Abstract
A 26-year-old man presented with lower abdominal discomfort and a palpable mass in the right lower quadrant. An abdominal computed tomography (CT) scan revealed an abdominal wall mass that extended from the dome of the bladder. Fluorine-18 fluorodeoxyglucose (FDG) positron-emission tomography/CT (PET/CT) showed hypermetabolic wall thickening around the bladder dome area that extended to the abdominal wall and hypermetabolic mesenteric infiltration. Differential diagnosis included a urachal tumor with invasion into adjacent organs and chronic inflammatory disease. Partial cystectomy with abdominal wall mass excision was performed, and the final pathologic report was consistent with urachal actinomycosis.
Urachal actinomycosis is an uncommon disease that has rarely been reported [1-3]. It is a chronic suppurative inflammatory disease caused mainly by Actinomyces israelii. We report a case of urachal actinomycosis that presented as lower abdominal pain and a palpable mass mimicking a urachal tumor.
A 26-year-old man presented to our outpatient clinic with complaints of lower abdominal discomfort and a palpable mass in the right lower quadrant. The patient had no remarkable past, familial, or personal history. The abdomen examination revealed a 6 cm palpable mass without tenderness in the right lower quadrant. Routine urine analysis revealed pyuria of 10-19 white blood cell (WBC)/high-power field (HPF) and microscopic hematuria of 5-9 red blood cell (RBC)/HPF. No organism was cultured from the urine, and urine cytology showed benign cells.
Chest and abdomen X-ray findings were within normal limits. Abdominal ultrasonography revealed irregular wall thickening of the bladder dome with extension to the abdominal wall. An abdominal computed tomography (CT) scan revealed an abdominal wall mass that extended from the bladder dome and irregular perivesical infiltration, suggesting urachal remnant-associated disease (Fig. 1). A cystoscopic biopsy that had been performed before the operation revealed chronic inflammation. Additional fluorine-18 fluorodeoxyglucose (FDG) positron-emission tomography (PET)/CT was performed to rule out a urachal tumor. The PET/CT showed hypermetabolic bladder wall thickening with mesenteric and omental infiltration, extending along the urachus (Fig. 2). Partial cystectomy with resection of the abdominal wall mass was performed because malignancy could not be ruled out completely. The mass contained necrotic lesions with yellowish foci in the deep resection margin and the final pathology was consistent with Actinomyces israelii with sulfur granules (Fig. 3).
The patient underwent treatment with oral fluoroquinolone for 3 months and recovered without complications.
Actinomycosis shows chronic, indolent, and recurrent clinical courses [4]. The most common sites involved are the cervicofacial, abdominal, and thoracic region [5]. The appendix and cecum are the most commonly affected abdominal organs [6]. Actinomyces israelii invades and penetrates the intestinal mucosa and bowel wall, producing localized or extended peritoneal and retroperitoneal abscess formation. Actinomyces israelii is a commensal organism within the oral cavity, alimentary tract, and vagina and spreads by direct extension. It produces multiple abscesses, resulting in necrosis and fibrosis [7]. Abdominal actinomycosis has no specific symptoms. It usually presents with a palpable mass, weight loss, and anorexia [7]. Definite diagnosis can be made by demonstration of Actinomyces israelii in a needle or surgical biopsy specimen.
The general PET/CT finding of actinomycosis is intense hypermetabolism as in malignancy [8]. Hypermetabolic changes at the bladder dome and urachus on PET/CT made the diagnosis very elusive in this case. Because there is not much difference in the PET/CT findings between malignancy and actinomycosis, utilization of PET/CT to rule out malignancy does not seem to be necessary, unless the case is strongly suggestive of malignancy.
We performed a partial cystectomy to clarify this elusive disease entity and confirmed Actinomyces israelii colonies in the specimen. Medical treatment for actinomycosis is antibiotic therapy and the drug of choice is penicillin. Intravenous administration of penicillin should be given, followed by oral penicillin or amoxicillin [9]. If the patient has penicillin allergy or resistance, ceftriaxone, doxycycline, clindamycin, or fluoroquinolone is recommended [10].
Figures and Tables
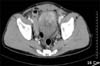 | FIG. 1Abdominal computed tomography (CT) showing wall thickening and a mass on the bladder dome. The mass extends to the abdominal wall from the bladder dome. |
 | FIG. 2Serial positron-emission tomography/computed tomography (PET/CT) images showing mild hypermetabolic wall thickening in the anterosuperior portion of the bladder (arrow heads) with hypermetabolic mesenteric and omental infiltration (arrows) extending along the urachus (thin arrow). |
 | FIG. 3(A) Partial cystectomy specimen revealing diffuse fibrotic thickening of the wall and relatively preserved luminal surface. There is an irregular necrotic lesion with yellowish foci in the deep resection margin. (B) Bacterial colony in the abscess background showing central entangled filamentous bacteria with a sunray appearance in the peripheral portion (H&E, ×400). |
References
1. Choi CK, Rim HK, Kim JS, Rim JS. A case of urachal actinomycosis. Korean J Urol. 2000. 41:183–186.
2. Lee SH, Kim KH, Kim JS, Kim MW, Lee HM, Lee KH, et al. A case of actinomycosis involving urachal remnant. Korean J Urol. 1999. 40:1714–1716.
3. Lee HJ, Oh GS, Seo JB, Chung MK. Urachal Actinomycosis: report of a case. Korean J Urol. 1999. 40:933–936.
4. Hsu CH, Lee CM, Chia CF, Lin YH. F-18 fluorodeoxyglucose positron emission tomography in an anorectal fistula with actinomycosis. Clin Nucl Med. 2004. 29:452–453.
5. Yegüez JF, Martinez SA, Sands LR, Hellinger MD. Pelvic actinomycosis presenting as malignant large bowel obstruction: a case report and a review of the literature. Am Surg. 2000. 66:85–90.
6. Cintron JR, Del Pino A, Duarte B, Wood D. Abdominal actinomycosis. Dis Colon Rectum. 1996. 39:105–108.
7. Hsiao HL, Shen JT, Yeh HC, Wu WJ, Wang CJ, Huang CH. Intra- and extra-abdominal actinomycosis mimicking urachal tumor in an intrauterine device carrier: a case report. Kaohsiung J Med Sci. 2008. 24:35–40.
8. Ho L, Seto J, Jadvar H. Actinomycosis mimicking anastomotic recurrent esophageal cancer on PET-CT. Clin Nucl Med. 2006. 31:646–647.
9. Yeung VH, Wong QH, Chao NS, Leung MW, Kwok WK. Thoracic actinomycosis in an adolescent mimicking chest wall tumor or pulmonary tuberculosis. Pediatr Surg Int. 2008. 24:751–754.
10. Al-Kadhi S, Venkiteswaran KP, Al-Ansari A, Shamsudini A, Al-Bozom I, Kiliyanni AS. Primary vesical actinomycosis: a case report and literature review. Int J Urol. 2007. 14:969–971.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download