Abstract
Purpose
The most serious complication of suprapubic cystostomy is bowel injury. By computed tomography (CT), we investigated the risk factors of possible bowel interposition through the percutaneous suprapubic cystostomy tract.
Materials and Methods
From September to October 2009, we consecutively reviewed 795 abdominopelvic CT scans of adult patients performed for various reasons in our hospital. From these scans, we selected the films wherein the urinary bladder was distended more than 6 cm above the symphysis pubis. We then determined whether the bowel was interposed between the bladder and the skin at the routine puncture site of suprapubic cystostomy (the midline of the abdomen 3 cm above the upper margin of the symphysis pubis). We analyzed which factors influenced the possibility of the bowel being interposed between the bladder and the skin at the suprapubic puncture site.
Results
A total of 226 CT (148 males, 78 females) scans were selected. The mean patient age was 63 years (range, 26-84 years). The mean distance between the upper margin of the symphysis pubis and the umbilicus was 14.4 cm (range, 7.2-21.0 cm). In the multivariate analysis, obesity, a positive history of radical pelvic surgery, and a short distance (≤11 cm) between the symphysis pubis and the umbilicus had significant correlations with bowel interposition in the assumed tract.
Suprapubic cystostomies are performed for a variety of indications that require either temporary or permanent placement of suprapubic catheters [1]. The placement of percutaneous suprapubic catheters using a punch trocar technique involves some risks and should not be considered an innocuous procedure. Among the wide variety of complications, the most serious complication is bowel injury. Bowel injuries include perforation of the ileum [2-6] and colon [5] as well as small bowel obstruction and volvulus [3,7-9]. Because the percutaneous tract is blindly made at 3 to 4 cm above the symphysis pubis in the midline, the risk of bowel injury is constantly present. Therefore, before a percutaneous cystostomy is performed, especially if there has been prior abdominal or pelvic surgery, or if the bladder is not full, it is strongly advised to consider using ultrasound for the detection of interposed bowel along the percutaneous tract, because the bowel may be in close proximity to the tract [10]. However, that method does not totally guarantee the nonexistence of bowel crossing the tract, because it may be difficult for the ultrasound to detect a collapsed bowel. Despite this clinical setting, there has been little study of the risk factors for bowel injury associated with percutaneous cystostomy. This may be largely due to the practical limitations in demonstrating bowel injury before and after suprapubic cystostomy.
In this study, we investigated the risk factors for possible bowel interposition between the bladder and the skin at the routine puncture site of suprapubic cystostomy by computed tomography (CT), assuming that a hypothetical suprapubic cystostomy was performed.
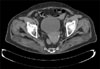
We retrospectively reviewed 795 consecutive adult abdominopelvic CT scans performed for various reasons in our hospital from September to October 2009. Among them, we selected 226 patients whose bladders were distended more than 6 cm above the upper margin of the symphysis pubis. Their medical charts at the time of the CT scan were analyzed retrospectively. Through the CT scan images, we determined whether the bowel was interposed between the urinary bladder and the skin at a point along the midline of the abdomen, 3 cm above the upper margin of the symphysis pubis (Fig. 1). This point is the routine suprapubic puncture site [11]. We investigated whether the age, gender, height, history of radical pelvic surgery, or the distance between the upper margin of the symphysis pubis and the umbilicus influenced the possibility of bowel interposition between the bladder and the skin at the suprapubic puncture site.
Statistical analyses were performed by applying the chi-square test and multiple logistic regression using commercially available software SPSS ver. 14.0 (SPSS Inc., Chicago, IL, USA). A p-value of <0.05 was considered statistically significant.
The patients' mean age was 63 years (range, 26-84 years). Among the 226 patients, 22 (9.7%) had undergone radical pelvic surgery previously. The mean distance between the upper margin of the symphysis pubis and the umbilicus was 14.4 cm (range, 7.2-21.0 cm) (Table 1).
The univariate analysis showed that sex (female, p=0.028), obesity (body mass index [BMI]≥25 kg/m2, p=0.006), a positive history of radical pelvic surgery (p<0.001), and a short distance (≤11 cm, p=0.016) between the upper margin of the symphysis pubis and the umbilicus were significantly correlated with bowel interposition at the routine suprapubic puncture site (Table 2). Among the 22 patients who had a radical pelvic operation, 20 had lower anterior resection, and the other 2 had segmental resection of the rectum due to rectal or colon cancer.
In the multivariate analysis, obesity (p=0.019), a positive history of pelvic surgery (p=0.001), and a short distance (p=0.016) between the upper margin of the symphysis pubis and the umbilicus were independent predictors for the bowel passing through the percutaneous tract (Table 3).
In our multivariate analysis, obesity, a history of pelvic surgery, and a short distance between the symphysis pubis and the umbilicus were independent predictors of bowel interposition through the percutaneous suprapubic cystostomy tract.
Prior pelvic surgery is a well known risk factor for bowel injury after percutaneous cystostomy. After a pelvic operation, the bowel can move downward through the opened space of Retzius, and associated postoperative adhesions may develop between the anterior abdominal wall and peritoneum, both of which may increase the probability of bowel injury during a suprapubic cystostomy procedure. In our study, 9 of the 22 patients (40.9%) who had radical pelvic surgery had an interposed bowel at the routine suprapubic cystostomy tract, whereas 17 of the 204 (8.3%) without a history of pelvic surgery had bowel interposition. All of the prior pelvic surgeries were opened lower anterior resections because of rectal or colon cancer.
Obesity has also been considered as a risk factor for bowel injury when performing a suprapubic cystostomy because it is difficult to localize the bladder in such patients [12]. Our study presented the novel hypothesis that obesity itself is an independent predictor for bowel interposition through the cystostomy tract. We do not know the exact reason for the above finding, but assumed that because obese patients have relatively larger bowel contents as well as omental fat, the bowel tended to move downward in the limited intra-abdominal space. Similarly, the correlation of bowel interposition with a short distance between the symphysis pubis and the umbilicus can be understood in the same manner.
As we mentioned above, 8.3% of the patients without a history of pelvic surgery had interposition of the bowel through the routine cystostomy tract. This was much higher than the general consensus, because the placement of a suprapubic tube for urinary diversion is generally an uneventful procedure. For the safe placement of a suprapubic catheter, the most important point is the full distension of the urinary bladder before the procedure. In this study, we considered bladder distension more than 6 cm above the upper margin of the symphysis pubis as a cutoff point on the basis of data from voiding cystourethrograms performed in 20 adult patients with neuropathic bladder. In their films, the average distance between the symphysis pubis and the upper margin of the cystogram at full bladder distension was 6.2 cm. We therefore defined 6 cm as the assumptive point of full bladder distension. Because a fully distended bladder in a normal patient without neuropathic bladder can rise more than 6 cm above the symphysis pubis, it seemed likely that our results overdetected the bowel interposition through the cystostomy tract. However, we should take into consideration that, clinically, the complications of suprapubic cystostomy are commonly seen in small capacity bladder with neuropathic deficits [1]. In the practical setting, although a small capacity bladder itself would be the major risk factor for complications in performing suprapubic cystostomy, the retrospective nature of our study could not reveal that relationship. The high exclusion rate (71.6%) was another major pitfall of this study, because patients who underwent abdominopelvic CT scan were not instructed to endure the urge to urinate.
To our knowledge, this is the first study that attempted to reveal the risk factors of possible bowel injury related to suprapubic cystostomy, even though the study was performed by an indirect approach. This study may offer useful information to practitioners who perform suprapubic cystostomies.
This study demonstrated the risk factors for the bowel being interposed at the routine suprapubic puncture site as detected by CT scan. When performing a suprapubic cystostomy, extreme caution is needed to avoid possible bowel injury in patients who are obese, who have had previous radical pelvic operations, and who have a short distance (≤11 cm) between the upper margin of the symphysis pubis and the umbilicus.
Figures and Tables
FIG. 1
Computed tomography scan showing the bowel interposed between the urinary bladder and the skin at a point along the midline of the abdomen, 3 cm above the upper margin of the symphysis pubis.
References
1. Dogra PN, Goel R. Complication of percutaneous suprapubic cystostomy. Int Urol Nephrol. 2004. 36:343–344.
2. Flock WD, Litvak AS, McRoberts JW. Evaluation of closed suprapubic cystostomy. Urology. 1978. 11:40–42.
3. Hebert DB, Mitchell GW Jr. Perforation of the ileum as a complication of suprapubic catheterization. Obstet Gynecol. 1983. 62:662–664.
4. Moody TE, Howards SS, Schneider JA, Rudolf LE. Intestinal obstruction: a complication of percutaneous cystostomy. A case report. J Urol. 1977. 118:680.
5. Browning DJ. Potential hazard of suprapubic catheterization. Med J Aust. 1977. 2:580.
6. Drutz HP, Khosid HI. Complications with Bonanno suprapubic catheters. Am J Obstet Gynecol. 1984. 149:685–686.
7. Simpson RR. An unusual cause of small bowel obstruction: the misplaced suprapubic catheter. J Urol. 2001. 165:1998.
8. Lin AC, Wu CC, Wang TL, Chang H. An unusual cause of volvulus: the misplaced suprapubic catheter. J Emerg Med. 2005. 28:219–220.
9. Liau SS, Shabeer UA. Laparoscopic management of cecal injury from a misplaced percutaneous suprapubic cystostomy. Surg Laparosc Endosc Percutan Tech. 2005. 15:378–379.
10. Ballentine HC, David YC. Wein AJ, Kavoussi LR, Novick AC, Partin AW, Peters CA, editors. Basic instrumentation and cystoscopy. Campbell-Walsh urology. 2007. 9th ed. Philadelphia: Saunders;161–170.
11. Engel WJ. Suprapubic trocar cystostomy: an evaluation and presentation of an improved instrument. J Urol. 1951. 65:998–1005.
12. Alagiri M, Seidmon EJ. Percutaneous endoscopic cystostomy for bladder localization and exact placement of a suprapubic tube. J Urol. 1998. 159:963–964.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download