INTRODUCTION
Benign prostatic hyperplasia (BPH) is one of the most common illnesses occurring in post-middle-aged men, and its importance and frequency are increasing at a dramatic pace [
1]. The initial treatment of BPH is mostly through medication, but some patients who show no improvements in their conditions with medication choose surgical treatment [
2]. Furthermore, when BPH is coupled with recurrent urinary retention, urinary tract infection (UTI), bladder stone, renal insufficiency, or gross hematuria, surgical treatment is considered first over medical management [
2]. Transurethral resection of the prostate (TURP) is the most standard surgical procedure performed for BPH to date [
3]. However, complications such as bleeding, retrograde ejaculation, and transurethral resection syndrome (TUR syndrome) can occur after TURP [
4]. In order to minimize such complications, minimally invasive procedures, such as photoselective vaporization of the prostate (PVP) using lasers, have been introduced. Recent PVP procedures have used high-energy 80 W potassium-titanyl-phosphate (KTP) lasers and 120 W lithium-triborate (LBO) lasers. Numerous studies have shown that PVP shows surgical outcomes similar to those of TURP, but reduces the hospital stay and catheterization time dramatically and further reduces bleeding, thereby decreasing possible complications [
5-
7]. To date, short-term results of PVP domestically have been presented on a number of occasions, but mid- to long-term results are largely lacking. Therefore, the aim of this study was to report 2-year surgical outcomes and durability of PVP in the treatment of symptomatic BPH.
Go to :

MATERIALS AND METHODS
This study was approved by the Institutional Review Board (IRB approval number: H-1003-021-311) at the Seoul National University Hospital. Between January 2006 and July 2007, 169 men with lower urinary tract symptoms (LUTS) or BPH that did not respond to medical treatment with an alpha-blocker underwent PVP by a single surgeon. Only 74 patients who had 2 years of follow-up data after the PVP procedure were included in this retrospective study. The exclusion criteria were as follows: 5-alpha-reductase inhibitor use, presence of an indwelling urinary catheter, previous prostate surgery, urethral stricture, prostate malignancy, and neurogenic bladder disease. All patients underwent a preoperative evaluation with transrectal ultrasound (TRUS) and multichannel video urodynamics (MMS UD-2000, Medical Measurement System, Enschede, The Netherlands) in addition to a standard evaluation for LUTS and BPH, including history, physical examination with digital rectal examination, International Prostate Symptom Score (IPSS), urinalysis, 3-day frequency-volume chart (FVC), serum creatinine, and serum prostate-specific antigen (PSA). After the PVP, the efficacy of this treatment for LUTS/BPH was assessed at 1, 3, 6, 12, and 24 months postoperatively by use of the IPSS and uroflowmetry with post-void residual urine volume (PVR).
Safety, including postoperative adverse events, was evaluated at each follow-up visit. To assess the subjective and objective surgical outcomes, and their durability on the basis of prostate size, the patients were stratified into two groups according to the median prostate volume: a prostate volume less than 45 ml (n=39) versus a prostate volume of 45 ml or greater (n=35).
All variables are reported as medians (25th, 75th percentiles) or as numbers of patients with percentages in parentheses. The variables were evaluated for statistically significant differences between the baseline measures and the measures obtained after PVP by use of the Wilcoxon signed-rank test. The comparative analysis between the two groups was performed by using the Mann-Whitney U test for continuous variables and the Fisher's exact test for categorical variables. A 5% level of significance was adopted for all statistical testing, and all statistical tests were two-sided. The Statistical Package for the Social Sciences (SPSS for Windows, release 12.0, SPSS Inc., Chicago, IL, USA) was used for the data analysis.
Go to :

RESULTS
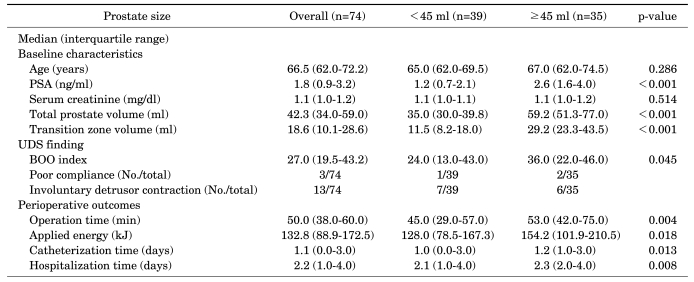
The baseline data are shown in
Table 1. In all patients, total prostate volume and transitional volume were 42.3 ml (range, 34.0-59.0 ml) and 18.6 ml (range, 10.1-28.6 ml), respectively. The larger size group (total prostate volume ≥ 45 ml) had significantly higher PSA values, bladder outlet obstruction index, and total energy used than did the smaller size group (total prostate volume <45 ml) (p<0.05). Also, the former had a significantly longer operation time, duration of catheterization, and hospital stay than did the latter (p<0.05).
TABLE 1
Baseline patient characteristics and perioperative outcome data
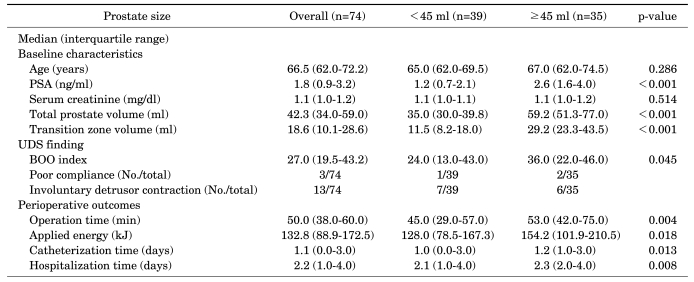

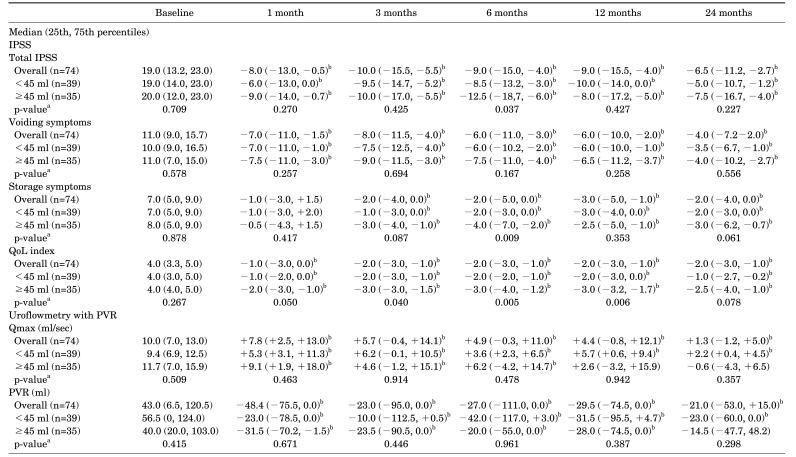
Table 2 lists the subjective and objective surgical outcomes and compares the changes in the parameters of the IPSS and uroflowmetry with PVR between the smaller size and the larger size groups. Overall, total IPSS, subtotal voiding symptom score, quality of life (QoL) index, maximum flow rate (Qmax), and PVR all showed significant improvement compared with baseline starting from 1 month, and these improvements were maintained up to 24 months postoperatively. The subtotal storage symptom score showed significant improvement compared with baseline starting from 3 months postoperatively, and this improvement also was maintained up to 24 months postoperatively. These tendencies were also observed in the smaller size group. However, in the larger size group, there was no significant improvement compared with baseline in the PVR at 24 months postoperatively or in the Qmax at 12 and 24 months postoperatively.
TABLE 2
Overall follow-up of subjective and objective micturition parameters and comparison of parameters in different prostate size subgroups
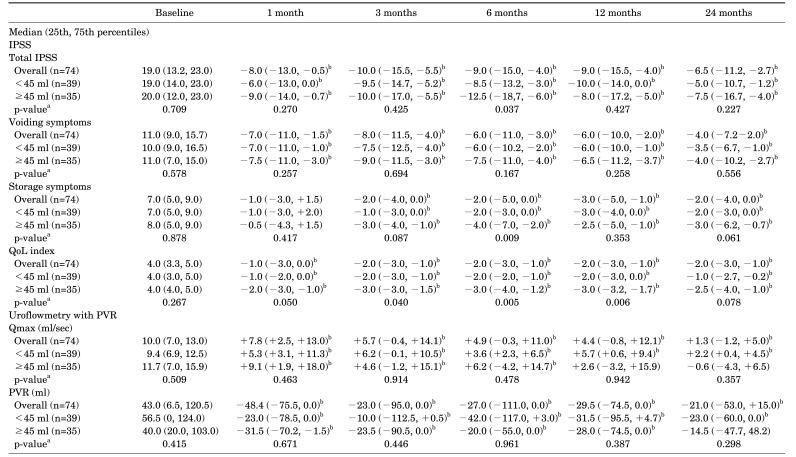

There was no significant difference in the change from baseline for the median values of the subtotal voiding symptom scores, Qmax, and PVR at 1, 3, 6, 12, and 24 months postoperatively between the two groups. However, the changes from baseline in the median values of the subtotal storage symptom scores, total IPSS at 6 months, and QoL index at 3, 6, and 12 months postoperatively were significantly higher in the larger size group than in the smaller size group (p<0.05) (
Table 2).
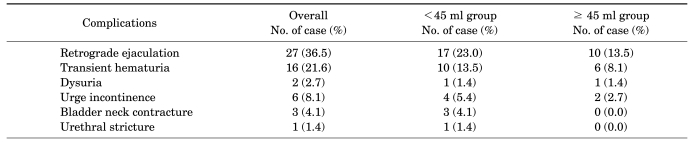
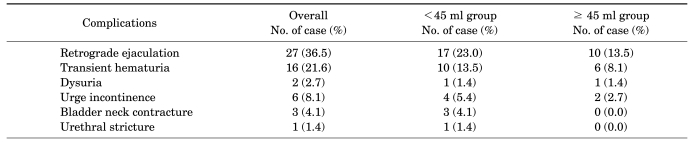
There were no serious intraoperative complications, such as intraoperative bleeding that required transfusion or TUR syndrome. Postoperative complications were 16 cases of hematuria (21.6%), 6 of urinary incontinence (8.1%), 1 of urethral stricture (2.7%), and 3 of bladder neck contracture (4.1%), with urethral stricture and bladder neck contracture occurring only in the smaller size group. In 4 cases (5.4%), complications with bladder neck contracture and urethral stricture led to urethral dilatation and endoscopic internal urethrotomy, but there was no case of re-growth of prostate tissue that led to reoperation (
Table 3).
TABLE 3
Postoperative complications

Go to :

DISCUSSION
The KTP laser belongs to the green light spectrum and is not easily absorbed by water but is absorbed by the red blood cells in tissues with plentiful blood vessels, such as in the prostate, resulting in excellent hemostatic and tissue removal effects through vaporization [
8]. The recent development of the 80 W and above KTP and LBO lasers has increased the vaporization speed dramatically and has led to an increased use of these lasers. Unlike TURP, PVP results in minimal bleeding, making endoscopic viewing possible; has little hematuria; and has a reduced time of dependency on the Foley catheter; furthermore, PVP is reported to have the same treatment effectiveness as TURP [
5-
7].
Choo et al, who presented a retrospective review over 2 years of 104 patients who received 80 W PVP-KTP for BPH, reported improvements in parameters such as IPSS, Qmax, QoL score, and PVR from 1 month after the PVP that were maintained up to 24 months postoperatively, similar to the current study [
9]. However, the number of patients reviewed by Choo et al over the 2 years progressively decreased, and they did not report for subtotal scores for the IPSS [
9].
The results of the current study showed that total IPSS, subtotal voiding symptom scores, QoL index, Qmax, and PVR were significantly improved compared with baseline starting from 1 month after the PVP, and these improvements were maintained up to 24 months postoperatively. Only the subtotal storage symptom scores showed significant improvement starting from 3 months postoperatively, and these improvements were also maintained for up to 2 years. These findings agree with existing reports that after prostatectomy, improvement in storage symptoms occurs later than that in voiding symptoms. After PVP, PVR is reduced, thus increasing the time it takes for bladder filling; this results in improvements in frequency, nocturia, and other such storage symptoms, which then leads to the resolution of obstruction [
10].
In the present study, the most common complication was retrograde ejaculation, which was observed in 27 cases (36.5%). Compared with the rate after TURP, however, the frequency of this complication was low [
4,
11]. Hwang et al reported a rate of retrograde ejaculation of 66.9% [
12], and Lee et al reported a rate of 11% [
13]. Malek et al reported that less than 26% of patients complained of retrograde ejaculation [
14], and Te et al reported that it was observed in 36% of patients [
5].
The exact reason for this difference in the incidence of retrograde ejaculation between TURP and PVP is unknown. According to Te et al, however, the reason for the lower incidence of retrograde ejaculation after PVP than after TURP may be that vaporization by laser cannot easily remove muscle fiber, thereby conserving the functionality of the bladder neck [
5]. In the case of the current study, not all patients were asked whether retrograde ejaculation developed; it was only recorded for those patients who complained of such symptoms. Therefore, the actual number suffering from retrograde ejaculation could have been higher.
In our study, there was no serious intraoperative bleeding that required transfusion or caused Foley catheter occlusion. As presented by Reich et al, even when PVP was performed on 66 patients with a high risk of cardiopulmonary functions who were taking anticoagulant medication or with hemorrhage-related illnesses, the PVP was performed safely with minimal bleeding [
15]. In cases in which bleeding is a major concern, PVP can be a valid alternative to TURP for treating BPH patients surgically.
In relation to high-volume prostates, varying views exist on the effectiveness and safety of PVP. Horasanli et al reported that TURP was a preferred treatment over PVP for large prostates on the basis of their study comparing the results of 76 randomly selected patients whose volume was over 70 cc and who underwent PVP or TURP procedures. Horasanli et al showed that although the PVP group showed a shorter duration of catheterization and hospital stay than did the TURP group, the operation time was longer; improvements in IPSS, Qmax, and PVR were less; and 7 (17.9%) of those who underwent PVP required reoperation due to re-growing prostatic tissue [
16]. Hwang et al also reported negative results of PVP used for large prostates in their study of the efficacy and safety of PVP. They showed that for prostates above 60 cc, no improvements were seen in IPSS or QoL, the duration of catheterization was longer, and the incidence of frequent urination and urgency was higher [
12].
However, Sandhu et al reported that even for large prostates, PVP is an effective treatment. In their study of 64 patients with prostate volumes of over 60 cc for 1 year after PVP, Qmax increased on average from 7.9 ml/s to 18.9 ml/s, PVR dropped from 189 ml to 109 ml, and total IPSS dropped from 18.4 to 6.7, with only 1 patient (2%) requiring reoperation [
17]. According to Choo et al, when comparisons were made between two groups based on a cutoff volume of 60 cc, there were no significant differences in IPSS, QoL index, or Qmax between the smaller and the larger size groups [
9]. However, PVR was significantly higher in the group with prostate volumes higher than 60 cc. At 12 and 24 months after PVP, the total IPSS, QoL index, Qmax, and PVR all improved in both groups compared with baseline, with total IPSS, QoL index, and Qmax showing no difference between the two groups. PVR was significantly higher in the larger size group at 12 months after PVP [
7]. However, the accuracy of this result cannot be verified because of the difference in the number of patients between the two groups (86 vs. 18) [
9]. In our study, the cutoff volume was 45 cc, which made the number of the two groups similar, and the two groups showed no significant differences in any baseline parameter. In both groups, total IPSS, subtotal voiding symptom scores, subtotal storage symptom scores, and QoL index showed significant improvements compared with baseline that lasted for up to 24 months. For Qmax at 12 and 24 months, and for PVR at 24 months after PVP, however, there were no improvements in the larger size group. This can be interpreted as selection bias due to follow-up loss occurring for those patients whose symptoms were alleviated within 1 year after the PVP. That is, only those patients whose symptoms had not improved were followed up from the original group (n=169). Subtotal voiding symptom scores, Qmax, and PVR improvements showed no significant differences between the two groups, but greater levels of improvement were seen in the larger size group for total IPSS and subtotal storage symptom scores at 6 months after PVP, and for QoL index at 3, 6, and 12 months after PVP, respectively. Operation time, applied energy, duration of catheterization, and hospital stay were all found to be significantly less in the smaller size group. In a study by Ruszat et al, in which three prostate volume groups were created on the basis of cutoffs of 40 ml and 80 ml, the group with less volume showed less improvement, which was similar to our study [
18].
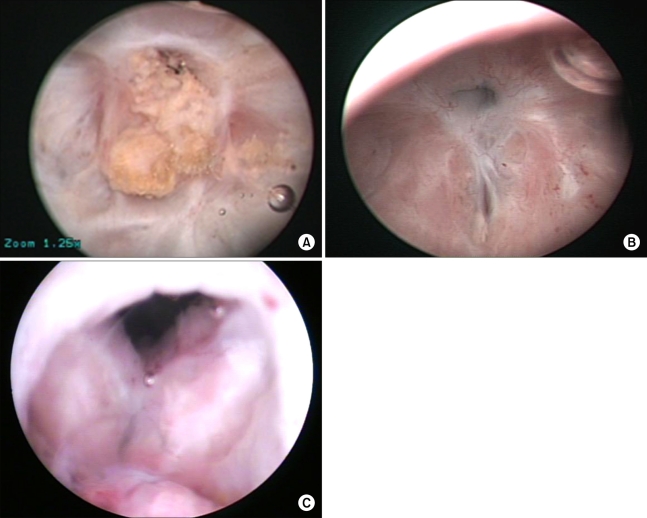
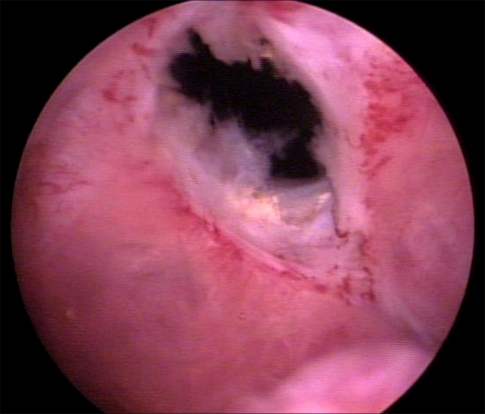
Concerning the postoperative complications that developed in the present study, there was 1 case of urethral stricture (1.4%) and 3 cases of bladder neck contracture (4.1%), with all complications being in the smaller size group. The characteristics and photographs of each bladder neck contracture are illustrated in
Figs. 1,
2, and
3. The study done by Ruszat et al showed that complications such as urethral stricture and bladder neck contracture were higher in the group with a prostate volume of less than 40 ml. The reason presented by those authors for the high number of urethral strictures in the small prostate group was that during the surgery, moving the laser scope close to the bulbomembranous urethra to preserve the sphincter could have led to mucosal injury, which then contributed to the stricture. To prevent bladder neck contracture during the PVP procedure for small sized prostates, the authors performed prophylactic bladder neck incisions [
18]; in our study, however, these types of procedures were not separately performed. In the current study, for all such complications, endoscopic interventions (urethrotomy, urethral dilatation) were performed, with the reoperation rate for complications being 5.6%. Of the complications reported by Rassweiler et al after TURP, urethral stricture was 2.2-9.8% and bladder neck contracture was 0.3-9.2%, with the reoperation rate being 3-14.5%, which is similar to the current study [
19], leading to the conclusion that the incidence of late complications is similar between the PVP and TURP procedures.
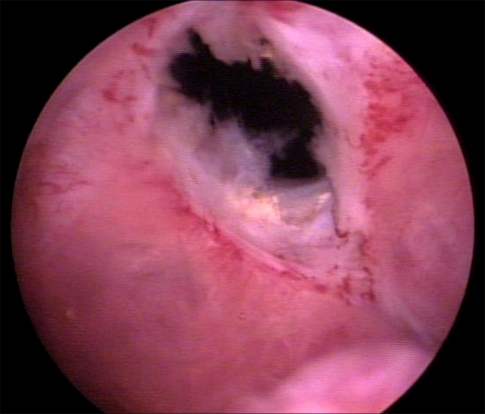
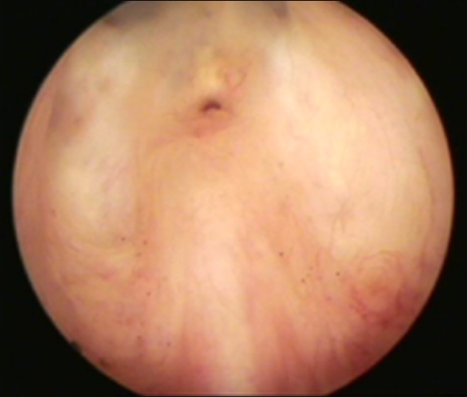 | FIG. 1Severe pin-point type BNC developed at 1 year after the PVP. After one endoscopic ureterotomy, there was no recurrence of BNC. BNC: bladder neck contracture, PVP: photoselective vaporization of the prostate. 
|
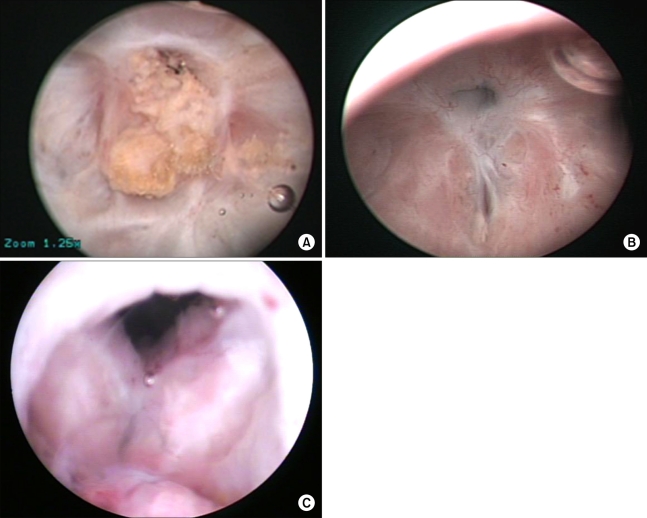 | FIG. 2BNC with an impacted urethral stone developed at 3 months after PVP (A). At 6 months after endoscopic urethrotomy and stone removal, a pin-point type BNC recurred (B). At 14 months after the 2nd endoscopic urethrotomy, multiple penile urethral strictures occurred (C). BNC: bladder neck contracture, PVP: photoselective vaporization of the prostate. 
|
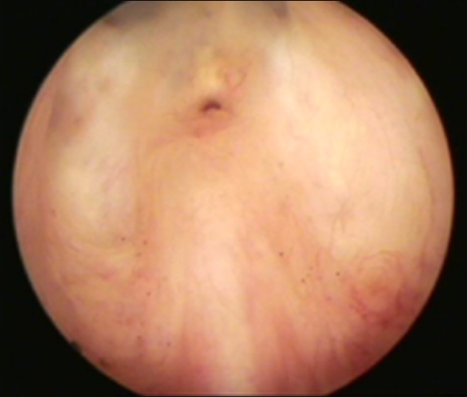
 | FIG. 3Mild BNC occurred at 6 months after the PVP. The contracture was resolved after two urethral soundation. BNC: bladder neck contracture, PVP: photoselective vaporization of the prostate. 
|
The limitations of this study include the following. First, the present study was a retrospective review only, which could have resulted in selection bias. Second, this study was based on a small cohort with a small number of cases and we reported only the mid-term results. Third, our study was not a randomized controlled study done through comparison with TURP, which is still known as the gold standard of BPH surgical management. Therefore, we cannot completely exclude the placebo effects or bias that may have affected the study results.
However, domestically, virtually no data exist on the long-term effects of PVP, which will allow the current study to be a meaningful evaluation tool and database for domestic long-term effectiveness.
Go to :





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download