Abstract
Purpose
The purpose of this study was to investigate social and behavioral factors associated with prostate-specific antigen (PSA) screening in men in California, United States, who were over 40 years of age and had ever heard about PSA screening.
Materials and Methods
This survey was administered as a random-digit-dialing telephone survey to produce reliable estimates of medium-sized counties. It surveyed 42,000 households and interviewed 58,407 people randomly. It considered socioeconomic status and health behavior as affecting PSA screening. Access to health care was measured as having regular health care access. The main outcome measure was self-report of ever having undergone PSA screening at least once in the respondent's lifetime.
Results
Of 8,864 respondents, 82.2% were White, 7.7% were Latin, 4.2% were African American, and 5.9% were Asian. The respondents' mean age was 60.13 years. Age was the significant factor for PSA screening. Respondents aged 50-59 years were 3.5 times as likely to have undergone PSA screening as were those aged 40-49 years (OR=3.49, p≤0.001). Race was not statistically significant after considering other factors. People who had never married had statistically significantly lower screening than did people who were married (OR=0.71, p=0.001). Poverty levels were statistically significant in both the unadjusted and the adjusted analysis. People who had no regular health care access were much less likely to have undergone PSA screening than were people who had regular health care access (OR=0.22, p=0.001).
Conclusions
The likelihood of PSA screening was positively associated with increased age, marital status (married), higher socioeconomic status (higher federal poverty level and higher educational attainment), and health care access. However, there was no statistically significant association of PSA screening with race, employment, exercise, smoking, or drinking status.
Prostate cancer is the most common malignancy among men in the United States and is the second leading cause of male cancer death. The incidence of prostate cancer varies widely among ethnic populations, and African American men in the United States have the highest incidence of prostate cancer [1].
The prostate-specific antigen (PSA) test has become widespread since 1980. If the serum PSA is more than 4 ng/ml, a man is considered to be at high risk of prostate cancer and a biopsy usually follows. In 2002, 75% of men aged 50 years and older had undergone at least 1 PSA testing, and 57% had been tested within the previous 2 years, despite debate about the value of screening for prostate cancer in terms of lowering prostate cancer mortality [2].
The American Cancer Society recommends that PSA and a digital rectal examination be offered annually to men aged 50 years or more who are expected to live at least 10 years [3]. Prostate cancer screening is important because early detection of the disease reduces prostate cancer mortality.
However, there are disparities with PSA screening in the United States; African Americans are less likely to undergo PSA screening than are Whites. Researchers previously reported a higher rate of elevated PSA (greater than 4.0 ng/ml) and a higher prostate cancer detection rate in African Americans than in White men in a community-based screening study [4]. Yet little is known about PSA screening behaviors and factors affecting those behaviors. Researchers have found that health care access, insurance coverage, and socioeconomic status (SES) are associated with PSA screening behavior [5]. The purpose of this study was to investigate the effects of sociodemographic and behavioral factors on PSA screening practice.
The 2005 California Health Interview Survey (CHIS 2005) was a collaborative project of the UCLA Center for Health Policy Research, the California Department of Health Services, and the Public Health Institute. The survey focused on a number of public health topics including health status and conditions, health-related behaviors, insurance coverage, and access to health care services. The survey was administered as a random-digit-dialing (RDD) telephone survey of California households that was designed to produce reliable estimates for the whole state, including medium and small-size counties. CHIS 2005 is the third data collection cycle (following CHIS 2001 and 2003) and was conducted between July 2005 and April 2006. It surveyed 42,000 households and interviewed 58,407 persons (43,020 adults aged 18 years and older, 4,029 adolescents, and 11,358 children) randomly drawn from every county, and it is the largest state survey in the United States.
This study considered sociodemographic information, SES, health behaviors, and access to health care as factors affecting PSA screening. Sociodemographic indicators included age, which was categorized into the age groups of ≥40 & <50, ≥50 & <60, ≥60 & <70, ≥70 & <80, and ≥80. For SES indicators, educational attainment, poverty, and working status were measured. Educational attainment was categorized into more than graduate school, ≥ 4 years of college, some college, and ≤ high school graduate. The poverty level was categorized into ≥300%, 200-299%, 100-199%, and ≤99% of the Federal Poverty Level (FPL). This poverty level is based on the U.S. Department of Commerce Bureau of the Census poverty thresholds, in which poverty is calculated as the proportion of income per number of people in the family. Working status was first categorized into full-time employed, part-time employed, and unemployed. Exercise, smoking status, and drinking habits were analyzed as indicators of health behaviors. Exercise was categorized as people who do exercise (vigorous exercise) <30 minutes and ≥30 minutes in a day. Respondents were categorized by smoking status as current smokers, former smokers, or never smokers. Access to health care was measured by "having regular health access except emergency visits."
To examine PSA screening among men over 40 years of age, logistic regression was used across various levels of predictors. First, bivariate analyses were performed to determine which independent variables would distinguish people who had higher PSA screening practice. Second, interaction terms were tested between variables on the basis of the literature and behavioral plausibility. There were no significant interactions between respondent variables and independent variables. Finally, multivariate logistic regression analyses were conducted to identify the most important predictors of having PSA screening. The analysis was conducted by using STATA statistical software version 9.0.
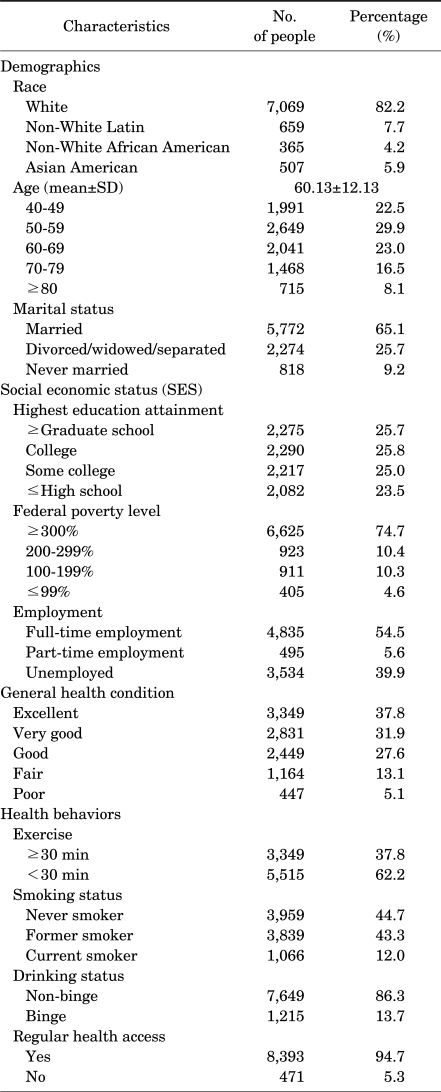
The 8,864 eligible respondents represented persons who lived in California. Of the respondents, 82.2% were White, 7.7% were non-White Latin, 4.2% were non-White African American, and 5.9% were Asian American. The respondents' mean age was 60.13 years (SD=12.13). A total of 6,264 (70.7%) of the respondents had ever undergone PSA screening. Of the respondents, 22.5% were aged 40-49 years, 29.9% were aged 50-59 years, 23% were aged 60-69 years, 16.5% were aged 70-79 years, and 8.1% were aged 80 years or older. About 65% of the respondents were married, 25.7% were divorced or widowed or separated, and 9.2% were never married (Table 1).
Concerning educational attainment, 51.5% of the respondents had more than a college education, 25.0% had some college education, and only 23.5% had less than a high school education. Considering income, the study measured the poverty level, and 74.7% were above 300% FPL and 4.6% were below 100% FPL. Of the total, 54.5% were employed full-time, 5.6% were employed part-time, and 39.9% were unemployed (Table 1).
Of the total, 37.8% of the respondents said that they had excellent health, 13.1% reported their health as fair, and 5.1% reported their health as poor. More than 60% of the respondents performed vigorous exercise less than 30 minutes every day. Considering health behaviors, there were 12.0% current smokers and 13.7% binge drinkers. Among the respondents, 94.7% had regular health access and 5.3% did not (Table 1).
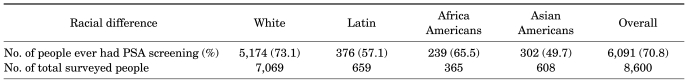
Non-White Latin persons were 0.49 times (95% CI: 0.41-0.57) less likely to have PSA screening practice than were White persons. Non-White African Americans were 0.69 times (95% CI: 0.56-0.87) less likely and Asian Americans were 0.54 times (95% CI: 0.45-0.65) less likely.
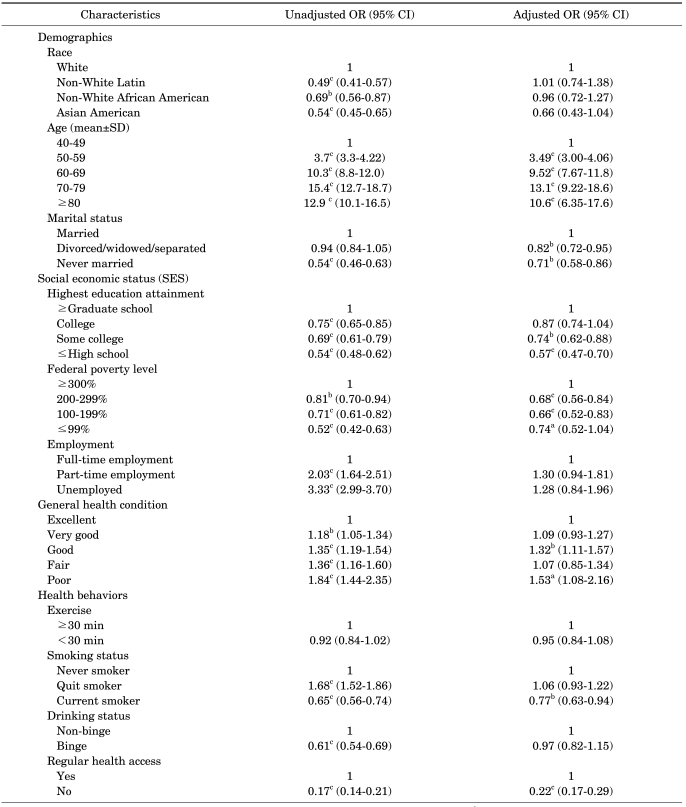
The prevalence of PSA screening by race differed: it was 73.1%, 57.1%, 65.5%, and 49.7% among Whites, non-White Latins, non-White African Americans, and Asian Americans, respectively. The difference in prevalence was statistically significant by Chi-square test (Table 2). As age increased, people were more likely to undergo PSA screening; men who were 50-59 years old were 3.7 times as likely to have undergone PSA screening as were those aged 40-49 years, and the group aged 60-69 years was 10.3 times as likely. Compared with married people, people who were divorced/widowed/separated and never married were less likely to have undergone PSA screening. The relationship between each of race, age, and marital status and PSA screening was statistically significant. The age group of 50-59 years was 3.5 times as likely to have undergone PSA screening as was the age group of 40-49 years [odds ratio (OR)=3.49, p≤0.001]. Race was not statistically significant after considering other factors; however, people who never married had a statistically significantly lower odds of having undergone PSA screening (OR=0.71, p=0.001) than did people who were married (Table 3).
Examining the relationship between SES and PSA screening showed that educational attainment was associated with PSA screening behavior. People who had more than a graduate school education were more likely to undergo PSA screening than were people who had a college education, but there were no statistically significant differences after adjustment. Yet, people who had an educational attainment level of less than some college were less likely to undergo PSA screening than were people who had more than a graduate school education. This difference was statistically significant even after adjustment. Poverty levels were statistically significant in both the unadjusted and the adjusted analyses. The relationship between employment and PSA screening showed statistical significance in the bivariate analysis, but the significance disappeared in the multivariate analysis (Table 3).
People whose general health condition was good had a 1.35 times higher PSA screening practice than did those whose general condition was excellent, and people whose general condition was poor had a 1.84 times higher PSA screening practice than did those whose general condition was excellent. There was a statistically significant positive association between general health condition and PSA screening within the unadjusted analysis. After adjustment, the groups whose general condition was very good and fair were not statistically significantly different from the excellent group but the groups whose general condition was good and poor were still statistically significantly different (Table 3).
Exercise status did not have an association with PSA screening. Smoking status had an association with PSA screening. Current smokers were 0.65 times less likely to have undergone PSA screening than were never smokers (0.65, p=0.001) in the unadjusted analysis and 0.77 times less likely in the adjusted analysis (0.77, p=0.009). Binge drinkers were 0.6 times less likely to have undergone PSA screening than were non-binge-drinkers (0.61, p<0.001) in the unadjusted analysis, but there was no statistically significant difference in the adjusted analysis (Table 3).
Persons without regular health care access were less likely to have undergone PSA screening than were persons with regular health care access, with a statistically significant association in the adjusted analysis (OR=0.22, p=0.001) (Table 3).
The principal screening tests for the detection of asymptomatic prostate cancer are the DRE and measurement of levels of the serum tumor marker PSA. Prostate biopsy is performed in patients with an abnormal digital rectal examination or an elevated serum PSA level. Although PSA is one of the best tumor markers currently available for medical practice, the major drawback of prostate cancer screening with PSA is that it is not accepted on a national basis. PSA screening, which is a widely accepted method for prostate cancer detection, is important for detecting early stages of prostate cancer. PSA screening is widespread in the United States; in 2000, about 57% of men aged 50 years and older had a PSA test [6].
We investigated the associations between PSA screening practice among men over 40 years old who had ever heard about PSA screening and demographics (race, age, and marital status), SES (education, poverty level, and employment), general health condition, access to health care, and health behaviors (exercise, smoking, and drinking). The purpose of the study was to find social and behavioral factors associated with PSA screening practice, and we can utilize results of the study to encourage people to undergo PSA screening for early detection of the disease.
Jones and his colleagues assessed the impact of study variables on race differences in long-term survival [7]. The authors mentioned that with 69 African Americans (60.0%) and 58 Whites (42.7%) diagnosed with non-localized cancer, African Americans were significantly more likely than Whites to be diagnosed with cancer that had progressed beyond a localized stage (unadjusted OR=2.02; 95% CI: 1.21-3.38), and modifiable factors such as screening practice and sociodemographic factors accounted for >60% of the race difference in prostate cancer stage at diagnosis. Resnick et al reported in patients with low-risk prostate cancer treated by radical prostatectomy that there existed no significant differences in surrogate measures of disease control, risk of disease upgrading, estimated tumor volume, or recurrence-free survival between Whites and African Americans [8]. Therefore, concern about the racial differences in prostate cancer screening is not negligible. Considering racial disparities, we categorized our respondents into 4 racial groups: White, non-White Latin, non-White African American, and Asian American, and compared the PSA screening practice among the groups. Compared with Whites, there was no statistically significant difference in PSA screening practice among non-White African Americans and Asian Americans. There was no statistically significant difference among the 3 different races compared with Whites in the adjusted analysis. This may have been because of the unbalanced sample sizes. The majority of the sample, 82.2%, was White, compared with 7.7% non-White Latin, 4.2% non-White African American, and 5.7% Asian American.
Screening efforts are typically aimed at detecting cancer earlier in its natural history, and age is one of the most important factors influencing the choice of the optimal treatment arm and its outcome. As radical prostatectomy and radiation therapy continue to evolve for prostate cancer, it becomes increasingly important to understand the prognostic factors that affect outcomes. Age, stage, and grade are among the most important treatment factors to analyze, because they are used ubiquitously to guide prostate cancer treatment. Particularly in prostate cancer, watchful waiting is an important treatment modality and men undergoing surveillance have lower local tumor stages, grades, and PSA and are older than are those who received active primary treatment (p<0.001) [9]. Accordingly, age is a key factor in stratifying the screening population. Our study found a strong association between PSA screening and age in both the unadjusted and the adjusted analysis. The results revealed that the possibility of undergoing PSA screening increased in proportion to increasing age. The group aged 50-59 years old was 3.49 times as likely to undergo PSA as was the group aged 40-49 years old, and the group aged 60-69 years old was 9.52 times as likely to undergo PSA screening as was the group aged 40-49 years old. This might be because of more exposure to cancer education and increased awareness among the older population; people are more likely to be exposed to cancer education or materials as they get older and they are also more likely to pay attention to issues of cancer screening. After we controlled for all other factors, age was still a statistically significant factor associated with PSA screening. It would be meaningful to investigate different age groups related to PSA screening behaviors and the factors that affect those behaviors.
Clegg et al analyzed population-based cancer registry data from the Surveillance, Epidemiology, and End Results (SEER) Program at the National Cancer Institute (NCI) and computed cohort-based age-adjusted cancer incidence rates. The impact of SES on cancer incidence and stage of diagnosis was evaluated. Men and women with less than a high school education had elevated lung cancer rate ratios of 3.01 and 2.02, respectively. Those with annual family incomes less than $12,500 had incidence rates that were more than 1.7 times the lung cancer incidence rate of those with incomes of $50,000 or higher. Lower income was also associated with a statistically significantly increased risk of distant-stage breast cancer among women and distant-stage prostate cancer among men [10].
With SES, our results showed the same finding as previous studies. As the poverty level decreased, people were less likely to undergo PSA screening. The group at 200-299% of the poverty level was 0.68 times less likely to undergo PSA screening than was the group with a poverty level of more than 300%. The odds ratio of the group at 100-199% of the poverty level compared with the group at a poverty level of more than 300% was 0.66 (p=0.001) and it was statistically significant with control for other factors (Table 3). In addition, people who were married were more likely to undergo PSA screening than were those who were divorced or separated or those who were never married. This might be because those in a marital group had more responsibility for their spouse and family economics, and they would pay more attention to their health and cancer prevention.
We expected that the likelihood of undergoing PSA screening would be decreased in people with lower educational attainment, those with lower awareness of cancer screening, and those who paid less attention to health promotion and prevention. The results agreed with our expectation. People who had a college education were 0.87 times less likely to undergo PSA screening than were people who had more than a graduate school education, but the difference was not statistically significant in the multivariate analysis. People whose educational attainment was less than high school were 0.54 times less likely to undergo PSA screening than were people who had a graduate school education, and this difference was statistically significant with control for other factors (p=0.001).
Finally, we analyzed the association between PSA screening and regular health access. There was a strong association between having a usual source of health care and receiving screening for breast and cervical cancers [11-14]. Even generalizations about the relationship between insurance coverage and cancer screening were not possible because that relationship has been examined in few studies. It is generally accepted that there is a positive correlation between the source of health care and performing cancer screening. In our study, the health care system and PSA screening were strongly associated. People who had regular health care access were more likely to undergo PSA screening than were people who had no regular health care access. People who have regular access would have a greater chance of receiving screening tests along with a physician's recommendation regarding preventive behavior. This result indicates that access to health care is a critical factor for PSA screening practice, and we need to consider ways to advocate PSA cancer screening to people who don't have regular access to health care.
Our study had some limitations. First, it was a cross-sectional study, so we did not evaluate the time to start PSA screening or the regularity of PSA screening. Second, the CHIS is a telephone survey; therefore, it potentially excludes people of low SES and people with severely impaired physical or mental health. Third, this study did not consider detail about past medical history. Not only prostatic disease, but also chronic medical diseases, such as diabetes mellitus and cardiovascular diseases, have been known to affect whether a man decides to undergo PSA testing or not. This point could be a pitfall of this study. However, this was a huge, community-based telephone survey. We think that the large number of the population can overcome the effect of someone's medical condition on his PSA-screening behavior. Last, our results for these surveys may not be representative of the entire country. These limitations notwithstanding, our results corroborate previous studies of not only PSA screening in prostate cancer, but also other popular cancer screening programs. Briefly, our results show that the likelihood of PSA screening was positively associated with increased age, marital status, higher socioeconomic status, and health care access. Additionally, our research suggests that there is a need to find effective ways of widening PSA screening to prostate cancer screening-naïve groups, especially those who are older or unmarried and lower socioeconomic groups.
SES reflects PSA screening behavior in males over 40 years old in California, United States. The likelihood of PSA screening was positively associated with increased age, marital status (married), higher SES (higher federal poverty level and higher educational attainment), and health care access. However, there was no statistically significant association of PSA screening with race, employment, exercise, smoking, or drinking status. These results corroborate previous studies of not only PSA screening in prostate cancer, but also other popular cancer screening programs.
References
1. Klein EA, Platz EA, Thompson IM. Wein AJ, Kavoussi LR, Novick AC, Partin AW, Peters CA, editors. Epidemiology, etiology, and prevention of prostate cancer. Campbell-Walsh urology. 2007. 9th ed. Philadelphia: Saunders;p. 2854–2873.
2. Sirovich BE, Schwartz LM, Woloshin S. Screening men for prostate and colorectal cancer in the United States: does practice reflect the evidence? JAMA. 2003; 289:1414–1420. PMID: 12636464.
3. Smith RA, von Eschenbach AC, Wender R, Levin B, Byers T, Rothenberg D, et al. American Cancer Society guidelines for the early detection of cancer: update of early detection guidelines for prostate, colorectal, and endometrial cancers. Also: update 2001--testing for early lung cancer detection. CA Cancer J Clin. 2001; 51:38–75. PMID: 11577479.

4. Smith DS, Bullock AD, Catalona WJ, Herschman JD. Racial differences in a prostate cancer screening study. J Urol. 1996; 156:1366–1369. PMID: 8808873.

5. Liu L, Cozen W, Bernstein L, Ross RK, Deapen D. Changing relationship between socioeconomic status and prostate cancer incidence. J Natl Cancer Inst. 2001; 93:705–709. PMID: 11333293.

6. Ross LE, Coates RJ, Breen N, Uhler RJ, Potosky AL, Blackman D. Prostate-specific antigen test use reported in the 2000 National Health Interview Survey. Prev Med. 2004; 38:732–744. PMID: 15193893.

7. Jones BA, Liu WL, Araujo AB, Kasl SV, Silvera SN, Solar-Vila H, et al. Explaining the race difference in prostate cancer stage at diagnosis. Cancer Epidemiol Biomarkers Prev. 2008; 17:2825–2834. PMID: 18829446.

8. Resnick MJ, Canter DJ, Guzzo TJ, Bruker BM, Bergey M, Sonnad SS, et al. Does race affect postoperative outcomes in patients with low-risk prostate cancer who undergo radical prostatectomy? Urology. 2009; 73:620–623. PMID: 19100607.

9. Stattin P, Holmberg E, Bratt O, Adolfsson J, Johansson JE, Hugosson J. Surveillance and deferred treatment for localized prostate cancer. Population based study in the National Prostate Cancer Register of Sweden. J Urol. 2008; 180:2423–2429. PMID: 18930283.

10. Clegg LX, Reichman ME, Miller BA, Hankey BF, Singh GK, Lin YD, et al. Impact of socioeconomic status on cancer incidence and stage at diagnosis: selected findings from the surveillance, epidemiology, and end results: National Longitudinal Mortality Study. Cancer Causes Control. 2009; 20:417–435. PMID: 19002764.

11. Pearlman DN, Rakowski W, Ehrich B, Clark MA. Breast cancer screening practices among black, Hispanic, and white women: reassessing differences. Am J Prev Med. 1996; 12:327–337. PMID: 8909641.

12. Phillips KA, Kerlikowske K, Baker LC, Chang SW, Brown ML. Factors associated with women's adherence to mammography screening guidelines. Health Serv Res. 1998; 33:29–53. PMID: 9566176.
13. Potosky AL, Breen N, Graubard BI, Parsons PE. The association between health care coverage and the use of cancer screening tests. Results from the 1992 National Health Interview Survey. Med Care. 1998; 36:257–270. PMID: 9520952.
14. Breen N, Wagener DK, Brown ML, Davis WW, Ballard-Barbash R. Progress in cancer screening over a decade: results of cancer screening from the 1987, 1992, and 1998 National Health Interview Surveys. J Natl Cancer Inst. 2001; 93:1704–1713. PMID: 11717331.

TABLE 1
Characteristics of men aged over 40 years who had ever heard about PSA screening in California
In this article, the authors concluded from a survey-based study of a population residing in North America that the likelihood of receiving prostate-specific antigen (PSA) screening was positively associated with age, marital status, socioeconomic status, and health care access. Meanwhile, they also observed that there was no statistically significant association of PSA screening with race, employment, exercise, smoking, or drinking status. As in Western countries, debate continues on whether PSA screening would be beneficial for Korean men. Thus, the subject of current study would be a matter of interest to a wide spectrum of Korean physicians. Still, I am somewhat perplexed with regard to the reported results. First, it is widely acknowledged that economic disparity exists among Americans according to race. Although situations have changed for the better in America through recent years, it would still be difficult to argue that African Americans in general currently have equal socioeconomic status to their white counterparts in America. Because those with higher living standards (certainly being employed) may well have easier access to medical services, the observed data from the authors' study are not easy to interpret [1]. Looking at the study subjects, it may just be the unequal racial makeup that could easily have affected the outcome. Because the parameters analyzed, such as race, socioeconomic status, employment, and health care access, are all significantly associated, a clear-cut conclusion from the authors' study is not possible. Also, it can be suggested that people with chronic disease (such as cardiovascular disease and diabetes) who are under regular medical care are more prone to being screened for various medical conditions. Accordingly, such issues should have been checked out for a study on PSA screening. Because prostate cancer awareness is higher than ever in Korea today, it would be safe to state that similar studies on Korean men over 40 years of age are warranted.
References
1. Gilligan T, Wang PS, Levin R, Kantoff PW, Avorn J. Racial differences in screening for prostate cancer in the elderly. Arch Intern Med. 2004; 164:1858–1864. PMID: 15451760.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download