Abstract
Purpose
The aim of this study was to describe the surgical clip-related complications that can occur after open retropubic prostatectomy (RRP), pure laparoscopic prostatectomy (LRP), and robot-assisted laparoscopic radical prostatectomy (RALP).
Materials and Methods
A database of 641 patients who underwent RRP (n=439), LRP (n=49), and RALP (n=153) at our institution between January 2006 and April 2009 was reviewed to identify patients with complications related to the use of surgical clips. The median follow-up time for the entire cohort was 19.0 months (range, 1-42 months).
Results
Of the 641 patients, 25 (5.7%), 1 (2.0%), and 2 (1.3%) had a bladder neck contracture after RRP, LRP, and RALP, respectively. Two RRP patients had a bladder stone. In total, 6 patients had surgical clip-related complications. Metal clip migration was associated with 2 (8%) of the 25 RRP cases of bladder neck contracture and both (100%) of the RRP cases of bladder stone. Moreover, both (100%) of the RALP cases of bladder neck contractures were associated with Hem-o-lok clip migration into the anastomotic site.
Conclusions
Surgical clips are prone to migration and may cause, or significantly contribute to, bladder neck contracture or the formation of bladder stones after radical prostatectomy. These findings also suggest that because the incidence of bladder neck contracture after RALP is low, the migration of Hem-o-lok clips should be suspected when voiding difficulty occurs after RALP.
Bladder neck contracture (BNC) is a complication of radical prostatectomy. The estimated incidence of BNC after open retropubic radical prostatectomy (RRP) ranges from 3% to 26% [1-8]. Robot-assisted laparoscopic radical prostatectomy (RALP) is becoming a more frequently performed procedure because it clearly has a lower rate of postoperative complications than RRP. In particular, the incidence of BNC after RALP ranges from 0.6% to 3% [9-12]. The reason for this lower incidence is unclear.
Several case reports have suggested that RRP, pure laparoscopic radical prostatectomy (LRP), and RALP are associated with complications related to the use of surgical clips, including BNC and the formation of bladder stones [13-19]. The purpose of this study was to evaluate the surgical clip-related complications that occurred after RRP, LRP, and RALP in our institution.
In our institution, RRP was the method of choice for radical prostatectomy until August 2005, when the first case of LRP was performed. Thereafter, LRP was frequently performed between August 2005 and April 2008. From May 2008, we began to conduct RALP. We retrospectively reviewed a database that has been maintained in our institution of the clinical, surgical, and pathological parameters of these procedures. Approval for the study was obtained from the institutional review board. We reviewed a total of 641 cases who underwent radical prostatectomy at our institution between January 2006 and April 2009.
Of the 641 patients, 439, 49, and 153 underwent RRP, LRP, and RALP, respectively. In all cases, the procedures were uneventful and proceeded in the usual fashion without complications. The median follow-up time for the entire cohort was 19.0 months (range, 1-42 months). Of the RRP, LRP, and RALP patients, 25 (5.7%), 1 (2.0%), and 2 (1.3%) had BNC, respectively, and 2 of the RRP patients developed a bladder stone. In total, 6 patients with complications related to the use of surgical clips were identified in the cohort.
The characteristics of these 6 patients are summarized in Table 1. All 6 patients had obstructive lower urinary tract symptoms after surgery. Cystoscopic examination of patient 1 revealed a metal clip within the BNC scar tissue. Urethral dilatation and transurethral incision were performed, but the symptoms recurred rapidly. This patient currently requires serial intermittent urethral dilatations. Cystoscopic examination of patient 2 indicated BNC and the presence of a metal clip protruding into the urethra through the urethrovesical anastomosis at 4 o'clock (Fig. 1). This patient responded to dilatation. Patients 3 and 4 were both found to have a Hem-o-lok clip in the bladder neck (Fig. 2). Their BNCs were resolved after a single urethral dilatation, after which the symptoms disappeared. Patients 5 and 6 were found to have a bladder stone that had formed around the metal clip in the bladder (Fig. 3). Transurethral holmium laser lithotripsy was performed. Retrospective re-evaluation of the kidney, ureter and bladder X-ray (KUB) revealed the metal clip in the bladder region (patient 5: Fig. 4). During the follow-up, neither patient exhibited signs of bladder stone recurrence. In all patients, the offending surgical clip was easily removed by using a grasping forceps.
The etiology of BNC is poorly understood. One study based on a patient self-reported questionnaire, which revealed that 25.9% of RRP patients reported at least one episode of BNC that required treatment, was unable to identify factors that could predict the occurrence of BNC [2]. In contrast, Surya et al reported that many factors promote the occurrence of BNC after RRP, including urinary extravasation, excessive blood loss, and previous bladder neck surgery [1]. Similarly, Thiel et al found that 17.5% of RRP patients required stricture dilatation by a mean time of 6 months after surgery and revealed that increased age and increased blood loss were statistically associated with stricture formation [6]. Recently, Erickson et al suggested that improved surgical technique and increased surgeon experience appear to be the most important factors that reduce the incidence of BNC [8]. Huang and Lepor added a history of previous transurethral resection of the prostate, pelvic external beam radiotherapy, and a hypertrophic healing response to the risk factors for BNC after RRP [5]. Another study found that of the 11.1% of patients who developed BNC after RRP, the biggest risk factor was current smoking (26%), with comorbidities such as hypertension, coronary artery disease, and diabetes also being significantly associated with the formation of BNC. The investigators hypothesized that local ischemia of the urethra and bladder neck caused by microvascular disease may lead to poor anastomotic healing and scar formation [3].
Msezane et al reported that the incidence of BNC after RALP was 1.1% [12]. Similarly, the incidence of BNC in our cohort of 153 consecutive RALP patients was 1.3%. It is not clear why the rate of BNC after RALP is significantly lower than that quoted in the RRP literature, but Msezane et al suggested that it may be due to the running anastomosis, better visualization, improved instrument maneuverability, and decreased blood loss [12]. Moreover, a comprehensive review of the literature comparing RRP, LRP, and RALP revealed that higher estimated blood loss was a significant factor in the development of BNC [20]. Recently, a study comparing RRP and RALP suggested that the predisposing causes of BNC are likely to be the combination of a fixed circular bladder stomatization with the subsequent healing of the stoma anastomosis to the urethra [21].
The present study shows that BNC may also arise as a result of clip migration. This has also been observed in the literature (Table 2), although it should be noted that most reported complications with surgical clips relate to hemorrhage. Long et al reported the first case of metal clip migration-induced BNC after RRP in a patient who had suffered multiple episodes of urinary retention and had undergone several failed urethrotomies [14]. Later, Blumenthal et al reported the first case report of Hem-o-lok migration into the vesicourethral anastomosis after RALP [16]. Those authors believe that the relationship between surgical clip migration into the anastomosis and BNC formation is not coincidental; they postulated that the physical disruption of the anastomosis by the surgical clip contributed to poor healing and may have elicited an inflammatory reaction. Tunnard et al then described a case of a Hem-o-lok clip-related complication following LRP: during bladder neck dilatation for a tight bladder neck, a Hem-o-lok was found in the bladder, having migrated from the urethrovesical anastomosis [18]. It was removed successfully but a repeat cystoscopy 3 months later revealed another Hem-o-lok device that had eroded through the vesicourethral anastomosis. This was removed successfully with the aid of a holmium laser.
In the present study, stones developed around the surgical clip in 2 patients after RRP. Other studies have also reported surgical clip-related complications other than BNC (Table 2). These include the case described by Palou et al of severe perineal pain after RRP due to the protrusion of a metal clip into the urethra at the urethrovesical anastomosis, and the case of Banks et al, in which the migration of a Hem-o-lok clip into the bladder led to stone formation after LRP [13,15]. There was also a recent report by Kadekawa et al of a case in which a metal clip had migrated into the urinary bladder after RRP [17]. It was hypothesized that inflammation had arisen around the urinary bladder or vesicourethral anastomosis and that this also involved the metal clip, which then eroded the bladder wall and eventually migrated into the bladder. In addition, Mora et al reported a case of intravesical migration and subsequent calculus formation with the spontaneous expulsion of a Hem-o-lok clip after LRP [19]. These findings suggest that foreign bodies in the bladder can act as a nidus for bladder stone formation owing to the presence of persistent chronic inflammation.
The mechanism underlying the migration of a surgical clip into the urinary tract is unclear. In our series, the rate of BNC after RALP was significantly lower than that after RRP. However, potential limitations of the current study should be considered. The current series was sequential. Because improvements in outcomes are related to temporal improvements in particular procedures, this trend might account for some improvement in outcome in the RALP group.
It appears that surgical clips are prone to migration and may cause, or significantly contribute to, BNC or the formation of bladder stones after radical prostatectomy. These findings raise questions regarding the use of foreign bodies in close proximity to the vesicourethral anastomosis during radical prostatectomy. At the very least, they indicate that care must be taken with the surgical clips used for inducing hemostasis near the apex of the prostate in radical prostatectomy. In addition, because the incidence of BNC after RALP is low, when unexplained voiding difficulty occurs after RALP, one should suspect that a Hem-o-lok clip has migrated, especially because Hem-o-lok clips cannot be detected on X-rays.
Figures and Tables
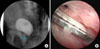 | FIG. 1(A) Lateral view of cystography: a surgical metal clip can be seen in contact with the urethra (arrow). (B) Cystoscopic evidence of clip-induced erosion. |
TABLE 2
Summary of reports of surgical clip-related complications after radical prostatectomy

RRP: open retropubic radical prostatectomy, AUR: acute urinary retention, BNC: bladder neck contracture, LRP: laparoscopic radical prostatectomy, RALP: robot-assisted laparoscopic radical prostatectomy, LUTS: lower urinary tract symptoms, KTP: potassium-titanyl-phosphate, TUI: transurethral incision
References
1. Surya BV, Provet J, Johanson KE, Brown J. Anastomotic strictures following radical prostatectomy: risk factors and management. J Urol. 1990. 143:755–758.
2. Moul JW, Mooneyhan RM, Kao TC, McLeod DG, Cruess DF. Preoperative and operative factors to predict incontinence, impotence and stricture after radical prostatectomy. Prostate Cancer Prostatic Dis. 1998. 1:242–249.
3. Borboroglu PG, Sands JP, Roberts JL, Amling CL. Risk factors for vesicourethral anastomotic stricture after radical prostatectomy. Urology. 2000. 56:96–100.
4. Besarani D, Amoroso P, Kirby R. Bladder neck contracture after radical retropubic prostatectomy. BJU Int. 2004. 94:1245–1247.
5. Huang G, Lepor H. Factors predisposing to the development of anastomotic strictures in a single-surgeon series of radical retropubic prostatectomies. BJU Int. 2006. 97:255–258.
6. Thiel DD, Igel TC, Brisson TE, Heckman MG. Outcomes with an alternative anastomotic technique after radical retropubic prostatectomy: 10-year experience. Urology. 2006. 68:132–136.
7. Elliott SP, Meng MV, Elkin EP, McAninch JW, Duchane J, Carroll PR. Incidence of urethral stricture after primary treatment of prostate cancer: data from CaPSURE. J Urol. 2007. 178:529–534.
8. Erickson BA, Meeks JJ, Roehl KA, Gonzalez CM, Catalona WJ. Bladder neck contracture after retropubic radical prostatectomy: incidence and risk factors from a large single-surgeon experience. BJU Int. 2009. 104:1615–1619.
9. Menon M, Tewari A, Peabody JO, Shrivastava A, Kaul S, Bhandari A, et al. Vattikuti Institute prostatectomy, a technique of robotic radical prostatectomy for management of localized carcinoma of the prostate: experience of over 1100 cases. Urol Clin North Am. 2004. 31:701–717.
10. Patel VR, Tully AS, Holmes R, Lindsay J. Robotic radical prostatectomy in the community setting--the learning curve and beyond: initial 200 cases. J Urol. 2005. 174:269–272.
11. Shalhav AL, Orvieto MA, Chien GW, Mikhail AA, Zagaja GP, Zorn KC. Minimizing knot tying during reconstructive laparoscopic urology. Urology. 2006. 68:508–513.
12. Msezane LP, Reynolds WS, Gofrit ON, Shalhav AL, Zagaja GP, Zorn KC. Bladder neck contracture after robot-assisted laparoscopic radical prostatectomy: evaluation of incidence and risk factors and impact on urinary function. J Endourol. 2008. 22:377–383.
13. Palou J, Alberola JM, Villavicencio H, Vicente J. It's like a pain in the ... perineum: a surgical clip protruding into the urethra through the urethrovesical anastomosis after radical prostatectomy. Scand J Urol Nephrol. 1997. 31:493–495.
14. Long B, Bou S, Bruyere F, Lanson Y. Vesicourethral anastomotic stricture after radical prostatectomy secondary to migration of a metal clip. Prog Urol. 2006. 16:384–385.
15. Banks EB, Ramani A, Monga M. Intravesical Weck clip migration after laparoscopic radical prostatectomy. Urology. 2008. 71:351.
16. Blumenthal KB, Sutherland DE, Wagner KR, Frazier HA, Engel JD. Bladder neck contractures related to the use of Hem-o-Lok clips in robot-assisted laparoscopic radical prostatectomy. Urology. 2008. 72:158–161.
17. Kadekawa K, Hossain RZ, Nishijima S, Miyazato M, Hokama S, Oshiro Y, et al. Migration of a metal clip into the urinary bladder. Urol Res. 2009. 37:117–119.
18. Tunnard GJ, Biyani CS. An unusual complication of a Hem-o-Lok clip following laparoscopic radical prostatectomy. J Laparoendosc Adv Surg Tech A. 2009. 19:649–651.
19. Mora ER, Gali OB, Garin JA, Arango O. Intravesical migration and spontaneous expulsion of a Hem-o-lok polymer ligating clip after laparoscopic radical prostatectomy. Urology. 2010. 75:1317.
20. El-Hakim A, Leung RA, Tewari A. Robotic prostatectomy: a pooled analysis of published literature. Expert Rev Anticancer Ther. 2006. 6:11–20.
21. Webb DR, Sethi K, Gee K. An analysis of the causes of bladder neck contracture after open and robot-assisted laparoscopic radical prostatectomy. BJU Int. 2009. 103:957–963.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download