Abstract
Purpose
The tension-free vaginal tape SECUR® (TVT-S) is a new, minimally invasive sling procedure for treating female stress urinary incontinence (SUI). However, results of comparisons of the TVT-S with the transobturator tape (TOT) sling are lacking. Therefore, we investigated outcome and satisfaction of the TVT-S procedure compared with the TOT procedure.
Materials and Methods
We included 64 patients with SUI who underwent the TVT-S (n=31) or TOT (MONARC®, n=33) procedure and were followed up for more than 1 year. The preoperative evaluation included history taking, pelvic examination, consecutive 3-day voiding diary, and urodynamic study including Valsalva leak point pressure. Postoperatively, continence status and subjective patient satisfaction were evaluated. Cure was defined as the absence of any episodes of involuntary urine leakage during stressful activities and a stress cough test.
Results
The TVT-S group (71.0%) showed a slightly lower cure rate than did the MONARC group (84.8%); however, there was no significant difference between the 2 groups (p=0.179). Nine of the patients who underwent the TVT-S showed incontinence postoperatively. Among them, the H approach was used in 7 patients and the U approach was done in 2 patients. Following TVT-S and MONARC, the patients' reported satisfaction was 80.6% and 78.8%, respectively. Patient satisfaction did not differ significantly between the two groups (p=0.854).
According to the International Continence Society (ICS), urinary incontinence is defined as cases in which social activities are impaired or hygiene problems are caused by involuntary urine leakage and there is an objective presence of the urine leakage [1]. Stress urinary incontinence (SUI) is the most common cause of female urinary incontinence, in which the urine leakage occurs involuntarily when the abdominal pressure is elevated and the bladder neck is opened. It results from hypermobility of the urethra and functional insufficiency of the urethral sphincter [2]. Recent epidemiological studies estimate that SUI affects 40% to 45% of Korean women [3,4]. At present, the most successful treatment for SUI is considered to be the midurethral sling.
Tension-free vaginal tape (TVT) is known to be a successful treatment for SUI. In 2001 Delorme used the 'outside-in' technique of a transobturator route for suburethral tape placement-the transobturator tape (TOT) [5,6]. This technique reduced the risk of bladder perforation and injuries to the bowels and large vessels compared with TVT. The cure rates of both procedures were similar, ranging from 90% to 95% [7].
Recently, tension-free vaginal tape-SECUR® (TVT-S) surgery, in which neither the retropubic space nor the transobturator route is passed, was introduced and the short-term results seem similar with conventional TOT. However, results for the efficacy and satisfaction of TVT-S are lacking in patients with more than 1-year of follow-up. Therefore, we compared outcome and satisfaction of the TOT (MONARC) and TVT-S procedures in women with SUI.
Of a total of 64 patients diagnosed with female SUI, 31 patients underwent TVT-S (TVT-Secur, Gynecare, Ethicon, Somerville, NJ, USA) and 33 underwent MONARC (outside-in, MONARC subfascial hammock, American Medical System) and were evaluated retrospectively in a nonrandomized manner. These patients were followed up for more than 12 months. The surgical approach of the TVT-S procedures was via the H approach, 51.6% (n=16), or via the U approach, 48.4% (n=15). Through preoperative physical examination and urodynamic studies, patients with neurogenic bladder, pelvic organ prolapse, suspected intrinsic sphincter deficiency, or past history of radical pelvic surgery were excluded.
Preoperatively, all patients underwent history taking, pelvic examination, consecutive 3-day voiding diary, and urodynamic study including Valsalva leak point pressure (VLPP). Surgery was performed by the same surgeon. Intra-operative cystoscopy was performed only for patients who underwent TVT-S via the U approach.
Following the postoperative period, urinary incontinence status and patient satisfaction were examined through an interview and physical examination in an outpatient setting. Cure was defined as the absence of any episodes of involuntary urine leakage during stressful activities and a stress cough test. Improvement was defined as a significant reduction in urine leakage, such that it did not require further treatment. The full bladder standing stress test by coughing was carried out to assess the cure rate. Satisfaction score was classified into three categories-'satisfied,' 'equivocal,' and 'unsatisfied'-on the basis of the patient's subjective symptoms more than 1 year after the operation.
Statistical analysis of the data was performed by using Student's t-test, chi-square test, and Fisher's exact test, for which SPSS ver. 13.0 (SPSS Inc., Chicago, IL, USA) was used. Statistical significance was set at p<0.05.
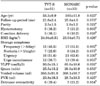
Mean age was 55.3±9.9 years (range, 43-85 years) in the TVT-S group and 58.5±11.8 years (range, 37-82 years) in the MONARC group (p=0.623). The mean follow-up period was 21.6 months (range, 18-25 months) in the TVT-S group and 25.8 months (range, 18-31 months) in the MONARC group (p=0.073). There were no significant differences in preoperative clinical findings between the two groups (Table 1).
The surgical cure rates were 71.0% (22/31) in the TVT-S group and 84.8% (28/33) in the MONARC group. Although the cure rate was slightly higher in the MONARC group, the difference between groups was not statistically significant (p=0.179) (Table 2). Following TVT-S and MONARC, the rates of patient satisfaction were 80.6% and 78.8% respectively. Patient satisfaction did not differ significantly between the two groups (p=0.854) (Table 2).
In the TVT-S group, cure rates were 56.3% (9/16) via the H-type approach and 86.7% (13/15) via the U-type approach. The cure rate of the U-type approach was higher than that of the H type, but not significantly so (p=0.070) (Table 3). Nine patients in the TVT-S group showed incontinence postoperatively. Among them, the H approach was used in 7 patients and the U approach was done in 2 patients. Five of these patients were found to be those who underwent TVT-S during the early experience of the surgeon. In the MONARC group, 5 patients showed incontinence postoperatively. Three of them showed improvement and 2 failed. Also, there were no significant complications related to TVT-S or MONARC.
Our study demonstrated that there was no significant difference in the cure rate or patient satisfaction between the TVT-S and MONARC procedures after more than 1 year of follow-up.
TVT and TOT are considered to be standard surgical treatments for SUI in women. The TOT procedure is easier than TVT, and it is therefore advantageous in that it can be easily learned, the surgical time and length of hospital stay are relatively shorter, and the long-term surgical outcomes are excellent. As a result, it has been widely used.
TVT-S was planned to reduce the invasiveness of the tape procedure by developing a new tape. The principal idea of this novel technique was to introduce a midurethral sling from a single incision without passing the retropubic space or the obturator foramen and its related nerves and vessels [8]. The TVT-S procedures utilize a shorter sling (8 cm) that is anchored directly to the retropubic fascia (U method) or the obturator internus muscle (H method). These steps lead to less dissection, lower amounts of synthetic material, and possibly fewer complications. Exit points are unnecessary, which reduces the immediate and persistent pain.
In a short-term follow-up of the TVT-S procedure, Martan et al reported a cure rate of 63% and an improvement rate of 26% at the 3-month follow-up in 85 patients [9]. Debodinance et al reported a cure rate of 70.4% at a 2-month follow-up in 110 patients [10].
We conducted a follow-up study for more than 1 year, according to which the TVT-S procedure showed efficacy and patient satisfaction similar to that of the MONARC procedure. Following the TVT-S procedure, the rate of treatment success was found to have a cure rate of 71% and an improvement rate of 19.3%. Following the MONARC procedure, the rate of surgical success was found to have a cure rate of 84.8% and an improvement rate of 9.1%. According to previous studies, TVT had a surgical success rate of 85% to 95% [7,11]. The TOT procedure had a surgical success rate of 91% including cure and improvement of symptoms after more than 1 year of follow-up [12]. Recently, many authors' results of a 1-year follow-up of TVT-S have shown cure rates of 78% to 88% [13-15], which agrees with our study of the TVT-S procedure.
In our study, the surgical cure rate was found to be slightly lower in the TVT-S group than in the MONARC group. The reason for the lower cure rate of the TVT-S procedure was as follows. The TVT-S involves a pull-back approach in which the inserter is withdrawn toward the vaginal incision. Therefore, unlike the retropubic TVT or the TOT approach, the mesh has a tendency to get looser during the final placement. A spacer is never placed for the TVT-S procedure. Also, in this study, the cure rate was lower for the same reasons during the early experience of the surgeon. Thus, unlike with TOT, special attention should be paid to ensure that the tension of the mesh is not loose.
In our study, patient satisfaction was 80.6% and 78.8% after TVT-S and MONARC, respectively. In association with this, Fischer et al reported that patient satisfaction with TOT was 90% after 1 year of follow-up [12]. Other authors reported that patient satisfaction with TVT-S was 76.4% to 80% after 1 year of follow-up [13,16], which agrees with this study of the TVT-S procedure.
According to Lee et al, the rate of surgical success with TVT-S showed no statistical significance (U type, 87.5%, vs. H type, 80.1%), but it was found to be relatively higher in the U type [13]. According to Meschia et al, however, the rate of surgical success with TVT-S showed no statistical significance (U type, 77%, vs. H type, 79%), but it was found to be slightly higher in the H type [14]. In this study, the cure rate of the U type was higher than that of the H type (U type, 86.7%, vs. H type, 56.3%), but the difference was statistically insignificant (p=0.070). One key step during the H approach is that the surgeon has to ensure that the TVT-S inserter has penetrated the obturator internus muscle. The anatomy of some patients may make it challenging to present the TVT-S inserter to the obturator internus muscle. If the mesh does not penetrate the internus, then it is likely to fail as it would then be wandering in the loose paravaginal fascial tissue without any strong anchor. Thus, it is important to follow the correct insertional angles so as to avoid placement in the loose space between the 12 o'clock and 3 o'clock positions. These factors may have affected our study's outcome.
Following the TVT procedure, complications such as hematoma formation, bladder perforation, intestinal injury, and vascular or nerve damage have occurred [17-19]. The TOT procedure was developed to reduce major complications such as bladder perforation and to eliminate the need for intra-operative cystoscopy. Compared with TVT, the incidence of complications is relatively lower [20]. However, according to previous studies, complications such as urethral or bladder perforation, vascular damage, and vaginal erosion are still reported [21,22]. According to another study, following the TVT-S procedure, complications such as vaginal wall perforation and urinary tract infection occurred [13,15,16]. In our study, however, no significant complications occurred after TVT-S or MONARC.
The limitation of the current study is that it was a retrospective, nonrandomized study and the number of patients was relatively small. Therefore, further large-scale, prospective studies are warranted.
After a follow-up period of over 1-year, the TVT-S and MONARC procedures were comparable in terms of the cure rate and patient satisfaction. Although the TVT-S procedures have a relatively lower cure rate than do current TVT or TOT procedures, efficacy can be improved with increasing proficiency. Studies are needed to establish further long-term and large-scale follow-up outcomes of the procedures.
Figures and Tables
References
1. Abrams P, Blaivas JG, Stanton SL, Andersen JT. The standardisation of terminology of lower urinary tract function. The International Continence Society Committee on Standardisation of Terminology. Scand J Urol Nephrol Suppl. 1988. 114:5–19.
2. Blaivas JG, Groutz A. Walsh PC, Retik AB, Vaughan ED, Wein AJ, editors. Urinary incontinence: pathophysiology, evaluation, treatment overview, and nonsurgical management. Campbell-Walsh urology. 2007. 9th ed. Philadelphia: Saunders;2046–2078.
3. Choo MS. Recent trends in the surgical treatment of female sterss urinary incontinence. Korean J Urol. 2004. 45:509–517.
4. Song HJ, Lee DH, Lee JY, Kim MJ. Epidemiologic study of urinary incontinence for Korean women over 30 years old. J Korean Continence Soc. 2001. 5:24–38.
5. Delorme E. Transobturator urethral suspension: mini-invasive procedure in the treatment of stress urinary incontinence in women. Prog Urol. 2001. 11:1306–1313.
6. Delorme E, Droupy S, de Tayrac R, Delmas V. Transobturator tape (Uratape): a new minimally-invasive procedure to treat female urinary incontinence. Eur Urol. 2004. 45:203–207.
7. Mellier G, Benayed B, Bretones S, Pasquier JC. Suburethral tape via the obturator route: is the TOT a simplification of the TVT? Int Urogynecol J Pelvic Floor Dysfunct. 2004. 15:227–232.
8. Neuman M. Perioperative complications and early follow-up with 100 TVT-SECUR procedures. J Minim Invasive Gynecol. 2008. 15:480–484.
9. Martan A, Svabík K, Masata J, Koleska T, El-Haddad R, Pavlikova M. Initial experience with a short, tension-free vaginal tape (the tension-free vaginal tape secur system). Eur J Obstet Gynecol Reprod Biol. 2009. 143:121–125.
10. Debodinance P, Lagrange E, Amblard J, Lenoble C, Lucot JP, Villet R, et al. TVT Secur: more and more minimally invasive. Preliminary prospective study of 110 cases. J Gynecol Obstet Biol Reprod (Paris). 2008. 37:229–236.
11. Kim WT, Kim KT, Kim JW, Choe JH, Lee JS, Seo JT. Comparative study of the tension-free vaginal tape (TVT) procedure and the suprapubic arc sling (SPARC) procedure for treating female stress urinary incontinence: a 1-year follow-up. Korean J Urol. 2006. 47:397–401.
12. Fischer A, Fink T, Zachmann S, Eickenbusch U. Comparison of retropubic and outside-in transobturator sling systems for the cure of female genuine stress urinary incontinence. Eur Urol. 2005. 48:799–804.
13. Lee KS, Lee YS, Seo JT, Na YG, Choo MS, Kim JC, et al. A prospective multicenter randomized comparative study between the U- and H-type methods of the TVT SECUR procedure for the treatment of female stress urinary incontinence: 1-year follow-up. Eur Urol. 2010. 57:973–979.
14. Meschia M, Barbacini P, Ambrogi V, Pifarotti P, Ricci L, Spreafico L. TVT-secur: a minimally invasive procedure for the treatment of primary stress urinary incontinence. One year data from a multi-centre prospective trial. Int Urogynecol J Pelvic Floor Dysfunct. 2009. 20:313–317.
15. Kim JJ, Lee YS, Lee KS. Randomized comparative study of the U- and H-type approaches of the TVT-Secur procedure for the treatment of female stress urinary incontinence: one-year follow-up. Korean J Urol. 2010. 51:250–256.
16. Jiménez Calvo J, Hualde Alfaro A, Raigoso Ortega O, Cebrian Lostal JL, Alvarez Bandres S, Jiménez Parra J, et al. Our experience with mini tapes (TVT Secur and MiniArc) in the surgery for stress urinary incontinence. Actas Urol Esp. 2008. 32:1013–1018.
17. Boustead GB. The tension-free vaginal tape for treating female stress urinary incontinence. BJU Int. 2002. 89:687–693.
18. Zilbert AW, Farrell SA. External iliac artery laceration during tension-free vaginal tape procedure. Int Urogynecol J Pelvic Floor Dysfunct. 2001. 12:141–143.
19. Amna MB, Randrianantenaina A, Michel F. Colic perforation as a complication of tension-free vaginal tape procedure. J Urol. 2003. 170:2387.
20. Seok NS, Suh HJ, Lee DH. Clinical outcome of transobturator Monarc procedures for treating of women with stress urinary incontinence: the 2-year follow-up. Korean J Urol. 2006. 47:835–840.
21. Minaglia S, Ozel B, Klutke C, Ballard C, Klutke J. Bladder injury during transobturator sling. Urology. 2004. 64:376–377.
22. Hermieu JF, Messas A, Delmas V, Ravery V, Dumonceau O, Boccon-Gibod L. Bladder injury after TVT transobturator. Prog Urol. 2003. 13:115–117.
This was a retrospective study of the results from two different sling surgeries in a single center. The authors compared the outcome and satisfaction of the MONARC and TVT-Secur procedures in the treatment of stress urinary incontinence. The conclusion of this article was that MONARC and TVT-Secur showed no significant differences in cure rate or patient satisfaction after a follow-up period of over 1 year. However, this study was performed in a retrospective, nonrandomized manner with a relatively small sample size compared with other comparative studies performed previously [1-3]. Therefore, it was inevitable that there was a limitation from weak statistical power in comparing the results of the two different surgical methods. The conclusion of this study of no significant differences between the two sling methods may be related to this relatively small sample size and weak statistical power. As the authors recommended, further long-term and large-scale follow-up of the procedures may lead to different conclusions.
References
1. Debodinance P. Trans-obturator urethral sling for the surgical correction of female stress urinary incontinence: outside-in (Monarc) versus inside-out (TVT-O). Are the two ways reassuring? Eur J Obstet Gynecol Reprod Biol. 2007. 133:232–238.
2. Laurikainen E, Valpas A, Kivela A, Kalliola T, Rinne K, Takala T, et al. Retropubic compared with transobturator tape placement in treatment of urinary incontinence: a randomized controlled trial. Obstet Gynecol. 2007. 109:4–11.
3. Lee KS, Lee YS, Seo JT, Na YG, Choo MS, Kim JC, et al. A prospective multicenter randomized comparative study between the U- and H-type methods of the TVT SECUR procedure for the treatment of female stress urinary incontinence: 1-year follow-up. Eur Urol. 2010. 57:973–979.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download