Abstract
Spontaneous bladder perforation is a very rare event. Prompt diagnosis of this injury is very important, particularly with intraperitoneal perforation, because mortality increases if surgical repair is delayed. Previous studies have reported that plain cystography is the primary modality of imaging study rather than relatively insensitive computed tomography (CT) when bladder perforation is suspected. We report here a rare case of spontaneous intraperitoneal perforation of the bladder associated with urothelial carcinoma with divergent histologic differentiation, as diagnosed with CT cystography.
Go to : 
Spontaneous intraperitoneal bladder rupture associated with urothelial cancer is a rare event. Such ruptures are usually associated with infection, neurogenic bladder, bladder overdistention, or radiation therapy for various pelvic malignancies. We report here a rare case of intraperitoneal bladder perforation that showed equivocal findings on the plain cystogram and even on the excretory phase of pelvic computed tomography (CT) with adequate bladder distention but that was diagnosed by CT cystography. The perforation was associated with urothelial cancer with divergent histologic differentiation, which has been shown to be more aggressive with a high grade and advanced stage than pure urothelial cancer. The patient had acute peritonitis associated with the intraperitoneal bladder perforation, but we successfully treated him conservatively.
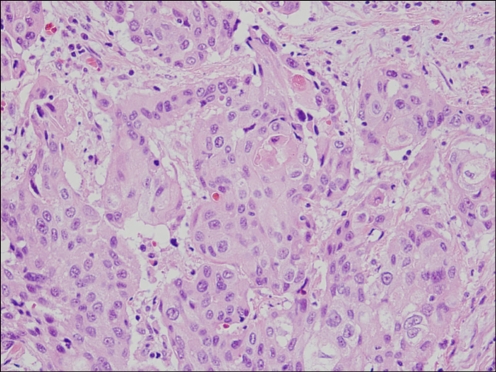
A 75-year-old male patient was emergently admitted to the hospital with gross hematuria, generalized abdominal pain, and oliguria of about 3 days' duration. He had undergone multimodal treatment for muscle-invasive bladder cancer (stage T2, urothelial cancer with sarcomatous differentiation) with transurethral resection (TUR) of the bladder tumor and 6 adjuvant cycles of cisplatin-based cytotoxic chemotherapy (gemcitabine+cisplatin) (Fig. 1), because he desired bladder preservation and had a strong fear of urinary diversion. One year after TUR, a follow-up CT scan showed bladder tumor recurrence with a focal irregular margin of the bladder wall, suggestive of perivesical invasion. So he underwent TUR of the bladder cancer (stage T2, urothelial cancer with squamous differentiation) (Fig. 2) with adjuvant chemotherapy (methotrexate, vinblastine, Adriamycin, and cisplatin).
At 10 months after the operation, he presented with acute illness with vague abdominal pain. He was febrile at 39℃. He did not have a history of recent pelvic trauma, instrumentation, pelvic radiation, infravesical obstruction due to benign prostatic hyperplasia, or episodes of acute urinary retention. On the physical exam, the abdomen was markedly distended with muscular guarding and rebound tenderness. The urinary sediment contained many white blood cells and red blood cells. The blood test showed marked leukocytosis with an acute phase inflammatory reaction. The serum creatinine (Cr) level was elevated to 5.8 mg/dl with biochemical features of acute renal failure [K 5.7 mmol/l, Na 126 mmol/l, serum blood urea nitrogen (BUN) 53 mg/dl, BUN/Cr ratio 9:1]. The spiral CT showed a large bladder tumor extending into the perivesical space with a focal bladder wall disruption. The bladder tumor was nearly in contact with the anterior rectal wall without clear demarcation. Also, both kidneys showed moderate hydronephrosis.
We therefore first suspected an invasive bladder tumor with a rectovesical fistula and performed sigmoidoscopy and plain film cystography with retrograde contrast media injection through an indwelling urethral catheter. Sigmoidoscopy showed no signs of fistula opening within the site of 70 cm from the anal verge except for a mild segmental mucosal edema. Plain film cystography showed a refractory bowel pattern to paralytic ileus and left lateral wall irregularity with a suggestive sinus tract, but no evidence of intra- or extraperitoneal contrast media extravasation (Fig. 3). Despite many imaging studies, it was difficult for us to identify the cause of the acute peritonitis and biochemical features of acute renal failure. So we finally performed CT cystography with the patient in the prone position with 50 ml megluatmine iothalamate mixed in 500 ml of normal saline. The CT cystography showed the highly attenuated fluid in the peritoneum via a disrupted left lateral bladder wall and small bowel loop pooling with contrast media (Fig. 4). However, there was no direct communication between the urinary bladder and the rectum. Considering the patient's age, poor general condition, and performance status, we decided to manage him conservatively with broad-spectrum antibiotics and indwelling catheters. A 8.5 Fr pigtail drain catheter was inserted into the right pelvic area under the guidance of fluoroscopy in addition to percutaneous nephrostomy catheters for adequate urine drainage. After the insertion of the intraperitoneal drain catheter, 150 ml of turbid, yellowish urine with pus was drained. Culture of the drained intraperitoneal fluid confirmed Enterococcus as the causative pathogen. After intervention, the patient's serum creatine level and white blood cell count returned to normal values in 4 days. The patient was discharged home with successful peritonitis resolution on hospital day 28th but died 3 months later as the result of acute renal failure.
Go to : 
Spontaneous intraperitoneal bladder perforation is a very rare clinical event and is associated with high mortality. Most spontaneous bladder ruptures occur as the result of long-term indwelling catheters, radiation, chronic cystitis, bladder distention due to infravesical obstruction, or neurogenic bladder dysfunction [1]. However, bladder perforation associated with bladder cancer is an extremely rare cause of spontaneous rupture [2,3]. Such rupture is a surgical emergency that may be rapidly fatal if its diagnosis and treatment is delayed or missed. Patients usually present with symptoms such as sudden onset of lower abdominal pain, high spiking fever, hematuria, abdominal distention with signs of peritoneal irritation, and anuria with biochemical features of acute renal failure due to auto-dialysis of urinary ascites across the peritoneum. Intraperitoneal perforation is traditionally diagnosed by plain film cystography or cystoscopy. Plain film cystography is accepted as the most accurate radiological technique for diagnosing bladder rupture. But with the widespread use of CT cystography, this imaging technique is increasingly being performed as an alternate method of diagnosing bladder rupture and has been shown to be as accurate as conventional cystography [4]. CT cystography can also distinguish the specific type of bladder rupture between extraperitoneal or intraperitoneal [5]. CT cystography has several advantages over plain film cystography: (1) it is rapid and is easily performed at the same time as other CT studies, (2) it is less affected by overlying bone fragments, and (3) it is more sensitive to the detection of small amounts of intraperitoneal or extraperitoneal fluid [6].
In the present case, even though an abdominal helical CT scan was performed with adequate bladder distention of intravenous contrast media injection, there was no evidence of intraperitoneal perforation even on the 10 minute delay scan. So we checked CT cystography with retrograde contrast media injection in the prone position and finally diagnosed that the intraperitoneal perforation was associated with invasive bladder cancer.
Urothelial carcinomas are known to demonstrate a wide range of divergent histologic differentiations into the entire spectrum of histologic variants, including squamous, glandular, micropapillary, sarcomatoid, small cell, clear cell, lymphoepithelial, and plasmacytoid components. Wasco et al found that any type or amount of divergent histologic differentiation present with urothelial carcinoma was strongly associated with unfavorable prognostic features [7]. Such cancer with mixed histologic features was nearly uniformly high grade and highly invasive and was also an independent predictor of extravesical diseases [7,8]. In our case, 2 TUR specimens showed urothelial carcinoma with sarcomatoid differentiation and squamous differentiation, respectively. Highly aggressive characteristics of urothelial cancer with divergent differentiation may explain the spontaneous bladder perforation and following early death.
In summary, we encountered a case of spontaneous intraperitoneal bladder perforation associated with highly aggressive urothelial cancer with divergent differentiation. At first, the findings of conventional helical CT and plain film cystography made it difficult for us to diagnose the intraperitoneal perforation properly. But CT cystography was very sensitive to small amounts of extravasated contrast material.
Although intraperitoneal bladder rupture is a serious condition due to increased urine leakage and subsequent systemic absorption, and prompt surgical repair is key for patient management, we managed the patient conservatively rather than by open surgical repair in consideration of his poor general condition and suboptimal prognosis [9]. We successfully treated the patient conservatively with adequate urinary diversion, intraperitoneal drainage, and broad-spectrum antibiotics.
Go to : 
References
1. Evans RA, Reece RW, Smith MJ. Idiopathic rupture of the bladder. J Urol. 1976; 116:565–567. PMID: 978806.

2. Bastable JR, De Jode LR, Warren RP. Spontaneous rupture of the bladder. Br J Urol. 1959; 31:78–86. PMID: 13651652.

3. Deck AJ, Shaves S, Talner L, Porter JR. Computerized tomography cystography for the diagnosis of traumatic bladder rupture. J Urol. 2000; 164:43–46. PMID: 10840421.

4. Holmäng S, Kleist H, Lundstam S, Borghede G. Spontaneous perforation of the bladder after external beam radiotherapy for bladder carcinoma. J Urol. 1996; 155:645. PMID: 8558686.
5. Sivit CJ, Cutting JP, Eichelberger MR. CT diagnosis and localization of rupture of the bladder in children with blunt abdominal trauma: significance of contrast material extravasation in the pelvis. AJR Am J Roentgenol. 1995; 164:1243–1246. PMID: 7717239.

6. Budd JS. Spontaneous intraperitoneal rupture of the bladder in association with transitional cell carcinoma. Postgrad Med J. 1988; 64:165–166. PMID: 3174533.

7. Skolarikos A, Chrisofos M, Ferakis N, Papatsoris A, Dellis A, Deliveliotis C. Does the management of bladder perforation during transurethral resection of superficial bladder tumors predispose to extravesical tumor recurrence. J Urol. 2005; 173:1908–1911. PMID: 15879773.

8. Wasco MJ, Daignault S, Zhang Y, Kunju LP, Kinnaman M, Braun T, et al. Urothelial carcinoma with divergent histologic differentiation (mixed histologic features) predicts the presence of locally advanced bladder cancer when detected at transurethral resection. Urology. 2007; 70:69–74. PMID: 17656211.

9. Jozwicki W, Domaniewski J, Skok Z, Wolski Z, Domanowska E, Jozwicka G. Usefulness of histologic homogeneity estimation of muscle-invasive urinary bladder cancer in an individual prognosis: a mapping study. Urology. 2005; 66:1122–1126. PMID: 16286151.

Go to : 




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download