insignificant residual fragment) on a plain KUB or CT image after the first session, and 2) the overall stone-free rate, which was defined as no residual fragment or <4 mm on the KUB film or CT image 4 weeks after the last treatment. The number of sessions referred to the number of PCNL procedures each patient underwent. The total operation time was calculated by adding the time taken to perform the percutaneous nephrostomy to the time taken for the lithotripsy. Hospital days referred to the total number of days the patients stayed in the hospital after the first PCNL, during which time some patients also underwent a second or third PCNL procedure. After the last PCNL procedure, ESWL was used as an accessory treatment in the patients with residual stones ≥4 mm. The characteristics of the stones were evaluated. The complications associated with the PCNL session were recorded, including postoperative fever, total hemoglobin loss, need for transfusion, perforation of the renal pelvis, and the development of pneumothorax or pleural effusion. The total rates of technical lithotripter-related problems that occurred during the PCNL were also recorded.
All data were statistically analyzed by using MedCalc® (MedCalc Software, Mariakerke, Belgium). The results were expressed as Means±SDs. Student's t-test was used to compare the mean values of the continuous variables, whereas the chi-square test was used to compare the discrete variables. A p-value less than 0.05 was considered significant.
As shown in Table 1, groups A (Lithoclast® alone) and B (Lithoclast® in combination with ultrasonic lithotripsy) were similar in terms of stone size (29.0±17.6 and 33.3±18.4 mm, respectively, p=0.318). The two groups also did not differ significantly in the distribution of stone type (p=0.510): 20 group A patients and 24 group B patients had staghorn calculi, and the remaining stones were renal calyx stones or renal pelvis stones.
After the first PCNL session, 19 (54.3%) of the group A patients and 15 (38.5%) of the group B patients continued to have clinically significant residual stone fragments, and they had to undergo a second or a third PCNL. Thus, as shown in Table 2, the initial stone-free rates for groups A and B were 45.7% and 61.5%, respectively (p=0.177). The average number of treatment sessions for groups A and B was 1.71±0.93 and 1.44±0.64, respectively; this difference did not achieve statistical significance (p=0.134). Whereas groups A and B did not differ significantly in their overall stone-free rates or stone composition (p=0.369, p=0.935), combination therapy significantly reduced the total operative time (181±50 vs. 221±65 min, respectively, p=0.004) and the duration of the postoperative hospital stay (11.6±3.8 vs. 14.2±4.4, respectively, p=0.009). After the last PCNL session, 5 group A patients (14.3%) and 3 group B patients (7.7%) continued to have clinically significant residual stone fragments and therefore underwent ESWL treatment.
The rates of various complications associated with the first PCNL are shown in Table 3. Combination therapy significantly reduced the postoperative hemoglobin loss (1.12±0.61 vs. 1.39±1.02 g/dl, respectively, p=0.013). Four (11.4%) and 2 (6.9%) group A and B patients, respectively, experienced bleeding that required a transfusion to manage it. None of the patients experienced severe bleeding that required embolization. There were also no cases of pleural or lung injury due to the puncture. None of the patients required ureteral catheterization or ureteroscopy to remove residual stones. Lithoclast® alone was associated with mechanical failures in 2 group A patients (5.7%), and this was due to fracturing of the lithoclast probe (Table 3). Combination therapy was associated with mechanical malfunction in 5 group B patients (12.8%) due to suction tube obstruction (2 patients) and device failure that required resetting of the machine every 30 minutes (3 patients).
Although ESWL has revolutionized the management of urinary stones, PCNL still plays an important role in the treatment of large or multiple kidney stones [4]. The PCNL procedure can be divided into three steps, namely, percutaneous access, tract dilation, and stone fragmentation. The success of PCNL is related to the ability to achieve an optimal access tract. A subcostal tract through the posterior middle or the inferior calyx may be acceptable for stones in the renal pelvis and those in the middle or inferior calyx [5]. For stones in the superior calyx and for staghorn stones, an approach through the superior calyx has clear advantages with acceptable complications. A significant chest complication rate of about 5% must be considered when choosing the supracostal approach [5]. In the present study, the punctures were made at the mid or lower calyx to prevent chest complications. Indeed, no complications related to the puncture were observed. Another fundamental PCNL procedural step is the dilation of the tract that creates the nephrostomy access. This is commonly achieved by using Amplatz fascial dilators, Alken metal dilators, or pneumatic balloon dilators [6]. Park et al have reported on the advantage of the attending radiologist preoperatively achieving an access tract, which reduces operation time and complications [7].
With regard to the third PCNL procedural step, namely, stone fragmentation, a number of lithotripsy approaches have been developed. The first is electrohydraulic lithotripsy (EHL), which is based on spark-gap technology and was first introduced by Yutkin (1955). Raney and Handler have reported the use of EHL for open nephrolithotomy [8]. EHL is cheaper than the other lithotripsy devices. However, despite the technical improvements and extensive clinical experience with EHL, it remains the least safe of all lithotripsy devices. In fact, Hofbauer et al showed that EHL is associated with a higher rate of perforation than is the use of a pneumatic lithotripter (17.6% vs. 2.6%, respectively) [9].
Another lithotripter is the holmium:yttrium-aluminum-garnet (Ho:YAG) laser, which is a high-energy pulse solid-state laser. The efficacy of the Ho:YAG laser is correlated with the pulse energy output. It has been reported to be a safe and effective treatment modality for large renal stones, even at high power settings [10,11]. The advantages of the Ho:YAG laser are that it effectively fragments all sorts of renal calculi, and the fibers are small enough to be passed through flexible endoscopes [12]. However, one disadvantage of the Ho-YAG laser is that the resulting stone fragments must be extracted by grasping each one individually. Another disadvantage is that the inadvertent exposure of the urothelium to the laser beam may lead to perforation or bleeding from shock-wave exposure and heating. Moreover, the cost of this laser system is high [13].
The Lithoclast® lithotripter uses pneumatic ballast, which crushes the stone without producing any thermal effects [14]. Because this mechanical energy passes along the metal wire to the stone, the probe works like a chisel on the stone surface [15]. This modality destroys all stones, regardless of their composition. Another advantage of the Lithoclast® is that its cost is low [16]. However, it also suffers from the disadvantage that the stone fragments it produces are usually large and are likely to be displaced. In addition, in the case of granulation tissue-wrapped stones or impacted stones in a narrowed calyceal neck, hemorrhage is likely because of the mechanical impact from the rod and repeated friction between the stone and the mucosa of the renal collection system, and this hemorrhage blurs the vision of the field.
Ultrasonic lithotripsy uses mechanical energy that is created by piezo-ceramic elements. The vibrations (23-27 Hz) are transmitted through rigid probes, which results in a drilling action [17,18]. This lithotripter allows stone fragments to be simultaneously aspirated through the hollow probe, which helps to remove the stone particles. In particular, soft matrix stones such as phosphate-containing calculi can be readily suctioned out. Ultrasonic lithotripsy is very safe, because activating the probe when it is in contact with the urothelium results in only superficial erosion. However, ultrasound lithotripsy is somewhat less effective for very hard renal stones or for hard stones with a smooth surface [19]. In such cases, the lithotripter sometimes only succeeds in drilling deep holes into the stone without inducing any fragmentation. In addition, continuous irrigation is needed to prevent the probe from overheating. Notably, to prevent failure of an overheated device, the ultrasonic lithotripter must be started at a power mode between 1 and 2 (as recommended by the manufacturer), after which the power can be increased as needed up to 3 [20].
The ultrasound and pneumatic lithotripsy technologies have recently been combined to produce a single device. Compared with an ultrasonic device, the combined pneumatic and ultrasonic device is associated with significantly increased lithotripsy efficacy (stone disintegration) and efficiency (stone fragmentation and clearance) [21,22]. The main advantage of using an ultrasonic lithotripter in combination with a pneumatic lithotripter is that the fragmented stones can be cleared by active negative pressure suction. No other instruments are needed for the wholestone fragmenting and clearing process. Thus, there is no need to wash the nephroscope, which requires that it be repeatedly withdrawn from and then reinserted into the body. This reduces the intra- and postoperative complication rates, increases the stone-free rate, and shortens the operation time. Because negative pressure suction maintains the renal collection system at a low pressure, this also reduces the risk of bacterial infection. When considering the stone fragmentation efficacy of combined Lithoclast® and ultrasonic lithotripsy, Lithoclast® is more powerful for treating hard stones, whereas small fragments, granulation tissue-wrapped stones, impacted stones, and stones with a soft matrix (e.g., phosphate-containing calculi) are particularly suitable for aspiration through the ultrasound probe. Stone fragments can either be cleared out by forceps after crude fragmentation with the Lithoclast® or be flushed out through the hollow probe of the ultrasound lithotripter. In our study, the combination technique had a valuable synergistic effect.
In an actual clinical setting, the the combined use of these two instruments can maximize their advantages and minimize their disadvantages. Even in cases in which hard stones are present, for which fragmentation is difficult while bubbles are formed despite the use of ultrasonic lithotripsy, the surgical procedure can be performed both easily and safely. The stones can be fragmented to the appropriate size by using the power that a pneumatic lithotripter generates to a sufficient extent and the superior displacement of a stone or the occurrence of hemorrhagic events can be prevented by using the active negative suction of ultrasonic lithotripsy. Even in cases in which soft matrix stones are present and where the removal of stones is somewhat troublesome with a pneumatic lithotripter, the surgical procedure can be performed both easily and safely by using the active negative suction of ultrasonic lithotripsy. Compared with a single use of ultrasonic lithotripsy, any device malfunction (probe fracture, suction tubing obstruction) occurred at a lower frequency. Besides, even in cases in which hemorrhage occurred as a result of percutaneous access or tract dilation, an access could easily be made for the surgical field with use of the suction device with no necessity for removing the stones one by one with forceps.
The present study was limited by the fact that it was a retrospective, single-center study with a relatively small sample size (74 patients). In addition, the stones were not divided according to their composition into hard and soft stones. Although a device that combines ultrasonic lithotripsy with Lithoclast® has recently been invented, little was known in Korea about the benefits of combining these two lithotripsy technologies, which makes this study useful for actual Korean medical practice.
Disintegration of renal stones by use of pneumatic lithotripsy (Lithoclast®) alone or together with ultrasonic lithotripsy was found to be effective. The combination was associated with significant reductions in the operation time, hemoglobin loss, and hospital stay as compared with the use of Lithoclast® alone, and this was true regardless of the stones' composition. Thus, combining a pneumatic lithotripter with an ultrasonic lithotripter, which permits using the superior power of the Lithoclast® and enables the aspiration of debris during ultrasonic lithotripsy, is highly advantageous for treating renal calculi.
References
1. Fernström I, Johansson B. Percutaneous pyelolithotomy. A new extraction technique. Scand J Urol Nephrol. 1976. 10:257–259.
2. Marguet CG, Springhart WP, Tan YH, Patel A, Undre S, Albala DM, et al. Simultaneous combined use of flexible ureteroscopy and percutaneous nephrolithotomy to reduce the number of access tracts in the management of complex renal calculi. BJU Int. 2005. 96:1097–1100.
3. Begun FP. Modes of intracorporeal lithotripsy: ultrasound versus electrohydraulic lithotripsy versus laser lithotripsy. Semin Urol. 1994. 12:39–50.
4. Brannen GE, Bush WH, Correa RJ, Gibbons RP, Elder JS. Kidney stone removal: percutaneous versus surgical lithotomy. J Urol. 1985. 133:6–12.
5. Gupta R, Kumar A, Kapoor R, Srivastava A, Mandhani A. Prospective evaluation of safety and efficacy of the supracostal approach for percutaneous nephrolithotomy. BJU Int. 2002. 90:809–813.
6. Davidoff R, Bellman GC. Influence of technique of percutaneous tract creation on incidence of renal hemorrhage. J Urol. 1997. 157:1229–1231.
7. Park BH, Han YM, Kim YG. Comparison of the two-stage procedure with the one-stage procedure for percutaneous nephrolithotomy. Korean J Urol. 2006. 47:512–516.
8. Raney AM, Handler J. Electrohydraulic nephrolithotripsy. Urology. 1975. 6:439–442.
9. Hofbauer J, Höbarth K, Marberger M. Electrohydraulic versus pneumatic disintegration in the treatment of ureteral stones: a randomized, prospective trial. J Urol. 1995. 153:623–625.
10. Yiu MK, Liu PL, Yiu TF, Chan AY. Clinical experience with holmium:YAG laser lithotripsy of ureteral calculi. Lasers Surg Med. 1996. 19:103–106.
11. Jou YC, Shen CH, Cheng MC, Lin CT, Chen PC. High-power holmium:yttrium-aluminum-garnet laser for percutaneous treatment of large renal stones. Urology. 2007. 69:22–25.
12. Teichman JM, Vassar GJ, Bishoff JT, Bellman GC. Holmium:YAG lithotripsy yields smaller fragments than lithoclast, pulsed dye laser or electrohydraulic lithotripsy. J Urol. 1998. 159:17–23.
13. Michel MS, Honeck P, Alken P. New endourologic technology for simultaneous holmium:YAG laser lithotripsy and fragment evacuation for PCNL: ex-vivo comparison to standard ultrasonic lithotripsy. J Endourol. 2008. 22:1537–1539.
14. Piergiovanni M, Desgrandchamps F, Cochand-Priollet B, Janssen T, Colomer S, Teillac P, et al. Ureteral and bladder lesions after ballistic, ultrasonic, electrohydraulic, or laser lithotripsy. J Endourol. 1994. 8:293–299.
15. Hofmann R, Pickl U, Hartung R. The Lithoclast and Lithoclast Master - an experimental and clinical comparison. J Endourol. 1996. 10:S119.
16. Hofmann R, Pickl U, Schwarzer JU, Hartung R. Mechanical vs. laser lithotripsy for ureteral calculi. J Urol. 1994. 151:203A.
17. Begun FP. Modes of intracorporeal lithotripsy: ultrasound versus electrohydraulic lithotripsy versus laser lithotripsy. Semin Urol. 1994. 12:39–50.
18. Fuchs GJ. Ultrasonic lithotripsy in the ureter. Urol Clin North Am. 1988. 15:347–359.
19. Hofmann R, Olbert P, Weber J, Wille S, Varga Z. Clinical experience with a new ultrasonic and LithoClast combination for percutaneous litholapaxy. BJU Int. 2002. 90:16–19.
20. Lehman DS, Hruby GW, Phillips C, Venkatesh R, Best S, Monga M, et al. Prospective randomized comparison of a combined ultrasonic and pneumatic lithotrite with a standard ultrasonic lithotrite for percutaneous nephrolithotomy. J Endourol. 2008. 22:285–289.
21. Auge BK, Lallas CD, Pietrow PK, Zhong P, Preminger GM. In vitro comparison of standard ultrasound and pneumatic lithotrites with a new combination intracorporeal lithotripsy device. Urology. 2002. 60:28–32.
22. Hofmann R, Weber J, Heidenreich A, Varga Z, Olbert P. Experimental studies and first clinical experience with a new Lithoclast and ultrasound combination for lithotripsy. Eur Urol. 2002. 42:376–381.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download