Abstract
Purpose
The Remeex (Mechanical External Regulation) sling is a mid-urethral sling that allows adjustment of the sling tension in the postoperative period. We evaluated the early outcomes of the procedure in patients in whom the success rate of tension-free slings is low, such as with intrinsic sphincter deficiency (ISD).
Materials and Methods
We included 17 women with urodynamically proven stress urinary incontinence (SUI) who underwent the Remeex procedure and were followed for at least 12 months. The patients were considered to have ISD on the basis of a Valsalva leak point pressure (VLPP) <60 cmH2O or a maximum urethral closure pressure (MUCP) <20 cmH2O. We analyzed parameters including history taking, urodynamic study (UDS), and postoperative clinical outcomes. Patient's success and satisfaction rates were evaluated after the procedure. Also, we asked about lower urinary tract symptoms (LUTSs) with a questionnaire, and the severity of LUTSs was assessed with the Visual Analog Scale (VAS) before and 12 months after the operation.
Results
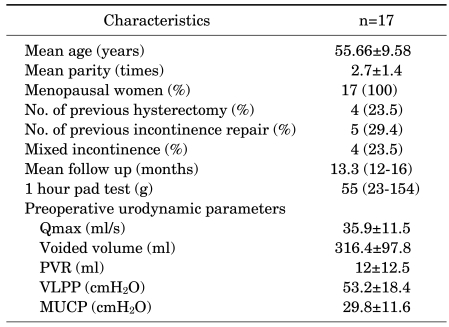
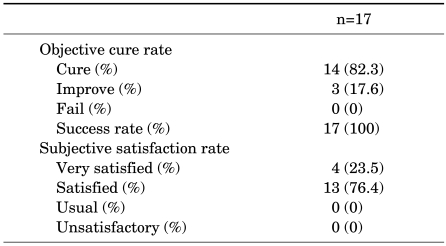
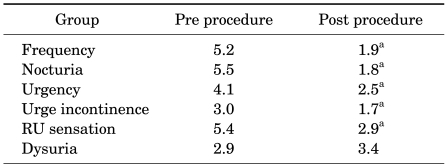
The patients' mean age was 55.6±9.58 years. Four (23.5%) patients had mixed incontinence. Five patients (29.4%) had undergone previous surgery for SUI. At a mean follow-up of 13.3 months (range, 12-16 months), 14 patients (82.3%) were cured and 3 patients (17.6%) were improved. Four patients (23.5%) answered very satisfied and 13 patients (76.4%) answered satisfied on the satisfaction questionnaire. Also, LUTSs were improved except voiding pain (p<0.05).
Urinary incontinence is generally defined as the involuntary loss of urine. It produces serious economic, social, and psychological problems that have a significant impact on women's health. Stress urinary incontinence (SUI) is involuntary leakage of urine during effort, exertion, sneezing, or coughing [1]. According to its mechanism, SUI is categorized into anatomical urinary incontinence due to urethral hypermobility and intrinsic sphincter deficiency (ISD) [2]. A variety of surgical techniques have been developed on the basis of research on SUI, and tension-free vaginal tape (TVT), which was introduced in 1996, has been frequently used. The success rates of the TVT procedure have been reported to be above 80-100% [3-6]. Many factors can produce the recurrence of SUI after surgery, however, such as the presence of a hidden ISD, mixed incontinence, hormonal changes, age-related collagen alteration, and significant weight gain. Success rates of the tension-free sling in SUI with ISD are 24-84%, although it was differently reported according to research in comparison with the success of anatomical urinary incontinence to treat urinary incontinence [7-9]. The most common problem of sling surgery has been excess tension, and concern over postoperative bladder outlet obstruction has led to the development of a number of methods for determining the proper tension. Remeex is a re-adjustable sling system for the surgical treatment of female SUI. This procedure permits the adjustment and readjustment of sling tension intra-operatively or during the postoperative period with minimally invasive ambulatory surgery, which can be performed under local anesthesia months or even years after the first procedure. Therefore, it has the advantages that urinary retention can be obtained and incontinence can be minimized. In the present study, we analyzed the results of Remeex surgery in Korean women with SUI to determine whether it is effective for SUI with ISD.
Seventeen patients were diagnosed with SUI with ISD by urodynamic study (UDS) at the urology department and underwent the Reemex procedure from February 2007 to March 2009 and were followed up for more than 12 months. All patients were preoperatively evaluated through history taking, physical examination, symptom questionnaire, 1-hour pad test, and UDS. Patients with neurological disorders or detrusor overactivity were excluded from this protocol. Additional minor exclusion factors included chronic degenerative diseases that would affect muscular and nerve tissues, advanced genital prolapses, and active or recurrent urinary tract infections. Subjects were required to have a positive result on a cough stress test and >10 g of leakage as measured by a 1-hour pad test with a standardized bladder volume (200 ml) [10]. A urodynamic evaluation was also performed. Methods, definitions, and units conformed to standards proposed by the International Continence Society [11]. Subjects were considered to have ISD identified by the Valsalva leak point pressure (VLPP) <60 cmH2O measurement in the sitting position with a volume of 150 ml in the bladder or by the maximum urethral closure pressure (MUCP) <20 cmH2O measurement in the sitting position with a volume of 200 ml in the bladder.
The operation was carried out under spinal anesthesia. Operation time, hospitalized time, complications, objective success, and satisfaction rate and change in lower urinary tract symptoms (LUTSs) were evaluated. Objective outcomes were assessed by clinical examination and a 1-hour pad test. The outcome measurement was the objective cure of stress incontinence based on a negative pad test with a standardized bladder volume (<2 g in weight) [10]. When the patients had insignificant incontinence after surgery (<10 g in weight), they were defined as improved. When the degree of incontinence did not change after surgery (>10 g in weight), it was defined as a failure. Success rates included cure and improvement. Patients' subjective satisfaction was investigated by using a questionnaire which asked them to classify their level of satisfaction with the outcome of the surgery by selecting one of four grades (very satisfactory, satisfactory, usual, and unsatisfactory). The LUTSs evaluated included frequency, nocturia, urgency, urge incontinence, residual urine sensation, and dysuria. To quantify overall satisfaction in urination before and after surgery with respect to each LUTS, a VAS was used to compare changes in VAS points before and after surgery. The VAS ranged from 0 for very satisfactory to 10 for very unsatisfactory.
All patients were evaluated at 1, 2, and more than 12 months. We conducted Student's t-tests, one-way ANOVA, and chi-square tests on the results of the study with the use of SPSS 10.0. When groups were compared and the p-value was below 0.05, it was judged as significant.
The Remeex system consists of a regulation device (varitensor) and a short polypropylene sling (35×12 mm) with suspension suture threads. The Remeex mechanical regulation part is a subcutaneous permanent implant with the "varitensor," which permits adjustment of the sling support from outside the body by means of an external manipulator (EM). The varitensor also has a mechanical connecting point for the EM on its upper side. These components are made of biocompatible materials such as titanium and ultra-high-molecular-weight polyethylene (Chirulen®). First, we made a 3 cm abdominal incision just over the pubis. The sling was placed at the level of the mid-urethra through a vaginal incision, and the suspension threads were passed through the Retzius space by a suture passer needle driven by a passer handle. After we checked the bladder integrity, the suspension threads were introduced into the varitensor. The tension of the sling could then be regulated. Clockwise rotation elevates the sling, and counterclockwise rotation lowers the sling. The adjustment can be made in the operating room according to surgical experience. The following morning the catheter was removed, and after filling the bladder with 300 ml of saline, we controlled the incontinence level, with the patient standing up and doing incontinence maneuvers, and regulated the sling elevation accordingly. Then we asked the patient to urinate and we measured the residual urine. The EM is a disposable part of the set that is removed once the desired continence level is achieved. If this was >100 ml, we lowered the sling tension. When there was no incontinence and the residual was <100 ml, we disconnected the manipulator and discharged the patient.
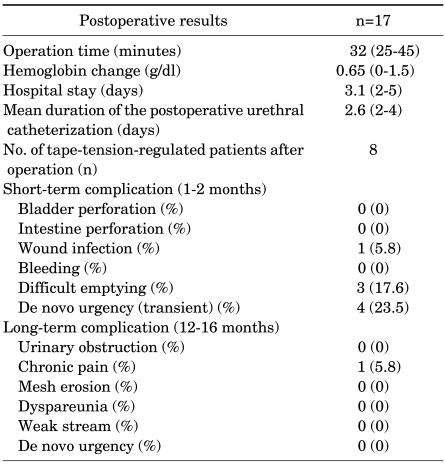
The mean age of the study subjects was 55.66±9.58 years. The numbers of patients who underwent hysterectomy and incontinence TVT operations were four and five, respectively. Four of the 17 patients had mixed incontinence. All of the patients were postmenopausal, their mean parity was 2.7±1.4, and the mean observation period was 13.3 months. The mean preoperative 1-hour pad test was 55 g (Table 1). There were no intraoperative complications, the mean operation time was 32 minutes (range, 25-45 minutes), and the mean duration of postoperative urethral catheterization was 2.6 days (range, 2-4 days). No patient needed catheterization for more than 4 days. Immediate postoperative regulation (the day after surgery) was necessary in 8 of the 17 patients. They showed no significant complications such as damage to the urinary bladder, the intestines, and blood vessels or hematoma. However, they had the following short-term complications: four patients (23.5%) had transient urgency, one patient (5.8%) had wound infection, and three patients (17.6%) had difficulty emptying. All of them improved after manipulator control. The following long-term complications occurred: one patient (5.8%) had suprapubic wound pain and three patients with hyperactivity de novo required anticholinergic treatment. No other complications were found (Table 2). Postoperatively, in 5 of the 17 patients, the stress test with 300 ml volume in the bladder was positive after catheter removal and we needed to increase the sling tension by rotating the manipulator of the varitensor clockwise a mean of 5 mm. In 3 of the 17 patients the residual was abnormal, and we had to decrease the sling tension by rotating the manipulator counterclockwise by a mean of 4 mm. Urgency was present in four patients while we regulated the prosthesis, which made the procedure of precise adjustment of the sling tension difficult. Three of these patients had mixed incontinence and were treated with anticholinergics. One month and 2 months after surgery, three patients still complained of stress incontinence that was confirmed by a stress test and a positive pad test. We therefore modified the sling support level at 2 months postoperatively. At 12 months, postoperative symptoms of incontinence were cured in 14 patients and improved in 3 patients. No failures occurred and the success rate (cure+improvement) was 100%. Four patients (23.5%) answered that they were very satisfied and 13 patients (76.4%) answered that they were satisfied. All patients answered that they were 100% satisfied (Table 3). In the VAS point change in LUTSs after surgery showed significant improvement in frequency, nocturia, urgency, urge incontinence and residual urine sensation. However, dysuria was somewhat worsened (Table 4).
Urine leakage occurs when the bladder neck opens as abdominal pressure increases without contraction of the detrusor muscle. Its causes are categorized into urethral hypermobility and ISD [2]. In 1996, Ulsten et al introduced TVT, which is a variant of sling surgery. It has been extensively used for the treatment of SUI [11]. The short-term results of TVT currently reported are 80-100% satisfactory [3,12,13]. Nilsson et al observed 80 patients for 7 years and reported an 81.3% success rate [14]. However, according to a report by Mazouni, 60% had voiding difficulty after TVT surgery [15], and severe complications such as misplacement of the tape in the bladder or urethra due to bladder perforation or urethral erosion, vessel injury, and bowel perforation have been reported [16]. In 2001, Delorme suggested using the mid-urethra sling with the polypropylene mesh passing through the obturator foramen instead of the Retzius space. Liapis et al reported that the full recovery rates of the Monarc and TVT-O procedures were 90% and 87% after 1 year of follow-up observation [17]. In a study by Seok et al, 14% of patients complained of mild voiding difficulty after TOT surgery, but it was lower than in those who had TVT [18].
ISD means insufficiency of the urethral sphincter regardless of anatomical locations, which was suggested by McGuire [19]. Some controversy exists over the definition of ISD. To diagnose ISD, we usually measure VLPP and MUCP. When the urinary bladder is filled with 150-200 ml and VLPP is below 60 cmH2O or MUCP is below 20 cmH2O, ISD is determined [20]. Kim et al categorized patients who had TVT into a group with VLPP above 60 cmH2O and a group with VLPP below 60 cmH2O and evaluated them for 5 years. Because they found no significant difference in the success rates between the two groups, Kim et al reported that VLPP is not a factor that affects the success of TVT [21]. But Paick et al categorized 221 patients who had TVT into a group whose VLPP was above 60 cmH2O and a group whose VLPP was below 60 cmH2O and observed them for a mean period of 10.5 months. Success rates were 93.1% and 82%, and the group with lower VLPP showed lower success rates of TVT [7]. Rezapour et al determined the following cases as high-risk factors of failure: when patients are older than 70 years, when MUCP is below 10, and when the patients have an immotile urethra. After TVT surgery for SUI with ISD, 74% (36 of 49 patients) showed success and 12% (12) improved. The success rate was 86%, which was lower in comparison with TVT for patients with anatomical urinary incontinence [22]. In 2006, Doo et al conducted TVT targeting 31 patients with VLPP below 60 cmH2O and 64 with VLPP above 60 cmH2O. Five years later, full recovery rates were 51.6% and 82.8%, respectively. The success rate of the ISD group was significantly lower [23]. When MUCP was below 20 cmH2O, the success rate of TVT was 73% [24].
Recently, TOT has been used for the treatment of SUI patients along with TVT, but there have been only a few reports on its outcomes for SUI with ISD. O'Connor et al categorized 43 patients who had TOT into a group with VLPP above 60 cmH2O and a group with VLPP below 60 cmH2O and observed them for 6 months. They reported that the full recovery rate of the former group was 25%, which was significantly lower than that of the latter group of 77%. The difference was because the mesh tape of TOT, which was more horizontally placed, lacked support because it wrapped a smaller part of the urethra in comparison with that by TVT [9]. Surgical procedures to treat SUI generally aim at lifting and supporting the urethrovesical junction. Sub-urethral slings serve this purpose well. The overall goal of the sling operation is to produce adequate urethral resistance to prevent stress incontinence, allowing voluntary and complete bladder emptying. Slings that are too tight are associated with voiding dysfunction and de novo urge incontinence. Slings that are too loose may still allow stress incontinence.
The most common problem with sling surgery has been the excess tension of the sling and concern over postoperative bladder outlet obstruction, which has led to the development of a number of methods for determining proper sling tension. If SUI reappears or the patient suffers persistence of urinary leakage after surgery, it will lead us to perform a new intervention to correct it. However, the success rate of incontinence reoperations is between 20% and 40% lower than that of first-time operations, and these procedures present a greater number of complications. The sub-urethral sling has traditionally been considered a procedure of last resort for previous surgical failures and for those patients with severe ISD [25].
The Remeex system allows postoperative adjustment of the sling tension. This sling system allows the surgeon to leave the sling very loose at the time of surgery with the ability to tighten or loosen the sling easily in the postoperative period to achieve continence and still maintain adequate voiding function. This system is composed of a sub-urethral sling with two traction thread sutures connected to a regulation device (varitensor) positioned above the fascia of the abdominal muscle. The varitensor and the sling remain implanted to allow readjustment of the bladder suspension level. The ability to readjust the tension avoids postsurgical urinary retention and ensures long-term continence.
Early reports from the literature [26] on the Remeex procedure showed a subjective success rate of 90%. The most common postoperative complication is de novo overactive bladder (4.7-12.5%); wound infections (3.5%) and vaginal erosion (0.8%) are also reported. Mantovani et al conducted Remeex on 32 women with SUI who had a fixed urethra, urethral hypermobility, ISD, or failed in previous surgery and observed them for 3 years. They reported that 31 were fully recovered except for one patient who had the instrument removed because of infection [27]. Araco et al conducted surgery on 38 patients with ISD and controlled the tension of 3 patients (7.9%) 6 months after the surgery. It was reported all of them showed successful results 1 year after the surgery [28]. Moreno et al evaluated the results of the Reemex system in 683 Spanish patients. They reported that the mean patient age was 59.9 years (range, 21-87 years) with a mean follow-up of 23 months (range, 6-93 months). In the total group, 30.2% of the patients had mixed incontinence, 73.1% of the patients had ISD, 35.7% of the patients had a previous history of failed surgical interventions for urinary incontinence, and 54.3% of the patients had previous pelvic-floor-associated operations. The cure rate was 92.2%, with 6.9% improvement and only 0.9% failures. No patients suffered voiding difficulties in the long term [29].
In 2010, Errando et al evaluated the outcomes, complications, and quality of life of patients after a Remeex system for recurrent SUI and ISD indications [30]. One hundred twenty-five patients with SUI were prospectively evaluated. They reported that after a mean follow-up of 38 months (range, 26-72 months), 109 patients (87%) were cured of SUI on the basis of a pad-test and clinical, and 16 patients (13%) remained incontinent. But, 9 of those (7%) were satisfied to the point that they declined re-adjustment of the sling, and 7 (6%) are on the waiting list for re-adjustment. The varitensor was removed in 1 case because of infection. No other complications were seen [30]. Our results are also similar with literature reviews [26-30] of the Remeex system in women with SUI. Therefore, it is suggested that the Remeex system is a minimally invasive technique with good, consistent results in groups of Korean female SUI patients with ISD.
We provided the Remeex adjustable sling system to 17 Korean women with SUI and evaluated the early outcomes of the Remeex procedures. The procedure provides good cure and satisfaction rates for female SUI caused by ISD with a low complication rate. The only specific difficulties or complications are related to the varitensor, which should be removed in case of chronic pain or infection. For this reason, we consider the Remeex system in patients in which the success rate of tension-free slings is lower. This study targeted a small number of subjects and the follow-up period was short. This study suggests that more subjects and a longer follow-up period are needed for more specific evaluation.
References
1. Abrams P, Cardozo L, Fall M, Griffiths D, Rosier P, Ulmsten U, et al. The standardisation of terminology of lower urinary tract function: report from the Standardisation Sub-committee of the International Continence Society. Neurourol Urodyn. 2002; 21:167–178. PMID: 11857671.

2. Blaivas JG, Romanzi LJ, Heritz DM. Walsh PC, Retik AB, Vaughan ED, Wein AJ, editors. Urinary incontinence: pathophysiology, evaluation, treatment overview and nonsurgical management. Campbell's urology. 1998. 7th ed. Philadelphia: Saunders;p. 1007–1043.
3. Ulmsten U, Falconer C, Johnson P, Jomaa M, Lanner L, Nilsson CG, et al. A multicenter study of tension-free vaginal tape (TVT) for surgical treatment of stress urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct. 1998; 9:210–213. PMID: 9795826.

4. Olsson I, Kroon U. A three-year postoperative evaluation of tension-free vaginal tape. Gynecol Obstet Invest. 1999; 48:267–269. PMID: 10592431.

5. Ulmsten U, Johnson P, Rezapour M. A three-year follow up of tension free vaginal tape for surgical treatment of female stress urinary incontinence. Br J Obstet Gynaecol. 1999; 106:345–350. PMID: 10426241.

6. Zullo MA, Plotti F, Calcagno M, Marullo E, Palaia I, Bellati F, et al. One-year follow-up of tension-free vaginal tape (TVT) and trans-obturator suburethral tape from inside to outside (TVT-O) for surgical treatment of female stress urinary incontinence : a prospective randomised trial. Eur Urol. 2007; 51:1376–1382. PMID: 17110021.
7. Paick JS, Ku JH, Shin JW, Son H, Oh SJ, Kim SW. Tension-free vaginal tape procedure for urinary incontinence with low Valsalva leak point pressure. J Urol. 2004; 172:1370–1373. PMID: 15371847.

8. Razapour M, Ulmsten U. Tension-free vaginal tape (TVT) in women with recurrent stress urinary incontinence --a long-term follow up. Int Urogynecol J Pelvic Floor Dysfunct. 2001; 12(Suppl 2):S9–S11. PMID: 11450980.
9. O'Connor RC, Nanigian DK, Lyon MB, Ellison LM, Bales GT, Stone AR. Early outcomes of mid-urethral slings for female stress urinary incontinence stratified by valsalva leak point pressure. Neurourol Urodyn. 2006; 25:685–688. PMID: 16817185.
10. Lose G, Rosenkilde P, Gammelgaard J, Schroeder T. Pad-weighing test performed with standardized bladder volume. Urology. 1988; 32:78–80. PMID: 3388665.

11. Schäfer W, Abrams P, Liao L, Mattiasson A, Pesce F, Spangberg A, et al. Good urodynamic practices: uroflowmetry, filling cystometry, and pressure-flow studies. Neurourol Urodyn. 2002; 21:261–274. PMID: 11948720.

12. Moran PA, Ward KL, Johnson D, Smirni WE, Hilton P, Bibby J. Tension-free vaginal tape for primary genuine stress incontinence: a two-centre follow-up study. BJU Int. 2000; 86:39–42. PMID: 10886080.

13. Nilsson CG. The tensionfree vaginal tape procedure (TVT) for treatment of female urinary incontinence. A minimal invasive surgical procedure. Acta Obstet Gynecol Scand Suppl. 1998; 168:34–37. PMID: 9744788.
14. Nilsson CG, Kuuva N, Falconer C, Rezapour M, Ulmsten U. Long-term results of the tension-free vaginal tape (TVT) procedure for surgical treatment of female stress urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct. 2001; 12(Suppl 2):S5–S8. PMID: 11450979.

15. Mazouni C, Karsenty G, Bretelle F, Bladou F, Gamerre M, Serment G. Urinary complications and sexual function after the tension-free vaginal tape procedure. Acta Obstet Gynecol Scand. 2004; 83:955–961. PMID: 15453893.

16. Zilbert AW, Farrell SA. External iliac artery laceration during tension-free vaginal tape procedure. Int Urogynecol J Pelvic Floor Dysfunct. 2001; 12:141–143. PMID: 11374514.

17. Liapis A, Bakas P, Creatsas G. Monarc vs TVT-O for the treatment of primary stress incontinence: a randomized study. Int Urogynecol J Pelvic Floor Dysfunct. 2008; 19:185–190. PMID: 17668144.

18. Seok NS, Suh HJ, Lee DH. Clinical outcome of transobturator Monarc procedures for treating of women with stress urinary incontinence: the 2-year follow up. Korean J Urol. 2006; 47:835–840.

19. McGuire EJ. Zinner NR, Sterling AM, editors. Urodynamic findings in patients after failure of stress incontinence operation. Female incontinence. 1980. 1st ed. New York: Alan R Liss;p. 351–360.
20. Rodriguez LV, de Almeida F, Dorey F, Raz S. Does Valsalva leak point pressure predict outcome after the distal urethral polypropylene sling? Role of urodynamics in the sling era. J Urol. 2004; 172:210–214. PMID: 15201776.
21. Kim NS, Bae JH, Lee JG. Long-term follow-up of the tension-free vaginal tape (TVT) procedure for treating female stress urinary incontinence. Korean J Urol. 2006; 47:729–733.

22. Rezapour M, Falconer C, Ulmsten U. Tension-free vaginal tape (TVT) in stress incontinent women with intrinsic sphincter deficiency (ISD)--a long-term follow-up. Int Urogynecol J Pelvic Floor Dysfunct. 2001; 12(Suppl 2):S12–S14. PMID: 11450973.
23. Doo CK, Kim JB, Kim WS, Park JS, Chung BJ, Kim JY, et al. Predictive factors affecting long-term cure and patient satisfaction of the tension-free vaginal tape procedure for the treatment of female stress urinary incontinence. J Korean Continence Soc. 2006; 10:9–16.

24. Liapis A, Bakas P, Salamalekis E, Botsis D, Creatsas G. Tension-free vaginal tape (TVT) in women with low urethral closure pressure. Eur J Obstet Gynecol Reprod Biol. 2004; 116:67–70. PMID: 15294371.

25. Amaye-Obu FA, Drutz HP. Surgical management of recurrent stress urinary incontinence: a 12-year experience. Am J Obstet Gynecol. 1999; 181:1296–1307. PMID: 10601904.

26. Sousa-Escandón A, Lema Grillé J, Rodríguez Gómez JI, Rios Tallón L, Uribarri González C, Marqués-Queimadelos A. Externally readjustable device to regulate sling tension in stress urinary incontinence: preliminary results. J Endourol. 2003; 17:515–521. PMID: 14565886.
27. Mantovani F, Castelnuovo C, Bernardini P. ReMeEx device (External Mechanical Regulator) for incontinence: implantation and regulation procedure, complications and results at 3 years follow-up. Arch Ital Urol Androl. 2004; 76:49–50. PMID: 15185826.
28. Araco F, Gravante G, Dati S, Bulzomi' V, Sesti F, Piccione E. Results 1 year after the Reemex system was applied for the treatment of stress urinary incontinence caused by intrinsic sphincter deficiency. Int Urogynecol J Pelvic Floor Dysfunct. 2008; 19:783–786. PMID: 18071617.
29. Moreno Sierra J, Marques Queimadelos A, Arano Beltran P, De La Fuente Perez P, Cerezuela Requena JF, Cortes Otero E, et al. Spanish registry of the TRT Reemex system in women with stress urinary incontinence (SUI). Arch Esp Urol. 2006; 59:169–174. PMID: 16649522.
30. Errando C, Rodriguez-Escovar F, Gutierrez C, Baez C, Araño P, Villavicencio H. A re-adjustable sling for female recurrent stress incontinence and sphincteric deficiency: outcomes and complications in 125 patients using the Remeex sling system. Neurourol Urodyn. 2010; Epub ahead of print.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download