Abstract
Purpose
We assessed the long-term effects of the tension-free vaginal tape (TVT) procedure for stress urinary incontinence (SUI) on voiding, storage, and patient satisfaction.
Materials and Methods
This retrospective study examined the records of 134 patients who had undergone the TVT procedure for SUI and were followed up for more than 5 years. Voiding function was evaluated by measuring maximum urinary flow rate (MFR), post-void residual urine volume (PVR), and storage function by using a voiding diary. Patients were asked to describe their satisfaction with the operation.
Results
MFR was lower at 1 month compared with the preoperative level, but had recovered to preoperative levels by 5 years postoperatively. However, some patients with >50%, 25-50%, and <25% decreases in the MFR at 1 month postoperatively showed a decrease in the MFR of >50% at 5 years. PVR increased over the 5 postoperative years. Of the patients with urgency and urgency incontinence, 43.8% and 48.1% showed improvement, respectively, whereas new patients developed postoperatively. Thus, the total number of patients with urgency or urgency incontinence remained similar over the 5 years. In those with a changed voiding pattern, patient satisfaction was negatively affected by de novo urgency and urgency incontinence and decreased MFR.
Conclusions
Any obstructive effect of the TVT procedure diminished over time in most patients, although a decrease in the MFR was sustained in some patients. With regard to overactive bladder symptoms, some patients were cured and some patients complained of de novo symptoms. The most major factor affecting patient satisfaction was de novo urgency.
Go to : 
Since its introduction in 1996 by Ulmsten et al [1], the tension-free vaginal tape (TVT) sling procedure has become a preferred treatment for female stress urinary incontinence (SUI) worldwide as a result of its minimally invasive nature and high success rates. However, little is known about the long-term effects of the TVT sling on voiding and storage or on long-term patient satisfaction.
Although the TVT sling is placed with no or minimal tension under the midurethra, there appears to be a significant effect on voiding [2], and reported rates of urinary retention range from 4% to 20% [3,4]. In addition, whereas preoperative urgency incontinence and overactive bladder symptoms have been reported to be resolved in 63.1-90.1% and 47.8-57.3% of patients after TVT [5,6], respectively, the rates of postoperative de novo urgency and urgency incontinence are reported to be 5-25% [7-10] after the procedure. Postoperatively, a maximal urinary flow rate (MFR) <10 ml/s [11] and retention were found to compromise patient satisfaction [12], and de novo urgency was found to have a severe impact on quality of life in 14.5% of patients [13].
The present report describes a 5-year follow-up study of female SUI patients who underwent the TVT procedure. The study examined changes in voiding and storage and also evaluated patient satisfaction.
Go to : 
Of 155 female patients who underwent the TVT procedure for SUI in three institutions between March 1999 and June 2000, the study retrospectively examined the clinical data of 134 who were followed up for more than 5 years. We previously reported long-term outcomes of the TVT procedure [14]. In this study, we re-analyzed the previous data. Pre-operative evaluation data available on all patients included detailed medical history, physical examination, neurological evaluation, uroflowmetry (MMS flowstar®), post-void residual urine volume (PVR) as measured by using a Bladder scan®, a 3-day voiding diary, and a complete multichannel urodynamic study (Aquarius 120® filling cystometry). Postoperative voiding symptoms were evaluated objectively as MFR and PVR, and storage symptoms were evaluated as urgency, frequency, and urgency incontinence by use of a 3-day voiding diary. Patients were monitored at 1 month, 1 year, and 5 years postoperatively. The data from the uroflowmetry, PVR measurements, and 3-day voiding diary were re-analyzed.
At 5 years postoperatively, the patients were asked to classify their global satisfaction level as very satisfied, satisfied, so-so, or dissatisfied. Both 'very satisfied' and 'satisfied' were scored as satisfied.
All definitions corresponded to those of the International Continence Society [15]. Analyses were performed by using statistical software (SPSS 12.0, SPSS Inc. Chicago, USA), and a p-value<0.05 was considered to indicate a significant difference. For statistical analysis, normal distributions of parameters ware analyzed by using Student's t-test. The correlation between patient satisfaction and 5-year postoperative voiding patterns was analyzed by using the chi-square test by percentage frequencies.
Go to : 
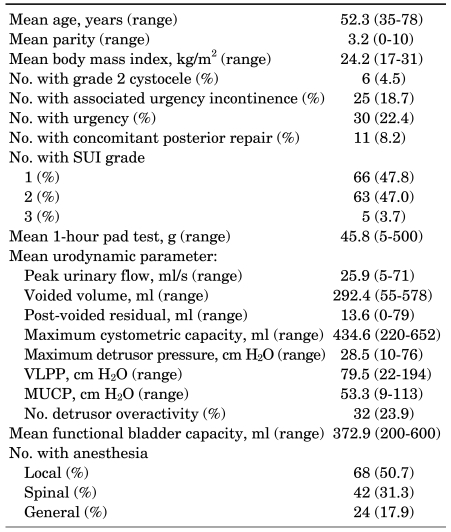
The 134 study patients had a mean age of 52.3±9.3 (range, 35 to 78) years, and the mean follow-up period was 67.0±4.6 (range, 60 to 76) months. Prior to surgery, 30 (22.4%) women had symptoms of urgency and 25 (18.7%) had symptoms of urgency incontinence. The preoperative SUI symptom grades were 1 in 66 (47.8%) patients, 2 in 63 (47.0%) patients, and 3 in 5 (3.7%) patients (Table 1). Among the patients, 7 (5.2%) patients had undergone previous anti-incontinence surgery (anterior vaginal wall sling for 4, a Raz operation for 2, and bladder neck suspension for 1), and 19 (14.2%) had undergone a previous hysterectomy. The objective 5-year cure rate was 76.9% (103/134), and the satisfaction rate was 86.6% (116/134).
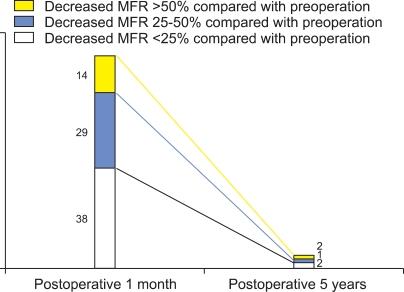
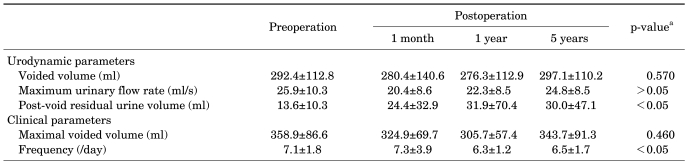
The mean MFR decreased from 25.9±10.3 ml/s preoperatively to 20.4±8.6 ml/s at 1 month after the TVT procedure (p<0.001). However, at 1 year postoperatively, the MFR increased to 22.3±8.5 ml/s, and at 5 years postoperatively it recovered to 24.8±8.5 ml/s, which was similar to the preoperative flow rate (p>0.05). PVR increased significantly from 13.6±10.3 ml preoperatively to 24.4±32.9 ml at 1 month, 31.9±70.4 ml at 1 year, and 30.3±47.1 ml at 5 years postoperatively, with the three postoperative figures being not significantly different (p>0.05) (Table 2). Of the 14 patients who showed a >50% decrease in the MFR at 1 month postoperatively, 2 (14.3%) still had a >50% decrease in the MFR after 5 years. Of the 29 patients who showed a 25-50% decrease in the MFR at 1 month postoperatively, 1 (3.4%) had a >50% decrease in the MFR at 5 years postoperatively. Of the 38 patients who showed a <25% reduction in the MFR at 1 month postoperatively, 2 (5.3%) remained the same at 5 years postoperatively. A total of 63.2% (24/38) of patients with a <25% decrease in the MFR at 1 month postoperatively showed <25% decreases in the MFR at 5 years (Fig. 1).
The mean micturition frequency per day value at 5 years postoperatively was lower than the mean preoperative value (7.1±1.8 vs. 6.5±1.7, p=0.004) (Table 2). Of the 43 patients with a preoperative micturition frequency per day of ≥8, 13 (30.2%) had a >30% decrease, 4 (9.3%) had an increase, and 26 (60.5%) had no change after 5 years. Of the patients with a preoperative micturition frequency per day of <8, 23 (34.3%) had a decrease and 18 (26.9%) had an increase after 5 years. Surgery had no effect on the maximal voided volume (358.9±86.6 ml preoperatively, 324.9±69.7 ml at 1 month, 305.7±57.4 ml at 1 year, and 343.7±91.3 ml at 5 years postoperatively; p=0.460) (Table 2).
Of the 30 patients (22.4%) with preoperative urgency, 14 (46.7%) showed improvement at 5 years postoperatively. Of the patients who did not show preoperative urgency, 16 (12.2%) developed de novo urgency postoperatively. Thus, the total number of patients with urgency remained similar over the 5 years. Of the 25 (18.7%) patients with preoperative urgency incontinence, 12 (48%) showed improvement. Of the patients who did not have preoperative urgency incontinence, 12 (11.0%) developed de novo urgency incontinence postoperatively. The total number of patients with urgency incontinence at 5 years postoperatively was 24 (17.9%), which was similar to the preoperative figure (Fig. 2).
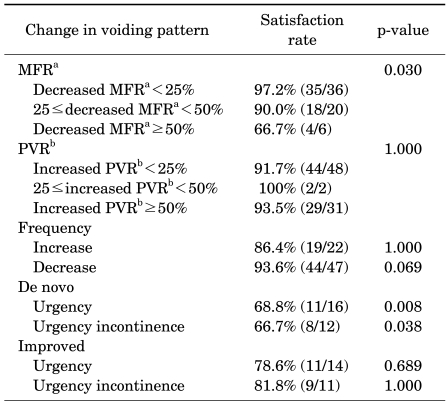
The proportion of patients reporting global satisfaction with the operation was 86.6% (116/134) at 5 years postoperatively. We analyzed the relationship between satisfaction rate and postoperative MFR at 5 years. The satisfaction rate was found to correlate with the MFR, with a greater reduction in the MFR associated with greater dissatisfaction (p=0.030) (Table 3). In contrast, changes in the PVR over 5 years did not correlate with satisfaction. For the 43 patients with a preoperative micturition frequency per day of ≥8, the satisfaction rates for those showing increased and decreased micturition frequency at 5 years postoperatively were 86.4% (19/22) and 93.6% (44/47), respectively (p>0.05). The satisfaction rates for patients who developed de novo urgency and de novo urge incontinence were 68.8% (11/16) and 66.7% (8/12), respectively, whereas the satisfaction rates for those with preoperative urgency and urgency incontinence that improved postoperatively were 78.6% (11/14) and 81.8% (9/11), respectively.
Of the postoperative voiding parameters we examined, the most important factor affecting patient satisfaction was de novo urgency (p=0.008).
Go to : 
Although the TVT procedure is generally associated with universally excellent outcomes, concerns about postoperative voiding have recently been raised.
Dietz et al examined long-term MFR, PVR, and voiding symptoms after the TVT procedure. They reported improvement in voiding as reflected in reduced residual urine volumes, normalized voided volumes, and an increased MFR [16].
The present study found that overall voiding function improved over time postoperatively, although it remained poor or worsened in some patients. Of the patients showing a >50% decrease in the MFR at 1 month postoperatively, 14.3% sustained this decrease to 5 years. Thus, patients with a greatly reduced flow rate in the immediate postoperative period are more likely to retain this reduction in the long term than are patients with smaller reductions in the immediate postoperative flow rate.
TVT procedures are known to have an obstructive effect on the urethra, which may affect voiding [17]. Our study showed that PVR increased during the follow-up period, which is consistent with previous reports [7,18]. Whereas the overall MFR was lower than preoperative levels at 1 month after the TVT procedure, it had recovered to preoperative levels by 5 years postoperatively. One hypothesis for this improvement in voiding patterns is that chronic obstruction results in progressive detrusor hypertrophy, allowing better emptying [19].
Others reported an increase in the prevalence of symptoms of urgency and urgency incontinence after the TVT procedure [20]. In contrast, the present data indicate no change in the number of patients showing these symptoms over 5 years. We found that some patients with preoperative urgency or urgency incontinence showed postoperative improvement, whereas some patients developed de novo urgency or urgency incontinence. This may reflect overactive bladder with aging and postoperative lower urinary tract obstruction. The prevalences of de novo urgency and urgency incontinence in our study (12.2% and 11.0%, respectively) were within the ranges reported in previous studies [7-10].
We previously reported that a decline in the MFR to <10 ml/s can compromise patient satisfaction with the TVT procedure [11]. In the present study, we evaluated factors additional to the MFR to understand issues affecting global patient satisfaction in more detail. For patients with altered voiding patterns after surgery, satisfaction was impaired by a decreased MFR, de novo urgency, and de novo urgency incontinence. Patient satisfaction was not found to correlate with increased PVR, micturition frequency, improved urgency, or improved urgency incontinence. The major factor affecting patient satisfaction was the development of de novo urgency (p=0.007). 0verall, 86.6% (116/134) of patients were satisfied with the operation, whereas only 80.0% (20/25) of those who developed de novo urgency were satisfied.
A previous study reported on the assessment of 87 patients using a Patient Satisfaction Questionnaire (PSQ) at 24 months postoperatively [21]. That study found that 95.5% of patients were somewhat or completely satisfied with their progress, and that the majority of patients were satisfied despite the presence of irritating voiding symptoms. In contrast, the present study over 5 years showed that the development of de novo urgency reduced patient satisfaction. The present findings will likely assist clinicians in preoperative discussions with patients regarding potential changes in voiding patterns after surgery.
A limitation with the present study was the lack of follow-up urodynamic data on patients who showed changed voiding patterns after the TVT procedure. A study by Lin et al [22] that included follow-up multi-channel urodynamic studies found that the mean preoperative values for average flow rate, MFR, PVR, and detrusor pressure at peak flow during voiding cystometry were not different from the values obtained at 3, 6, and 12 months after TVT surgery.
Go to : 
Any obstructive effect of the TVT procedure diminished over time in most patients, although a decrease in the MFR was sustained in some patients. Concerning overactive bladder symptoms, some patients were cured and some patients complained of de novo symptoms. Therefore, the total number of patients with overactive bladder was maintained similarly during the 5 years. The most major factor affecting patient satisfaction was de novo urgency.
Go to : 
References
1. Ulmsten U, Henriksson L, Johnson P, Varhos G. An ambulatory surgical procedure under local anesthesia for treatment of female urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct. 1996; 7:81–85. PMID: 8798092.

2. Sander P, Moller LM, Rudnicki PM, Lose G. Does the tension-free vaginal tape procedure affect the voiding phase? Pressure-flow studies before and 1 year after surgery. BJU Int. 2002; 89:694–698. PMID: 11966626.

3. Mishra VC, Mishra N, Karim OM, Motiwala HG. Voiding dysfunction after tension-free vaginal tape: a conservative approach is often successful. Int Urogynecol J Pelvic Floor Dysfunct. 2005; 16:210–214. PMID: 15372143.

4. Klutke C, Siegel S, Carlin B, Paszkiewicz E, Kirkemo A, Klutke J. Urinary retention after tension-free vaginal tape procedure: incidence and treatment. Urology. 2001; 58:697–701. PMID: 11711343.

5. Segal JL, Vassallo B, Kleeman S, Silva WA, Karram MM. Prevalence of persistent and de novo overactive bladder symptoms after the tension-free vaginal tape. Obstet Gynecol. 2004; 104:1263–1269. PMID: 15572487.

6. Lee GB, Kim HS, Koh JS, Kim HW, Lee YS, Suh HJ, et al. The changes of storage symptoms after tension-free vaginal tape procedures in stress urinary incontinence patients. Korean J Urol. 2007; 48:1289–1295.

7. Nilsson CG, Kuuva N, Falconer C, Rezapour M, Ulmsten U. Long-term results of the tension-free vaginal tape (TVT) procedure for surgical treatment of female stress urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct. 2001; 12(Suppl 2):S5–S8. PMID: 11450979.

8. Abouassaly R, Steinberg JR, Lemieux M, Marois C, Gilchrist LI, Bourque JL, et al. Complications of tension-free vaginal tape surgery: a multi-institutional review. BJU Int. 2004; 94:110–113. PMID: 15217442.

9. Jeffry L, Deval B, Birsan A, Soriano D, Darai E. Objective and subjective cure rates after tension-free vaginal tape for treatment of urinary incontinence. Urology. 2001; 58:702–706. PMID: 11711344.

10. Deval B, Jeffry L, Al Najjar F, Soriano D, Darai E. Determinants of patient dissatisfaction after a tension-free vaginal tape procedure for urinary incontinence. J Urol. 2002; 167:2093–2097. PMID: 11956447.

11. Park S, Hong B, Lee KS, Choo MS. Risk factors of voiding dysfunction and patient satisfaction after tension-free vaginal tape procedure. J Korean Med Sci. 2005; 20:1006–1010. PMID: 16361813.

12. Park SC, Hong BS, Choo MS. Risk factors related to immediate urinary retention after tension-free vaginal tape procedure. Korean J Urol. 2003; 44:503–508.
13. Holmgren C, Nilsson S, Lanner L, Hellberg D. Frequency of de novo urgency in 463 women who had undergone the tension-free vaginal tape (TVT) procedure for genuine stress urinary incontinence-a long-term follow-up. Eur J Obstet Gynecol Reprod Biol. 2007; 132:121–125. PMID: 16815624.

14. Doo CK, Hong B, Chung BJ, Kim JY, Jung HC, Lee KS, et al. Five-year outcomes of the tension-free vaginal tape procedure for treatment of female stress urinary incontinence. Eur Urol. 2006; 50:333–338. PMID: 16713066.

15. Abrams P, Cardozo L, Fall M, Griffiths D, Rosier P, Ulmsten U, et al. The standardisation of terminology in lower urinary tract function: report from the standardisation sub-committee of the International Continence Society. Urology. 2003; 61:37–49. PMID: 12559262.

16. Dietz HP, Ellis G, Wilson PD, Herbison P. Voiding function after tension-free vaginal tape: a longitudinal study. Aust N Z J Obstet Gynaecol. 2004; 44:152–155. PMID: 15089841.

17. Klutke JJ, Klutke CG, Bergman J, Elia G. Bladder neck suspension for stress urinary incontinence: how does it work? Neurourol Urodyn. 1999; 18:623–627. PMID: 10529710.

18. Klutke JJ, Klutke CG, Bergman J, Elia G. Urodynamics changes in voiding after anti-incontinence surgery: an insight into the mechanism of cure. Urology. 1999; 54:1003–1007. PMID: 10604698.
19. Robinson D, Anders K, Cardozo L, Bidmead J, Toozs-Hobson P, Khullar V. Can ultrasound replace ambulatory urodynamics when investigating women with irritative urinary symptoms? BJOG. 2002; 109:145–148. PMID: 11888096.

20. Liapis A, Bakas P, Creatsas G. Long-term efficacy of tension-free vaginal tape in the management of stress urinary incontinence in women: efficacy at 5- and 7-year follow-up. Int Urogynecol J Pelvic Floor Dysfunct. 2008; 19:1509–1512. PMID: 18542836.

21. Richter HE, Norman AM, Burgio KL, Goode PS, Wright KC, Benton J, et al. Tension-free vaginal tape: a prospective subjective and objective outcome analysis. Int Urogynecol J Pelvic Floor Dysfunct. 2005; 16:109–113. PMID: 15789144.

22. Lin LY, Sheu BC, Lin HH. Sequential assessment of urodynamic findings before and after tension-free vaginal tape (TVT) operation for female genuine stress incontinence. Eur Urol. 2004; 45:362–366. PMID: 15036684.

Go to : 




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download