Abstract
We report a rare case of robot-assisted laparoscopic radical prostatectomy (RARP) in a patient with a preexisting penile prosthesis. In this case, we completed RARP without removing the reservoir by using a deflation-inflation technique, and there were no complications related to the prosthesis. The patient had a negative surgical margin. The preserved three-piece inflatable penile prosthesis continued to function properly in 1 month. Reservoir-preserving RARP is technically feasible and safe. However, it is important to be aware of device-related complications. Long-term studies on the mechanical survival rate and patient satisfaction should be also performed.
Prostate cancer has been reported to occur most frequently in men over 40 years of age. In organ-confined cases, radical prostatectomy is the treatment of choice. After the introduction of the da Vinci® surgical system (Intuitive Surgical, Sunnyvale, USA), robot-assisted laparoscopic radical prostatectomy (RARP) has become a mainstay of treatment for prostate cancer in Korea [1]. In similar age groups, men also tend to experience sexual dysfunction, including erectile dysfunction (ED). In patients with ED, surgical treatments like penile prosthesis implantation are considered when behavior therapy and medications are not effective. For these reasons, prostate cancer patients who have undergone penile prosthesis implantation could be candidates for RARP. The three-piece inflatable penile prosthesis (IPP) comprises three components: a balloon-like reservoir, a flow-regulating pump, and a pair of cylinders. The reservoir can be injured during prostatectomy and can also hinder RARP because it is placed in the perivesical space. However, few RARP cases involving patients with a preexisting three-piece IPP have been reported, and similar situations are likely to occur more frequently as the number of operations increases. Therefore, we report our experience with RARP in a patient with a three-piece IPP that had been implanted in a previous surgery.
The patient was a 64-year-old male diagnosed with acinar-type prostate adenocarcinoma with a Gleason score of 6 (3+3) by prostate biopsy. His prostate volume was 25 g, and his prostate-specific antigen (PSA) was 2.34 ng/ml. The patient had undergone a three-piece IPP (AMS-700CX, American Medical Systems, USA) implantation 15 years previously because of diabetic erectile dysfunction. The 60 ml reservoir was placed in the left retropubic space through an external inguinal ring from a penoscrotal vertical incision. All devices worked well. Because we perform magnetic resonance imaging in all prostate cancer patients preoperatively (Fig. 1), the surgeon who performed this case was fully aware of the anatomical structure of the patient before surgery. The patient was informed in advance of the risks of malfunction, infection, and the possibility of IPP removal.
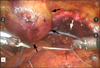
The RARP was done in the usual manner [2]. Initially, all six ports were placed after the pneumoperitoneum was established with a Veress needle. A 12 mm Visiport was placed at the umbilicus for the camera. The 8 mm ports for the robotic arms were placed laterally below the level of the umbilicus. In addition, a 12 mm assistant port was inserted between the camera port and the outer robot port and the suction cannula was put through a 5 mm port between the camera and robotic port ipsilateral to the assistant's side. In this case, the inflated reservoir was easily found in the lateral pelvic wall. We carefully dissected the encapsulated reservoir by electrocautery (monopolar curved scissor) so as not to injure it. After separating the reservoir capsule, deflation was performed on the pelvic wall to empty the reservoir, creating more prevesical space. There were no adhesions in the pelvic cavities (Fig. 2). Then, RARP was successfully performed [2]. After finishing the urethrovesical anastomosis with an 18Fr silicone Foley catheter and placing a drain, we inflated the reservoir (Fig. 3).
The operating time was 120 min, and the estimated blood loss during the surgery was 320 ml. There was no damage to the adjacent organs. The encapsulated reservoir was well inflated and was easily separated from the surrounding tissues. Reservoir change was not suspected. Pathologic examination revealed acinar type adenocarcinoma and the Gleason score was 6 (3+3). The tumor volume was 1.50 cc, and the surgical margin was negative. The length of hospital stay was 9 days. The drain was removed on day 4, and the urethral catheter was removed on day 9. The preserved IPP continued to function properly in 1 month. No other complications were reported. The 6-month follow-up PSA level was <0.01 ng/ml and the patient achieved pad-free status.
There have been some reports previously about prostatectomy performed on patients with a preexisting IPP, but not many [3-5]. Davis et al reported a case with infectious complications related to the IPP [3]. The deflation-inflation technique adopted for our patient was a technically smooth and feasible approach and there were neither complications nor mechanical malfunctions. This technique can be easily performed by a bedside assistant surgeon. Moreover, the procedure did not affect oncologic outcome and demonstrated the benefits of not having to undergo an additional operation. We considered the view of the operation field to be the most important factor during surgery. If deflation and retraction to the pelvic wall are incomplete, the reservoir has to be removed. Because the reservoir was located in the operation field, ipsilateral robotic arm movement is limited, which could make it difficult to perform RARP. There was also a risk of injuring the reservoir by the robotic arm. Actually, one of our prostate cancer patients requested the removal of the reservoir before RARP because he feared intraoperative and postoperative complications. In the present case, however, the patient underwent the RARP without removal of the reservoir. Previous studies did not report any perioperative complications, especially in robotic cases [5]. However, prosthesis-related infection and malfunction should be considered when performing this surgery [3,4,6,7]. Careful dissection around the peri-reservoir tissue and preservation of the pseudocapsules are the keys in this procedure. Infection can occur once the reservoir and connector tubes are contaminated by urine or irrigation fluid [2,8]. To prevent tearing of the pseudocapsule, we used a monopolar cutting current to dissect the encapsulated tissues and avoided directly grasping the reservoir [5]. When the implant was exposed, primary closure of the pseudocapsule and an above-average dose of long-term intravenous antibiotics were needed. When deflation and dissection were performed, the reservoir became fully mobile. During the healing period, the reservoir can become dislocated from its original place. Munoz et al reported a case with an intravesical reservoir that caused the initial symptoms accompanied by an IPP implantation, such as urinary tract infection and incontinence [9]. Leach et al also discussed a case in which the reservoir eroded into the bowel and bladder [10]. Sometimes, a dislocated reservoir can compress the ureter and cause hydronephrosis. For these reasons, we should keep in mind the complications that follow reservoir shifting if a patient complains of atypical urinary symptoms, hydronephrosis, or changes in bowel habits postoperatively. To fix the reservoir in the intended place, the urethral catheter should be removed as soon as possible because a distended bladder can help to push the movable reservoir superiorly and laterally [7]. Mireku-Boateng et al reported that they usually remove the urethral catheter at a mean time of postoperative day 12 [7]. In our case, the urethral catheter was removed earlier (on day 9) than in other studies. In our case, IPP had been performed through a penoscrotal incision so that we could avoid surrounding tissue adhesion and reservoir fixation. In our experience, organ-confined prostate cancer patients with a history of IPP implantation through penoscrotal incisions may be good candidates for reservoir-saving RARP. After performing the deflation-inflation technique for the RARP patient with a preexisting penile prosthetic reservoir, it appeared that this technique was feasible, safe, and cost-effective. However, it is important to be aware of device-related complications. Long-term studies on the mechanical survival rate and patient satisfaction should be also performed.
Figures and Tables
References
1. Park SY, Ham WS, Choi YD, Rha KH. Robot-assisted laparoscopic radical prostatectomy: clinical experience of 200 cases. Korean J Urol. 2008. 49:215–220.
2. Menon M, Hemal AK. Vattikuti Institute prostatectomy: a technique of robotic radical prostatectomy: experience in more than 1000 cases. J Endourol. 2004. 18:611–619.
3. Davis BE, DeBrock BJ, Lierz MF, Weigel JW. Management of preexisting inflatable penile prosthesis during radical retropubic prostatectomy. J Urol. 1992. 148:1198–1200.
4. Dunsmuir WD, Kirby RS. Conservation of inflatable penile prosthesis during radical retropubic prostatectomy. Br J Urol. 1997. 79:283–284.
5. Rehman J, Guru K, Chughtai B, Shabsigh R, Samadi D. Robotic radical prostatectomy in patients with preexisting inflatable penile prosthesis (IPP). Can J Urol. 2008. 15:4263–4265.
6. Tiguert R, Hurley PM, Gheiler EL, Tefilli MV, Gudziak MR, Dhabuwala CB, et al. Treatment outcome after radical prostatectomy is not adversely affected by a pre-existing penile prosthesis. Urology. 1998. 52:1030–1033.
7. Mireku-Boateng AO, Oben F. Surgical outcome of radical retropubic prostatectomy is not adversely affected by preexisting three-piece inflatable penile implant. Urol Int. 2005. 74:221–223.
8. Yang KM, Choi HK. Analysis of survival rate and cause of revision in penile prosthesis: a single center long term follow-up study. Korean J Urol. 2005. 46:1186–1191.
9. Munoz JJ, Ellsworth PI. The retained penile prosthesis reservoir: a risk. Urology. 2000. 55:949.
10. Leach GE, Shapiro CE, Hadley R, Raz S. Erosion of inflatable penile prosthesis reservoir into bladder and bowel. J Urol. 1984. 131:1177–1178.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download