Abstract
Purpose
Radical cystectomy has been the most widely used method in the treatment of bladder cancer, but it is limited by major problems. Therefore, we investigated the results of bladder-preserving treatment in patients with T3b, T4a, and T4b transitional carcinoma of the bladder who underwent transurethral resection of bladder cancer and subsequent administration of chemotherapy.
Materials and Methods
Of all patients who were diagnosed with bladder cancer and underwent bladder-preserving treatment between January 2001 and August 2008, 78 patients with at least 12 months of follow-up data were enrolled in this study. All patients received gemcitabine (1,000 mg/m2) and cisplatin (70 mg/m2) once per month postoperatively for a total of 6 months and completed a follow-up visit every 3 months. The patient survival rate and prognostic factors (age, tumor size, differentiation, number of lesions, stage, and presence of hydronephrosis) were assessed. The Kaplan-Meier method was used to analyze survival rate, and Cox multiple regression analysis was used for prognostic factors.
Results
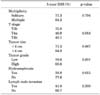
The mean patient age was 68.32±8.6 years, the mean duration of follow-up was 54.70±32.8 months, and the median duration of follow-up was 49.0 months. The 5-year survival rate was 66.2%. Single lesions were found in 28 cases (35.9%), and multiple lesions were found in 50 cases (64.1%). Stage T3b lesions were identified in 56 cases (71.8%), stage T4a lesions were identified in 16 cases (20.5%), and stage T4b lesions were identified in 6 cases (7.7%). Tumor size was less than 4 cm in 4 cases (59.0%) and greater than 4 cm in 32 (41.0%). Hydronephrosis was present in 21 cases (26.9%). In the 5-year survival analysis, prognostic factors significantly influencing survival rate were T-stage of the tumor and absence of hydronephrosis and complete regression after treatment (p<0.05). Multivariate analysis revealed that tumor stage and the absence of hydronephrosis were statistically significant prognostic indicators.
Conclusions
In patients with T3b, T4a, and T4b transitional carcinoma of the bladder, bladder preservation may prevent a decrease in quality of life. Also, our findings suggest that this approach could be considered a primary treatment option for patients with T3b stage tumors without evidence of hydronephrosis.
Current treatment options for muscle-invasive bladder cancer include radical cystectomy, chemotherapy, and radiotherapy. Recently, in an attempt to preserve the bladder - thereby reducing the likelihood of a decreased quality of life postoperatively - the combination of transurethral resection of the bladder cancer followed by chemotherapy and/or radiotherapy has been studied.
Cystectomy has been the treatment of choice for muscle-invasive bladder cancer confined to the organ, and recent improvements in surgical techniques have led to decreased rates of complications and mortality following surgery. In particular, the development of organ-preserving surgical procedures has changed the treatment strategies for a variety of tumors; therefore, the previous standard treatments are being replaced by organ-preserving procedures. Over the years, patients have become more aware of the complications and decreased quality of life that often follow radical cystectomy and are now more insistent upon preserving the bladder. Therefore, chemotherapy following transurethral resection of a bladder tumor is gaining more attention in the treatment of bladder cancer.
Recent studies on bladder-preserving therapy in muscle-invasive bladder cancer by Solsona, Herr, and Shipley showed a 5-year survival of 80% and a bladder preservation rate of 67-82%, which are highly successful outcomes [1-3]. Therefore, it can be expected that appropriately selected patients with muscle-invasive bladder cancer treated with a combination of transurethral resection of the bladder tumor and chemotherapy could experience outcomes similar to those in patients treated with radical cystectomy.
In this study, we analyzed the prognostic factors affecting the outcomes of T3b, T4a, and T4b transitional carcinoma of the bladder treated by transurethral resection of the bladder tumor and chemotherapy. Overall, the purpose of this study was to evaluate alternative efficacy, prognostic factors, and usefulness of bladder preservation treatment by analyzing the 5-year survival rate and the treatment's long-term outcomes through follow-up observations on the patient group.
A total of 78 patients from our institution who were diagnosed with T3b, T4a, and T4b transitional carcinoma of the bladder and who underwent transurethral resection of the bladder tumor and chemotherapy were enrolled in this retrospective study. To be included in the study, a patient had to meet the following criteria: 1) be diagnosed with T3b, T4a, or T4b transitional carcinoma of the bladder at our institution from January 2001 to August 2008, 2) have undergone transurethral resection of the bladder tumor and be followed up for at least 12 months, 3) complete each chemotherapy session, 4) patients with one of the above-mentioned stages but for whom surgery was not an option because of accompanying medical illnesses, 5) patients having problems of postoperative male sexual dysfunction and urinary incontinence or discomfort with urinary diversion, 6) patients of an old age, and 7) patients who rejected radical cystectomy as a treatment plan. Except for those cases who experienced progression of the tumor during chemotherapy, making advancement of the treatment impossible, repeat transurethral resection of the bladder cancer was performed in patients with recurrence.
Clinical staging of the bladder cancer was done by using cystoscopy, computed tomography (CT), bone scan, and simple chest X-ray. The stages were assigned by using the TNM staging system proposed by the AJCC. Patients with urethral or pelvic tumors were excluded. Currently, because Korea's medical insurance allows gemcitabine use in patients with stage T3b or above, patients at or above that stage were selected whether there was lymph node or distant metastasis.
All patients had a serum creatinine concentration of less than 2.0 mg/ml, a 24-hour creatinine clearance rate of at least 50 mg/min, normal erythropoietic function (WBC≥4,000/mm3, platelet≥100,000/mm3), and normal liver function (AST/ALT<40 U/l). The patients' performance status was between 0 and 2 on the basis of the ECOG, and each patient's bladder tumor was removed to the maximum extent allowed by transurethral resection. Four weeks after transurethral resection of the bladder cancer, chemotherapy was initiated. The chemotherapy regimen included gemcitabine (1,000 mg/m2) and cisplatin (70 mg/m2) per month for 6 months. Specifically, each session consisted of intravenous gemcitabine and cisplatin at the beginning of the month, followed by a week of rest, two weeks of intravenous gemcitabine, and another week of rest.
A pelvic CT scan and bone scan were performed every 3 months to evaluate the patient's response to the therapy, and after completion of the 6-month chemotherapy regimen, transurethral cystoscopy, a bladder cytology study, and a pelvic CT scan were performed every 2 to 3 months for 2 years to monitor for recurrence. Since then, the above tests were repeated every 6 month for 3 years; thereafter, follow-up was performed every 1 year.
Age, tumor size, degree of differentiation, number of tumor sites, staging, and the presence of hydronephrosis were selected as potential prognostic factors and were included in the analysis. The patients were declared cured of the tumor when no recurrence occurred. In the case of patients who died during follow-up, the relationship between recurrence and/or progression of the tumor and the direct cause of death was studied.
Both univariate and multivariate analyses were performed to determine whether any of the prognostic factors were significantly associated with outcomes after surgery. Factors were determined to be statistically significant if the p-value was less than 0.05. Survival data were analyzed by using the Kaplan-Meier method and log-rank test. To run statistical analysis, SPSS for Windows version 17 was used.
Six monthly chemotherapeutic sessions were scheduled for a total of 6 months after resection of the tumor. A total of 45 patients (58%) received 6 sessions, 23 (29%) received 2 to 5 sessions, and 10 (13%) received 7 to 12 sessions. The mean patient age was 68.32±8.6 years; the mean duration of follow-up was 54.70±32.8 months, and the median duration of follow-up was 49.0 months. A total of 28 patients 35.9%) had a solitary lesion, and 50 (64.1%) had multiple lesions. A total of 56 cases (71.8%) were classified as stage T3b, 16 (20.5%) were classified as stage T4a, and 6 (7.7%) were classified as stage T4b. A total of 46 patients (59.0%) had tumors that were less than 4 cm in size, and 32 (41.0%) had tumors that were 4 cm in size or greater. On pathology, all lesions were classified as urothelial carcinoma; 21 patients (26.9%) had hydronephrosis, 15 patients (19.2%) had lymph node invasion, 12 patients (15.4%) had distant metastasis, and 39 patients (50%) had received repeat transurethral resection of bladder cancer (Table 1).
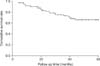
The average 5-year survival rate of the patients was 66.2% (Fig. 1). Univariate analysis showed that T-stage of the tumor, absence of hydronephrosis, and completion of the chemotherapy regimen were significantly associated with increased survival (Table 2). Multivariate analysis using Cox proportional hazards model showed that high tumor stage and presence of hydronephrosis were significant prognostic indicators of decreased survival (Table 3, Fig. 2, 3).
Complications were experienced by most patients and included alopecia, nausea, vomiting, and loss of appetite. Complications such as leukopenia, arising from long-term myelosuppression, worsened as time passed; however, administration of granulocyte colony-stimulating factor (G-CSF) often improved the condition.
The treatment of muscle-invasive bladder cancer can be divided into radical and bladder-preserving therapies, and the former is currently considered the standard of care. There are alternatives for patients who do not want to undergo radical cystectomy, for reasons such as complications from the surgery and post-surgical decrease in quality of life, as well as for patients in whom radical cystectomy is contraindicated. However, issues such as delayed initial treatment, potential cystectomy in the future, and current chemotherapeutic treatment can delay or prohibit performance of the surgery and, therefore, cannot be ignored. Furthermore, selecting appropriate patients for bladder-preserving procedures can be difficult [4,5].
Cisplatin-based combination chemotherapy has been reported to be more effective than single-drug regimens; therefore, since the 1980s, a combination of transurethral resection of the bladder tumor and cisplatin-based combination chemotherapy or radiotherapy has been used. In our study, the mean duration of follow-up was 51.9 months following transurethral resection of the bladder tumor and adjuvant chemotherapy, and our patient population showed a 5-year survival rate of 66.2%, which is not significantly different from the survival rate of similar patients who undergo radical cystectomy. This means that transurethral resection of low-staged muscle-invasive bladder cancer without hydronephrosis followed by chemotherapy may be equally as efficacious as more radical therapy (e.g., radical cystectomy).
Accordingly, in the early 1990s, Hashine, Mori, and others studied a combination therapy that included intra-arterial cisplatin-based chemotherapy in patients with low-stage muscle-invasive bladder cancer, reporting an improved 5-year survival rate of 78% to 85% [6,7].
Urinary incontinence is the most problematic complication affecting the quality of life in patients following radical cystectomy. The incidence rate is reported to be 70% to 95% during the day and 65% to 85% at night. However, most patients are willing to accept this complication as an often unavoidable result of complete removal of their tumor [4,5,8]. Complications of radiotherapy include bladder contraction (0-2%) and decreased bladder volume (9%) [9]. In addition, Zietman reported that development of erectile dysfunction and dissatisfaction with sexual life occurred in 54% and 59% of patients, respectively, who underwent radical cystectomy [10]. These complications are often significant, and it is therefore important to consider these factors when choosing the treatment modality for a patient with muscle-invasive bladder cancer.
During chemotherapy after bladder-preserving surgery, chemotherapy-induced myelosuppression-causing leukopenia is the most serious complication, and, for some patients, this complication is significant enough to compel them to forego completion of their chemotherapy and may even lead to death in some cases. However, most of the time, administration of G-CSF can reverse these negative effects of chemotherapy. Less serious complications, such as alopecia, decreased renal function, oral infection, nausea, vomiting, and loss of appetite, disappeared in most patients when they were off the therapy (i.e., during rest periods). Disadvantages are under-staging after transurethral resection of bladder cancer, no definite patient selection criteria, pain incurred during regularly scheduled cystoscopy, discomfort and costs of the radiologic tests and chemotherapy, inconvenience of repeat transurethral resection of bladder cancer in recurred cases, and follow-up losses during the therapy.
Complete transurethral tumor resection by a proficient urologist, complete remission induced by chemotherapy, and exact staging of the cancer through analysis of radiologic studies all play important roles in improving the efficacy of bladder-preserving therapy [11]. These factors need to be taken into consideration when choosing the appropriate treatment modality for a patient with bladder cancer. De la Rosa et al found multiple statistically significant positive prognostic indicators of survival in patients with bladder cancer: a tumor size less than 4 cm, a tumor with a low degree of differentiation, the presence of carcinoma in situ, and good response to chemotherapy [12]. Furthermore, Herr followed up 99 out of 432 patients who initially underwent repeated transurethral resection for muscle-invasive bladder tumors for 10 years and discovered that 34% of the patients experienced tumor recurrence [2]. Other potential prognostic factors, both clinical and pathologic, have been studied, and biochemical and genetic factors, such as Bcl-2 and P53, are expected to provide additional information regarding prognosis.
Our study showed that low-stage bladder cancer without hydronephrosis can be completely cured by complete transurethral resection of the bladder tumor with adjuvant chemotherapy. Even in the case of muscle-invasive cancer, a combination of transurethral resection and chemotherapy can safely be performed as long as the tumor is of a low stage and is limited to the lamina muscularis. Bladder-preserving therapy can help to prevent psychological stress and excessive treatment caused by radical cystectomy while improving patients' quality of life and promoting normal urination and satisfactory sexual activity. Thus, in addition to being an effective treatment modality, transurethral resection affords many additional benefits to the patient. Also, it must be remembered that regular follow-up to monitor for and to treat any recurrence is vital to maximizing patient survival.
In order to more definitively evaluate the efficacy, benefits, and drawbacks of bladder-preserving surgery, a prospective, randomized study with long-term follow up, comparing the outcomes of radical cystectomy versus transurethral resection of a bladder tumor, will be required.
This study followed 78 patients diagnosed with muscle-invasive bladder cancer who underwent transurethral resection of the bladder tumor. Their 5-year survival rate was 66.2%, which is comparable to that of radical cystectomy. Prognostic factors associated with decreased survival include a high-stage tumor and the presence of hydronephrosis. For patients with low-stage tumors and no hydronephrosis, bladder-preserving therapy may be a potential treatment option that offers not only a survival benefit found similarly in more radical therapies, but also an improved quality of life after surgery.
Figures and Tables
References
1. Solsona E, Iborra I, Ricos JV, Monros JL, Casanova J, Calabuig C. Feasibility of transurethral resection for muscle infiltrating carcinoma of the bladder: long-term followup of a prospective study. J Urol. 1998. 159:95–98.
2. Herr HW. Transurethral resection of muscle-invasive bladder cancer: 10-year outcome. J Clin Oncol. 2001. 19:89–93.
3. Shipley WU, Kaufman DS, Zehr E, Heney NM, Lane SC, Thakral HK, et al. Selective bladder preservation by combined modality protocol treatment: long-term outcomes of 190 patients with invasive bladder cancer. Urology. 2002. 60:62–67.
4. Mottet N, Castagnola C, Rischmann P, Deixonne M, Guyot M, Coloby P, et al. Quality of life after cystectomy: French national survey conducted by the French Association of Urology (AFU), the French Federation of Stoma Patients (FSF) and the French Association of Enterostomy Patients (AFET) in patients with ileal conduit urinary diversion or orthotopic neobladder. Prog Urol. 2008. 18:292–298.
5. Hart S, Skinner EC, Meyerowitz BE, Boyd S, Lieskovsky G, Skinner DG. Quality of life after radical cystectomy for bladder cancer in patients with an ileal conduit, cutaneous or urethral kock pouch. J Urol. 1999. 162:77–81.
6. Hashine K, Kusuhara Y, Miura N, Shirato A, Sumiyoshi Y, Kataoka M. Bladder preservation therapy conducted by intra-arterial chemotherapy and radiotherapy for muscle invasive bladder cancer. Jpn J Clin Oncol. 2009. 39:381–386.
7. Mori K, Nomata K, Noguchi M, Eguchi J, Hayashi N, Kanetake H. Long-term follow up of patients with invasive bladder carcinoma receiving combined cisplatin-based intra-arterial chemotherapy and radiotherapy. Int J Urol. 2007. 14:591–594.
8. Cookson MS. The surgical management of muscle invasive bladder cancer: a contemporary review. Semin Radiat Oncol. 2005. 15:10–18.
9. Rödel C, Weiss C, Sauer R. Trimodality treatment and selective organ preservation for bladder cancer. J Clin Oncol. 2006. 24:5536–5544.
10. Zietman AL, Sacco D, Skowronski U, Gomery P, Kaufman DS, Clark JA, et al. Organ conservation in invasive bladder cancer by transurethral resection, chemotherapy and radiation: results of a urodynamic and quality of life study on long-term survivors. J Urol. 2003. 170:1772–1776.
11. Sabaa MA, El-Gamal OM, Abo-Elenen M, Khanam A. Combined modality treatment with bladder preservation for muscle invasive bladder cancer. Urol Oncol. 2010. 28:14–20.
12. de la Rosa F, Garcia--Carbonero R, Passas J, Rosino A, Lianes P, Paz-Ares L. Primary cisplatin, methotrexate and vinblastine chemotheraphy with selective bladder preservation for muscle invasive carcinoma of the bladder: long-term followup of a prospective study. J Urol. 2002. 167:2413–2418.
This article is a retrospective study of bladder-preservation therapy for muscle-invasive bladder cancer (MIBC), especially T3b and above. Non-muscle-invasive bladder cancer (NMIBC), in fact, makes up of 80% of newly diagnosed bladder cancer, and approximately 20% is MIBC. Furthermore, 20% to 30% of recurred NMIBC becomes invasive and possibly metastatic [1]. For MIBC, radical cystectomy (RC) has been the gold standard of treatment with good cancer-specific survival and overall survival [2-4]. But, radical surgery on the bladder is accompanied by functional deterioration of continence and sexual behavior [5]. This functional deterioration is directly associated with the quality of life of bladder cancer patients after RC, and for this reason, many MIBC patients are unwilling to undergo RC. For many decades, although many physicians have tried to lower the complications and mortality associated with RC, the complication rate and perioperative rate has been as high as 17% to 32% and 2% to 3%, respectively [2]. Of course, in treating bladder cancer, survival is the first thing to be considered and it is true that survival is higher than in any other condition. But because the quality of life of the patients should not be overlooked, bladder-preservation therapy has been studied by many physicians for several decades.
Including this study, many studies have reported the efficacy of bladder-preservation therapy [combined chemotherapy and radiotherapy (RT) following vigorous transurethral resection of the bladder tumor (TURBT)], which has comparable 5-year survival and overall survival [6-9]. But no studies have made direct comparisons between the two therapies. Because of this, it is difficult to clarify whether to pay more for good results between RC and bladder-preservation therapy. What is more, in the studies of the North American Radiation Therapy Oncology Group (RTOG) [10] and Massachusetts General Hospital [11], large numbers of patients who underwent bladder-preservation therapy eventually required RC (45% and 34%, respectively).
To successfully conduct bladder-preservation therapy, first, observant and careful patient selection should be made, and vigorous TURBT should be performed until no visible tumor is seen. RT with concomitant radiosensitizing platinum-based chemotherapy should be accompanied in turns, with evaluation of response and prompt salvage RC for nonresponders. Last, long-term follow-up of patients should be done [12].
In conclusion, the study of bladder-preservation therapy is ongoing, rather than conclusive. After the accumulation of more such studies, a clear choice will be possible for bladder-preservation therapy of MIBC.
References
1. Kuczyk M, Turkeri L, Hammerer P, Ravery V. Is there a role for bladder preserving strategies in the treatment of muscle-invasive bladder cancer? Eur Urol. 2003. 44:57–64.
2. Stein JP, Lieskovsky G, Cote R, Groshen S, Feng AC, Boyd S, et al. Radical cystectomy in the treatment of invasive bladder cancer: long-term results in 1,054 patients. J Clin Oncol. 2001. 19:666–675.
3. Dalbagni G, Genega E, Hashibe M, Zhang ZF, Russo P, Herr H, et al. Cystectomy for bladder cancer: a contemporary series. J Urol. 2001. 165:1111–1116.
4. Ghoneim MA, Abdel-Latif M, el-Mekresh M, Abol-Enein H, Mosbah A, Ashamallah A, et al. Radical cystectomy for carcinoma of the bladder: 2,720 consecutive cases 5 years later. J Urol. 2008. 180:121–127.
5. World Health Organization (WHO) Consensus Conference on Bladder Cancer. Hautmann RE, Abol-Enein H, Hafez K, Haro I, Mansson W, et al. Urinary diversion. Urology. 2007. 69:1 Suppl. 17–49.
6. Given RW, Parsons JT, McCarley D, Wajsman Z. Bladder-sparing multimodality treatment of muscle-invasive bladder cancer: a five-year follow-up. Urology. 1995. 46:499–504.
7. Shipley WU, Kaufman DS, Zehr E, Heney NM, Lane SC, Thakral HK, et al. Selective bladder preservation by combined modality protocol treatment: long-term outcomes of 190 patients with invasive bladder cancer. Urology. 2002. 60:62–67.
8. de la Rosa F, Garcia-Carbonero R, Passas J, Rosino A, Lianes P, Paz-Ares L. Primary cisplatin, methotrexate and vinblastine chemotherapy with selective bladder preservation for muscle invasive carcinoma of the bladder: long-term followup of a prospective study. J Urol. 2002. 167:2413–2418.
9. Park KK, Song JM. Bladder preservation management for muscle invasive bladder cancer. Korean J Urol. 2004. 45:19–23.
10. Shipley WU, Zietman AL, Kaufman DS, Althausen AF, Heney NM. Invasive bladder cancer: treatment strategies using transurethral surgery, chemotherapy and radiation therapy with selection for bladder conservation. Int J Radiat Oncol Biol Phys. 1997. 39:937–943.
11. Shipley WU, Kaufman DS, Tester WJ, Pilepich MV, Sandler HM. Overview of bladder cancer trials in the Radiation Therapy Oncology Group. Cancer. 2003. 97:8 Suppl. 2115–2119.
12. Yafi FA, Cury FL, Kassouf W. Organ-sparing strategies in the management of invasive bladder cancer. Expert Rev Anticancer Ther. 2009. 9:1765–1775.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download