Abstract
Purpose
The aim of this study was to investigate the effect of transurethral resection of the prostate (TURP) on erectile function.
Materials and Methods
A total of 108 patients treated with TURP were retrospectively evaluated. All patients were evaluated 1, 3, and 6 months after TURP by use of the International Prostate Symptom Score (IPSS), International Index of Erectile Function (IIEF), peak urinary flow rate (Qmax), and post-void residual urine (PVR).
Results
One and 3 months after TURP, the erectile function domain score of the IIEF was significantly decreased. However, after 6 months, there was no longer a significant decrease in the erectile function domain score. The change in erectile function was compared with the IPSS score. There was no statistically significant correlation, but patients who had better voiding symptoms after TURP had improved erectile function.
Benign prostatic hyperplasia (BPH) is commonly seen in elderly men starting at 40 years of age. BPH often presents as lower urinary tract symptoms (LUTS) due to difficulties in voiding and irritability of the bladder. Transurethral resection of the prostate (TURP) has been considered the reference treatment for BPH for the past 30 years [1]. However, TURP, the standard surgical therapy for the relief of LUTS, is reported to cause erectile dysfunction (ED), although some patients with preexisting ED reported improved erectile function after TURP. Thus, recent evidence from both community and clinical trials has suggested a link between BPH-induced LUTS and erectile function [2].
The aim of this study was to evaluate erectile function after TURP in a hospital by use of the validated International Index of Erectile Function (IIEF) [3]. A second aim was to identify the possible factors associated with the occurrence of ED in this particular patient cohort.
Between January 2008 and August 2009, 108 patients who underwent TURP were retrospectively evaluated. All patients also underwent transrectal ultrasound (TRUS, B&K Medical, Herlev, Denmark). In addition, medical history, prostate-specific antigen (PSA), flow rate, urine residue, and International Prostate Symptom Score (IPSS) were recorded for those who presented without a catheter. Finally, the erectile function of the patient was evaluated according to the IIEF questionnaire. The flow rate, IPSS, and IIEF questionnaire were reevaluated at 1, 3, and 6 months postoperatively.
Monopolar TURP was performed by the same urologist. As much prostate adenomatous tissue as possible was removed as far as the surgical capsule. A 22 French resectoscope with a continuous irrigation system was used. An 18 French Foley catheter was inserted in all patients and was removed when hematuria sufficiently diminished. After removal of the catheter 2-5 days after the operation, a voiding trial was performed. If it was successful, the patient was discharged.
We used the IIEF score, which was calculated 1 month before the operation and 1, 3, and 6 months after the operation, to compare the change in erectile function. All domains included in the IIEF were compared with the IPSS and other items. Because the patients in this study had generally decreased sexual activities, there was a limited correlation between erectile function itself and satisfaction or orgasm. For this reason, the study focused on the EF domain of the IIEF. Because the range that divided the total score for the EF domain was 5 points, we divided the patients into 3 groups and defined them as follows: patients who had less than 5 points were defined as the impaired erectile function group, those who had more than 5 points were defined as the improved erectile function group, and those between the two groups mentioned above were defined as the no influence on erectile function group (The data that we compared were the EF domain questionnaire completed before the operation and that completed 6 months after the operation.). We also divided the patients into three groups and analyzed their characteristics. The first group consisted of patients who had erectile function before the operation but had no erectile function after the operation. The second group were those who had no erectile function before the operation but recovered erectile function after the operation. Finally, the third group were those who did not show any change in erectile function before or after TURP.
We analyzed the data with the Statistical Package for the Social Sciences 16.0 for Windows (SPSS Inc., Chicago, IL, USA). Comparisons of clinical characteristics and parameters were made by using the paired t-test and chi-square test. The comparative analysis between the three groups was performed by using ANOVA. For all statistical comparisons, significance was considered at p<0.05.
A total of 29 patients were excluded from the analysis, including 3 who were diagnosed with prostate carcinoma after surgery, 3 who had a urethral stricture after transurethral prostatic resection and underwent urethrotomy, and 23 who refused to complete the erectile function questionnaire. The patient characteristics are listed in Table 1. The mean patient age was 67.5 years (range, 55-80 years), the average amount of resected tissue was 26.5 g (range, 5-82 g), and the mean resection time was 64 minutes (range, 22-115 minutes). Histopathological examination revealed BPH in all patients.
Before and 6 months after TURP, the mean residual urine volume was reduced from 105.1±126.0 ml to 46.0±33.3 ml (p<0.01). The maximum flow rate improved from 10.1±5.4 ml/s to 15.5±8.7 ml/s (p<0.01). The mean IPSS score decreased from 18.7±8.6 to 7.8±8.1 (p<0.01). As shown in the table, the patients' symptoms improved greatly after TURP (Table 2).
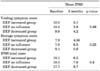
In the analysis at 1 and 3 months after TURP, the EF domain score was significantly decreased (p<0.04, p<0.03). Six months later, however, there was no longer a statistically significant decrease in the postoperative EF domain score compared with the preoperative EF domain score (p<0.08) (Table 3).
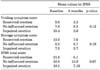
Nine patients had erectile function before the operation but had full ED after the operation (11%), and 6 patients had full ED before the operation but recovered erection after the operation (8%). A total of 12 patients (14%) had an increased EF domain score after the operation, and 23 patients (28%) had a decreased EF domain score after operation. There were no significant differences between the two groups for any compared items. Intraoperative capsular perforation occurred in 18 (21%) patients. Capsular perforation had no significant difference in the two groups (p<0.64, p<0.09). Interestingly, however, the recovered erectile function group show a more decreased IPSS-related score than did the full ED group after TURP: total IPSS score, -15.7 vs. -10.0 (p<0.1); voiding symptom score, -7.5 vs. -6.6 (p<0.2) (Table 4).
The increased EF domain score group had a more decreased IPSS-related score than did the decreased EF domain score group: total IPSS score, -11.6 vs. -9.0 (p<0.40); voiding symptom score, -7.1 vs. -5.4 (p<0.32) (Table 5). Capsular perforation was not significantly different (p<0.88).
BPH is a common condition in elderly men and is associated with a range of erectile function. Because ED also has a high prevalence in elderly men, many groups have assessed whether any causal relationship exists between BPH and erectile function [4]. Treatments for BPH are also associated with erectile function. But the effect of TURP on erectile function is still controversial, and the available evidence is conflicting. Erection is a complex phenomenon that involves neurological, hormonal, arterial, venous, and muscular components and that is further influenced by psychogenic, cognitive, and environmental factors [5,6]. The effect of TURP on erectile function may be brought about via several different routes, including the psychogenic effect of an invasive procedure in the genital region, injury to the nerve tracts supplying the corpus cavernosum as a result of electrocoagulation, thrombosis of the cavernosal arteries, venous leakage, and injury to the nerve tracts [7,8].
In fact, there are many reports of impaired erectile function after TURP. Many studies have reported that ED after TURP occurs in between 4% and 35% of patients and that it is associated with age or pre-existing ED [9-12]. Until now, no conclusive determination has been made. Most studies have reported only on the incidence of de novo ED after TURP and not on the proportion of patients experiencing an improvement of erectile function [10,11].
According to the results of our study, TURP does not affect the erectile function of the patient. Patients could be affected negatively as a result of worrying about the invasive procedure. Furthermore, patients could be affected by feeling pain during erection as the result of injury to the urethra. As time goes by, however, these problems are solved, and the change can most likely be attributed to improvement in the quality of urination. The survey showed that when patients experienced difficulty of urination caused by BPH, they preferred to avoid suffering from this condition by ceasing to pursue sex. Subsequently, their libido remained comparatively low. After TURP, their mental stress was released, their libido became normal, and the patients felt that their erectile ability improved.
Several authors have reported that capsular perforation is a potential risk factor for developing erectile dysfunction after TURP [13,14]. However, in our study, capsular perforation had no significant correlation with erectile function. We think that ED related to capsular perforation may depend on the location, depth, and extent of the perforation.
Most studies have reported only on the incidence of ED after TURP. Our study showed that there was a significant decrease in erectile function for 3 months after TURP. However, no significant change in erectile function was observed after 6 months. Although no significant correlation was detected, one interesting result was improved erectile function in the patients who had better voiding symptoms after TURP.
Figures and Tables
TABLE 3
Mean EF domain score on the IIEF at baseline and at 1, 3, and 6 months in patients undergoing transurethral prostatectomy

References
1. Wasson JH, Reda DJ, Bruskewitz RC, Elinson J, Keller AM, Henderson WG. The Veterans Affairs Cooperative Study Group on Transurethral Resection of the Prostate. A comparison of transurethral surgery with watchful waiting for moderate symptoms of benign prostatic hyperplasia. N Engl J Med. 1995. 332:75–79.
2. Cha JS, Park JK. Association between lower urinary tract symptoms and erectile dysfunction. Korean J Urol. 2005. 46:1023–1027.
3. Ahn TY, Lee DS, Kang W, Hong JH, Kim YS. Validation of an abridged Korean version of the International Index of Erectile Function (IIEF-5) as a diagnostic tool for erectile dysfunction. Korean J Urol. 2001. 42:535–540.
4. Sairam K, Kulinskaya E, McNicholas TA, Boustead GB, Hanbury DC. Sildenafil influences lower urinary tract symptoms. BJU Int. 2002. 90:836–839.
5. Feldman HA, Goldstein I, Hatzichristou DG, Krane RJ, McKinlay JB. Impotence and its medical and psychosocial correlates: results of the Massachusetts Male Aging Study. J Urol. 1994. 151:54–61.
6. Ledda A. Cigarette smoking, hypertension and erectile dysfunction. Curr Med Res Opin. 2000. 16:Suppl 1. S13–S16.
7. Lue TF, Tanagho EA. Physiology of erection and pharmacological management of impotence. J Urol. 1987. 137:829–836.
8. Hanbury DC, Sethia KK. Erectile function following transurethral prostatectomy. Br J Urol. 1995. 75:12–13.
9. Lindner A, Golomb J, Korczak D, Keller T, Siegel Y. Effects of prostatectomy on sexual function. Urology. 1991. 38:26–28.
10. Soderdahl DW, Knight RW, Hansberry KL. Erectile dysfunction following transurethral resection of the prostate. J Urol. 1996. 156:1354–1356.
11. Taher A. Erectile dysfunction after transurethral resection of the prostate: incidence and risk factors. World J Urol. 2004. 22:457–460.
12. Miner M, Rosenberg MT, Perelman MA. Treatment of lower urinary tract symptoms in benign prostatic hyperplasia and its impact on sexual function. Clin Ther. 2006. 28:13–25.
13. Poulakis V, Ferakis N, Witzsch U, de Vries R, Becht E. Erectile dysfunction after transurethral prostatectomy for lower urinary tract symptoms: results from a center with over 500 patients. Asian J Androl. 2006. 8:69–74.
14. Oh SY, Min KS, Choi SH. Effects of prostate volume and lower urinary tract symptoms on erectile function. Korean J Urol. 2007. 48:24–28.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download