Abstract
Purpose
We evaluated the long-term outcomes of the tension-free vaginal tape (TVT) procedure for the treatment of female urinary incontinence (UI).
Materials and Methods
We included 141 patients who underwent the TVT procedure for UI and responded to a questionnaire at the 6-year follow-up. The questionnaire included selected questions of the Korean version of the Bristol Female Lower Urinary Tract Symptom (BFLUTS) questionnaire and questions on patients' satisfaction with the procedure. Subjects were characterized as having been cured if they answered 'never' to the questions about any episodes of urine leakage.
Results
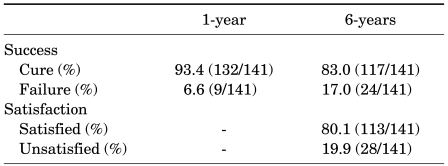
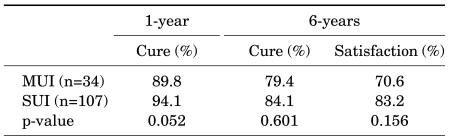
The mean follow-up was 85.5 months. The overall long-term cure rate for UI was 83.0% with a satisfaction rate of 80.1%, whereas the 1-year cure rate was 93.4%. The 1-year vs. 6-year cure rates in patients with urodynamic stress UI (SUI group; n=107) and with mixed UI (MUI group; n=34) were 94.1% vs. 84.1% and 89.8% vs. 79.4%, respectively, with no significant difference between the two groups. Also, long-term satisfaction rates in the SUI and MUI groups were 83.2% and 70.6%, without a significant difference between the two. In the MUI group, the 1-year and 6-year cure rates of urgency UI were 81.9% and 58.8%, respectively. There were no serious long-term complications related to the procedure. Most patients (85.9%) would likely recommend the TVT procedure to others.
Urinary incontinence (UI) is common in females. The incidence of female UI is 14-41% [1], and the incidence increases with aging [2,3]. The tension-free vaginal tape (TVT) procedure, which was first described in 1996 by Ulmsten and Petros, is a modified suburethral sling procedure for treating female stress urinary incontinence (SUI) based on the integral theory [4]. The TVT procedure provides high short- and intermediate-term success rates [5-7]. A few studies showed that the cure rate of the TVT procedure is 76.9-80% after long-term follow up [8-10]. However, long-term follow-up data on the TVT procedure are currently lacking in Korea. Therefore, we evaluated the long-term results of the TVT procedure for the treatment of female UI with 6-year follow-up data.
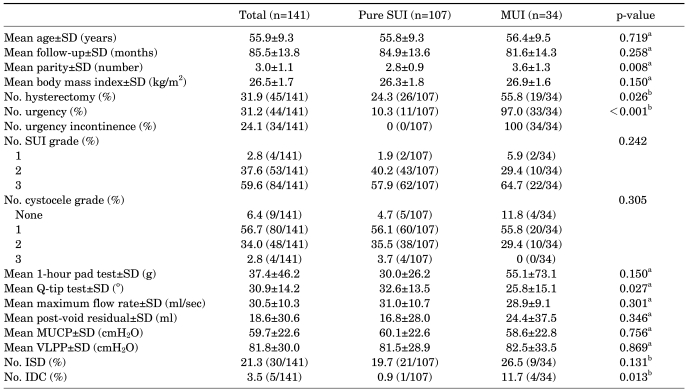
Approval for this study was provided by the Institutional Review Board of the Seoul National University Hospital. Between March 1999 and May 2003, 275 consecutive women with SUI underwent the TVT procedure at our institution. The study exclusion criteria were the following: the presence of any urinary tract infection, urogynecological malignancy, concomitant surgery (cystocele repair, etc.) or urogynecological surgery during the postoperative follow-up period, and postoperative follow-up of less than 6 years. Among 275 women, 131 patients could not be followed up because they did not respond when contacted by telephone (unavailable telephone number or interview refusal) and 3 patients died. A total of 141 (51.3%) were eligible in this retrospective study. Table 1 shows the baseline characteristics of the groups. The women's mean age was 55.9 years (range, 46-65 years) and the mean follow-up period was 85.5 months (range, 73-100 months). When we divided the patients into three groups according to Ingelman-Sundberg scale [11], 37.6% had a preoperative symptom grade of II and 59.6% had a grade of III. Preoperatively, 34 (24.1%) of the women complained of concomitant urgency UI and 44 (31.2%) complained of urgency. A total of 30 (21.3%) patients had UI combined with intrinsic sphincter deficiency and 83 (63.8%) patients had UI combined with urethral hypermobility. The rate of hysterectomy, mean parity, and the percentage of patients with involuntary detrusor contraction on the baseline urodynamic study were significantly higher in the MUI group than in the SUI group, whereas the mean degree on the Q-tip test was significantly lower in the MUI group than in the SUI group. Our preoperative protocol included history and physical examination, urinalysis, urine culture, uroflowmetry, postvoid residual urine measurement, 1-hour pad test, and multichannel videourodynamic studies. The severity of UI was classified by using the Ingelman-Sundberg scale [11].
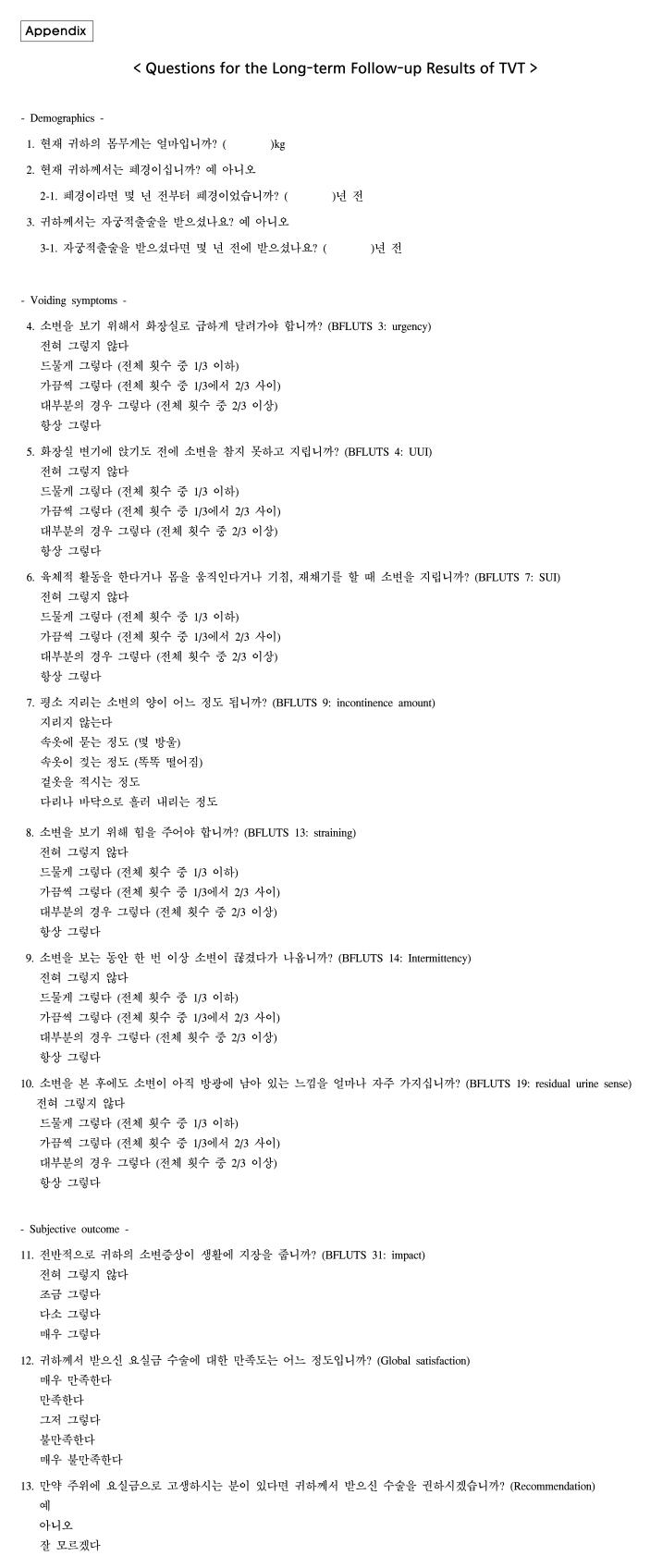
The TVT procedure was performed by 2 experienced surgeons at one institution by use of the standard technique with some modifications [12] under local anesthesia. Patients visited our clinic at 1 months, 6 months, and 1 year after surgery. Short-term follow-up evaluation included history taking, physical examination with stress test, 1-hour pad test, uroflowmetry, and post-void residual urine measurement. At the 6-year follow-up, long-term follow-up evaluation was performed by telephone questionnaire. The 6-year cure rate of the TVT procedure and patient global satisfaction were assessed by the questionnaire, which included selected questions from the Korean version of the Bristol Female Lower Urinary Tract Symptoms (BFLUTS) questionnaire [13], which evaluated LUTS and quality of life after the TVT procedure (Appendix), and two additional questions on patients' satisfaction with the procedure. At the 1-year follow-up, cure of UI after the procedure was defined as the absence of a subjective complaint of leakage and the absence of objective leakage on a stress test. At the 6-year follow-up, subjects were characterized as having been cured if they answered 'never' to questions no. 6 and 7 about any episodes of urine leakage. All other outcomes were regarded as failures.
Comparative analysis of the cure rates of TVT, patient global satisfaction, and complications between patients with urodynamic SUI (SUI group) and mixed UI (MUI group) was performed. All definitions corresponded to those of the International Continence Society [14]. Intrinsic sphincter deficiency was defined as a maximum urethral closure pressure <20 cmH2O or Valsalva leak point pressure (VLPP) <60 cmH2O [15]. Urethral hypermobility was defined as Q-tip >30° [16]. Subjects were categorized as having satisfaction if they answered 'very satisfied' or 'satisfied' to the question about patient satisfaction with the procedure. Statistical analysis was performed by using the Student's t test for continuous data and Fisher's exact test or chi-square test for categorical data. We used logistic regression analysis to determine the factors influencing cure at 6 years after the procedure. A 5% level of significance was used for all statistical testing, and all statistical tests were 2-sided. The Statistical Package for the Social Sciences (SPSS for Windows, release 17.0, SPSS Inc., Chicago, IL, USA) was used for the data analysis.
When we evaluated the cure rate, the overall 1-year cure rate was 93.4% and the 6-year subjective cure rate was 83.0%, respectively (Table 2). The overall proportion of patients who answered that they were very satisfied or satisfied with the results was 80.1% (Table 2). We divided the patients into two groups, the pure SUI group (107 patients) and the MUI group (34 patients), and compared the cure rates. The 1-year cure rate and the 6-year subjective cure rate in patients with urodynamic SUI (SUI group; n=107) and with mixed UI (MUI group; n=34) were 94.1% versus 84.1% and 89.8% versus 79.4%, respectively. In addition, when we evaluated the global satisfaction at the 6-year follow-up postoperatively, the proportion of patients who answered that they were very satisfied or satisfied was 83.2% in the SUI group and 70.6% in the MUI group without a statistically significant difference between the two (Table 3).
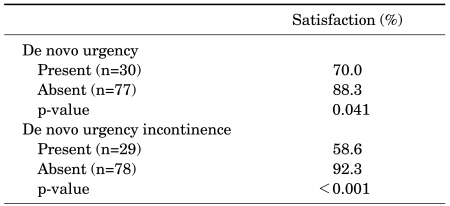
Nine patients (6.4%) had a bladder perforation. Ten women (7.1%) had urinary retention after surgery, which was managed with an indwelling catheter for <1 week. Temporary clean intermittent catheterization was required in 1.4%. Ten patients (7.1%) required catheter re-indwelling. Two patients (1.4%) underwent TVT cutting. No vaginal or urethral erosion was identified. At the 6-year follow-up, de novo urgency and de novo urgency incontinence developed in 28.0% (30/107) and 27.1% (29/107), respectively, of the pure SUI group (n=107). These worked as negative factors affecting subjective satisfaction with the operation results (Table 4). When we asked about recommendation of the TVT procedure, 122 patients (86.5%) answered that they would recommend the TVT procedure to other patients.
In the logistic regression analysis, there was no factor that predicted cure at 6 years after TVT. The odds ratios (95% CI, between high and low quartile) for persistent SUI were not increased for any factor (Table 5).
SUI is known to occur when the bladder neck and posterior urethra escape the normal anatomical position [17]. During a Valsalva maneuver, the pressure of the bladder neck and posterior urethra is lower than intravesical pressure, which leads to incontinence [17]. The short-term results of TVT have shown cure rates between 80% and 100% [5-7]. Long-term cure rates are reported to be from 71% to 86% [8-10]. Nilsson et al performed 7 years of long-term follow-up of 80 patients in 2004 and reported an 81.3% cure rate [18]. In our study, the long-term cure rate was 83.0% (117/141), and this result is almost the same as the results of previous studies. Razapour and Ulmsten performed TVT on 80 patients with mixed incontinence accompanied by urgency UI and reported an 85% cure rate, a 4% rate of improvement, and an 11% treatment failure rate within a mean follow-up period of 4 years (range, 3-5 years) [19]. In our study, the cure rate of patients with MUI at 1 year postoperatively was 89.8%, and the cure rate at 6 years postoperatively was 79.4%.
In the MUI group, the cure rate of urgency incontinence was decreased from 81.9% at 1 year postoperatively to 58.8% at 6 years postoperatively. Previous studies reported that the cure rate of urgency UI in MUI patients was 69-85% with short-term follow-up [20,21]. Holmgren et al reported that the cure rate of urgency UI at 3 years postoperatively was 60% and that at 6 to 8 years was 30% [22]. This might be due to an aging effect or atrophy of the bladder epithelium, which could be associated with the increased use of local estrogens or with neurological disorders [22].
There is still controversy about the difference between success rates of TVT procedures according to the VLPP. In 2001, Kim and Lee reported that the success rate of patients with a VLPP of less than 60 cmH2O was low [23]. In addition, Sand et al and Koonings et al reported that when the VLPP was lower than 60 cmH2O, the failure rate of the Burch operation procedure was 50% [24,25], and Song et al reported that TVT in patients with a low VLPP should be considered cautiously [26]. Conversely, Hsieh et al reported that in women with a VLPP of less than 60 cmH2O, the success rate showed a high percentage of 91.7%, suggesting that VLPP had no correlation with the success rate [27]. In our study, we divided the patients into two groups, one with a VLPP of lower than 60 cmH2O and the other with a VLPP of higher than 60 cmH2O, and the success rates did not differ significantly between the groups (81.1% versus 86.7%; p=0.59). According to the Ingelman-Sundberg scale, there was no significant difference in the success rate between the symptom Grade II group and the Grade III group postoperatively (83.3% versus 83.9%; p=1.000).
BFLUTS questionnaire is a self-descriptive urinary symptom measurement tool composed of 4 domains and 34 questions that was developed in 1996 by Abrams et al in the United Kingdom [14]. The 4 domains of the questionnaire are lower urinary tract symptom severity, sexual function, bothersomeness, and impact and quality of life. The scale of answers ranges from 'none' to 'always'. The questionnaire is designed so that the severity of symptoms can be evaluated and the impact of LUTS on daily life can be measured on every question. This is useful in evaluating the change in urinary symptoms before and after treatment, and the reproducibility and validity are known to be reliable. In our study, we selected some questions from the questionnaire associated with urgency, urgency UI, SUI, incontinence amount, straining, intermittency, feeling of incomplete emptying, and quality of life. Independent from the BFLUTS items, 2 questions were added concerning global satisfaction and recommendation.
One of the most common complications of TVT is bladder perforation, which is reported to have a rate of occurrence of 2.3% to 10% [6,28]. In our study, 9 patients out of 141 (6.4%) were reported to experience bladder perforation. Our results are comparable with those of previous studies.
The limitations of this study are, first, that it was a retrospective study, and second, that the BFLUTS questionnaire was used selectively. We added subjective questions of our own accord, therefore lowering the validity of the questionnaire. Third, there was a difference in the follow-up evaluation performed between 1 year and 6 years after the TVT, yet these results were compared and analyzed. Fourth, the study was based on the patients' subjective data and satisfaction. The severity of symptoms would probably vary from patient to patient; therefore, judgement of cure, improvement, and failure on the basis of these analyses may not always be accurate. If objective data such as uroflowmetry, residual urine measurement, and stress test had been collected at the 6-year follow-up, the results would probably have been more significant and reliable. Finally, this study was dependent on a questionnaire conducted by telephone interview; therefore, this study is vulnerable to selection bias.
In this study, the cure rate of stress UI decreased slightly at the 6-year long-term follow-up after TVT, but more than 80% of the patients who underwent the TVT procedure were satisfied with the results. At the 6-year follow-up, the cure rate of the TVT procedure was still high. However, these results are dependent on the subjective symptoms of the patient. Therefore, in order to obtain an accurate assessment of the long-term outcome of TVT, not only more long-term follow-up data but also objective data are needed.
References
1. Hampel C, Wienhold D, Benken N, Eggersmann C, Thüroff JW. Definition of overactive bladder and epidemiology of urinary incontinence. Urology. 1997; 50(6A Suppl):4–14. PMID: 9426746.

2. Iosif CF, Bekassy Z, Rydhström H. Prevalence of urinary incontinence in middle-aged women. Int J Gynaecol Obstet. 1988; 26:255–259. PMID: 2898402.

3. Thomas TM, Plymat KR, Blannin J, Meade TW. Prevalence of urinary incontinence. Br Med J. 1980; 281:1243–1245. PMID: 7427654.

4. Ulmsten U, Petros P. Intravaginal sligplasty (IVS): an ambulatory surgical procedure for treatment of female urinary incontinence. Scand J Urol Nephrol. 1995; 29:75–82. PMID: 7618052.
5. Moor RD, Serels SR, Davila GW, Settle P. Minimally invasive treatment for female stress urinary incontinence (SUI): a review including TVT, TOT, and mini-sling. Surg Technol Int. 2009; 18:157–173. PMID: 19579203.
6. Ulmsten U, Johnson P, Rezapour M. A three-year follow up of tension free vaginal tape for surgical treatment of female stress urinary incontinence. Br J Obstet Gynaecol. 1999; 106:345–350. PMID: 10426241.

7. Nilsson CG, Kuuva N. The tension-free vaginal tape procedure is successful in the majority of women with indications for surgical treatment of urinary stress incontinence. BJOG. 2001; 108:414–419. PMID: 11305550.

8. Nilsson CG, Kuuva N, Falconer C, Rezapour M, Ulmsten U. Long-term results of the tension-free vaginal tape (TVT) procedure for surgical treatment of female stress urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct. 2001; 12(Suppl 2):S5–S8. PMID: 11450979.

9. Doo CK, Hong B, Chung BJ, Kim JY, Jung HC, Lee KS, et al. Five-year outcomes of the tension-free vaginal tape procedure for treatment of female stress urinary incontinence. Eur Urol. 2006; 50:333–338. PMID: 16713066.

10. Deffieux X, Donnadieu AC, Porcher R, Gervaise A, Frydman R, Fernandez H. Long-term results of tension-free vaginal tape for female urinary incontinence: follow up over 6 years. Int J Urol. 2007; 14:521–526. PMID: 17593097.
11. Ingelman-Sundberg A, Ulmsten U. Surgical treatment of female urinary stress incontinence. Contrib Gynecol Obstet. 1983; 10:51–69. PMID: 6685605.

12. Ulmsten U, Falconer C, Johnson P, Jomaa M, Lanner L, Nilsson CG, et al. A multicenter study of tension-free vaginal tape (TVT) for surgical treatment of stress urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct. 1998; 9:210–213. PMID: 9795826.

13. Oh SJ, Park HG, Paick SH, Park WH, Choo MS. Translation and linguistic validation of Korean version of the Bristol Female Lower Urinary Tract Symptom instrument. J Korean Continence Soc. 2004; 8:89–113.

14. Abrams P, Cardozo L, Fall M, Griffiths D, Rosier P, Ulmsten U, et al. The standardisation of terminology of lower urinary tract function: report from the Standardisation Sub-committee of the International Continence Society. Neurourol Urodyn. 2002; 21:167–178. PMID: 11857671.

15. Haab F, Zimmern PE, Leach GE. Female stress urinary incontinence due to intrinsic sphincteric deficiency: recognition and management. J Urol. 1996; 156:3–17. PMID: 8648827.

16. Bergman A, McCarthy TA, Ballard CA, Yanai J. Role of the Q-tip test in evaluating stress urinary incontinence. J Reprod Med. 1987; 32:273–275. PMID: 3585870.
17. McGuire EJ, Lytton B, Pepe V, Kohorn EI. Stress urinary incontinence. Obstet Gynecol. 1976; 47:255–264. PMID: 943076.
18. Nilsson CG, Falconer C, Rezapour M. Seven-year follow-up of the tension-free vaginal tape procedure for treatment of urinary incontinence. Obstet Gynecol. 2004; 104:1259–1262. PMID: 15572486.

19. Rezapour M, Ulmsten U. Tension-free vaginal tape (TVT) in women with mixed urinary incontinence--a long-term follow-up. Int Urogynecol J Pelvic Floor Dysfunct. 2001; 12(Suppl 2):S15–S18. PMID: 11450974.
20. Debodinance P, Delporte P, Engrand JB, Boulogne M. Tension-free vaginal tape (TVT) in the treatment of urinary stress incontinence: 3 years experience involving 256 operations. Eur J Obstet Gynecol Reprod Biol. 2002; 105:49–58. PMID: 12270565.

21. Laurikainen E, Kiilholma P. The tension-free vaginal tape procedure for female urinary incontinence without preoperative urodynamic evaluation. J Am Coll Surg. 2003; 196:579–583. PMID: 12691935.

22. Holmgren C, Nilsson S, Lanner L, Hellberg D. Long-term results with tension-free vaginal tape on mixed and stress urinary incontinence. Obstet Gynecol. 2005; 106:38–43. PMID: 15994615.

23. Kim HJ, Lee JG. Short term results of tension-free vaginal tape procedure for women with stress urinary incontinence. Korean J Urol. 2001; 42:1305–1311.
24. Sand PK, Bowen LW, Panganiban R, Ostergard DR. The low pressure urethra as a factor in failed retropubic urethropexy. Obstet Gynecol. 1987; 69:399–402. PMID: 3822288.
25. Koonings PP, Bergman A, Ballard CA. Low urethral pressure and stress urinary incontinence in women: risk factor for failed retropubic surgical procedure. Urology. 1990; 36:245–248. PMID: 2392816.
26. Song S, Hong B, Choo MS. Three-year outcome of the tension-free vaginal tape procedure for treatment of female stress urinary incontinence. Korean J Urol. 2003; 44:307–311.
27. Hsieh GC, Klutke JJ, Kobak WH. Low valsalva leak-point pressure and success retropubic urethropexy. Int Urogynecol J Pelvic Floor Dysfunct. 2001; 12:46–50. PMID: 11294532.
28. Abouassaly R, Steinberg JR, Lemieux M, Marois C, Gilchrist LI, Bourque JL, et al. Complication of tension-free vaginal tape surgery: a multi-institutional review. BJU Int. 2004; 94:110–113. PMID: 15217442.
TABLE 5
Univariate predictors of cure at 6 years after TVT
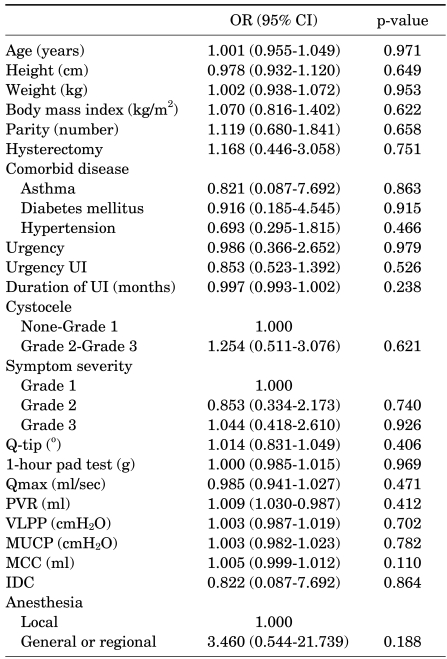
TVT: tension-free vaginal tape, OR: odds ratio, CI: confidence interval, UI: stress urinary incontinence, Qmax: maximum flow rate, PVR: post-void residual, VLPP: Valsalva leak point pressure, MUCP: maximum urethral closure pressure, MCC: maximum cystometric capacity, IDC: involuntary detrusor contraction




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download