Abstract
Purpose
We aimed to evaluate the anatomical and functional outcomes of posterior intravaginal slingplasty (P-IVS) for the treatment of a vaginal vault or uterine prolapse (VP/UP).
Materials and Methods
This was a 12-month prospective, multicenter, observational study. Women aged over 30 years who presented with stage II or greater VP/UP underwent P-IVS by four urologists at four university hospitals. Preoperatively, pelvic examination by use of the Pelvic Organ Prolapse Quantification (POP-Q) system, the Pelvic Floor Distress Inventory (PFDI) questionnaire, the 3-day frequency volume chart, and uroflowmetry were completed. At the 12-month follow-up, changes in the POP-Q, PFDI, frequency volume chart, and uroflowmetry parameters were assessed. Cure was defined as VP/UP stage 0 and improvement as stage I.
Results
The cure and improvement rates among the 32 women were 65.6% and 34.4%, respectively. All subscale scores of the Urinary Distress Inventory, the general subscale score of the Pelvic Organ Prolapse Distress Inventory, and the rectal prolapse subscale score of the Colo-Rectal-Anal Distress Inventory were significantly improved. There were no significant changes in the frequency volume chart or uroflowmetry parameters. There was one case of surgery-related transfusion.
Pelvic organ prolapse (POP) is a common condition that has a negative effect on a woman's quality of life. It is estimated that approximately 32% of the female population aged ≥18 years in Korea has some degree of POP [1]. The prevalence of any prolapse was 2.0% in women aged 20 to 29 years, but in those aged over 50 years, it increased to 57.5%. Because POP is an age-related condition, its prevalence is expected to increase with the aging of the population.
Vaginal apical prolapse, vaginal vault or uterine prolapse (VP/UP), is a complex condition commonly associated with other organ defects such as cystocele, rectocele, or enterocele in nearly 75% of affected patients [2]. The clinical presentation varies, with various effects on urinary, bowel, and sexual functions. Even if incontinence is not a presenting complaint, it must be assessed after the reduction of the prolapse with a pessary or other means of support. Thus, successful treatment for VP/UP depends not only on the restoration of the anatomical abnormality but also on comprehensive management of the combined dysfunction, including all potential vaginal support defects and urinary, bowel, and sexual dysfunctions.
The surgical management of apical prolapse requires an apical suspension procedure. For the last decades, VP/UP has been treated by several forms of trans-vaginal or trans-abdominal procedures, such as sacrospinous colpopexy or abdominal sacral colpopexy. However, morbidity and a high recurrence rate necessitated less morbid and more effective therapeutic methods. In trials of minimally invasive and less morbid surgical techniques, Petros [3] introduced infracoccygeal sacropexy with intravaginal slingplasty (Tyco Healthcare, Norwalk, USA), giving rise to posterior intravaginal slingplasty (P-IVS) based on the integral theory in 1997 [4]. The most critical aspect of this procedure is to restore the prolapsed upper vagina to a normal anatomical position by means of uterosacral ligament suspension.
We conducted the present study to evaluate the therapeutic efficacy and safety of P-IVS for restoring the anatomical defect of the VP/UP and for improving the associated pelvic floor symptoms.
A total of 40 women aged over 30 years presenting with stage ≥II VP/UP underwent P-IVS by four urologists at four university hospitals. Exclusion criteria included pregnancy or contemplating pregnancy during the study period, severe vaginal atrophy, history of pelvic irradiation therapy, and high risk for surgery. The study was performed in accordance with the principles of the Declaration of Helsinki, and written informed consent was obtained from all patients before surgery.
The baseline demographic data collected included age, body mass index (BMI), obstetric and gynecologic history, and medical and surgical history. Preoperatively, all subjects underwent a pelvic examination in the seated semilithotomy position with a Valsalva maneuver. The POP quantification (POP-Q) standard scoring system and 3x3 grid system [5] were adopted for staging and recording the 9 points of the POP-Q system. In cases presenting with lower urinary tract symptoms (LUTS), including stress urinary incontinence (SUI), a multi-channel urodynamic study was performed with reduction of the prolapse. The Pelvic Floor Distress Inventory (PFDI) score [6], 3-day frequency volume chart (FVC), and maximal flow rate (MFR) with post-void residuals (PVR) were also evaluated. At the 12-month postoperative visit, the POP-Q stage and the 9 points were evaluated to assess the anatomical results. Cure of VP/UP was defined when the postoperative POP-Q system point C was found to be stage 0, i.e., the quantitation value for point C was ≤-[total vaginal leugth (TVL)-2] cm. Improvement was defined as stage I, i.e., its quantitation value was <-1 and >-[TVL-2] cm. Failure was assigned to postoperative POP-Q stage II or greater, i.e., its quantitation value was ≥-1 cm. Surgical outcomes of the combined compartment prolapses were assessed similarly, which defined cure as stage 0, improvement as stage I, and failure as stage II or greater, as described in the POP-Q system [5]. Postoperative changes in the PFDI score, FVC, MFR, and PVR were evaluated to assess the functional outcomes. Intraoperative and postoperative complications were also evaluated.
The surgeries were performed with the patient in the lithotomy position under spinal or general anaesthesia. The procedure followed the methods introduced by Papa Petros [7] with a tunnelling device (Tyco Healthcare, Norwalk, USA) and polypropylene tape (Tyco Healthcare, Norwalk, USA). For patients who had concomitant surgeries, additional procedures were performed after closure of the P-IVS wound. Vaginal packing and a urethral catheter were left in place for 48 hours. Intravenous antibiotics were given postoperatively for 24 hours, followed by oral treatment for 14 days.
Postoperative changes in the POP-Q stage, PFDI, FVC, MFR, and PVR were evaluated. Statistical significance was determined by using a Wilcoxon signed rank test or a Student's t-test (paired) according to the normality assumption. Comparison of the outcomes between women with vault prolapse and those with uterine prolapse was performed by using the Mann-Whitney U or chi-square test. All statistical analyses were performed with SPSS 17.0 software (SPSS, Chicago, USA). A p-value of <0.05 was considered to be statistically significant.
Thirty-two of the 40 women were followed up for 12 months postoperatively. The women's average age was 56.2 years and their average BMI was 24.4 kg/m2. Eleven (34.4%) women had a prior hysterectomy (Table 1). The average time for surgery was 68.5±33.9 min [71.9±33.7 for VP and 66.7±4.5 for UP (p=0.502)]. Average hospital stay was 4.6±1.9 days [4.8±1.7 for VP and 4.5±2.1 for UP (p=0.416)]. Concomitant surgeries were performed in 21 (65.6%) women: 16 (50.0%) midurethral slings (MUS), 14 (43.7%) anterior vaginal wall repairs, 7 (21.9%) posterior colporrhaphies, and 1 hemorrhoidectomy (Table 2).
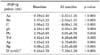
In the preoperative pelvic examination, 24 of the 32 patients (75.0%) had stage II VP/UP, 5 (15.6%) had stage III, and 3 (9.4%) had stage IV. At 12 months postoperatively, the cure rate of apical prolapse was 65.6% (21/32) and the improvement rate was 34.4% (11/32) [63.6% (7/11) for VP and 66.7% (14/21) for UP (p=1.000)]. For anterior vaginal wall prolapse, the cure rate was 68.8% (22/32) and the improvement rate was 12.5% (4/32). For posterior vaginal wall prolapse, the cure rate was 87.5% (28/32) and the improvement rate was 9.4% (3/32). During 12 months of follow-up, 6 patients had recurrent anterior prolapse and 1 had recurrent posterior prolapse. The anatomical results of the apical, anterior, and posterior prolapses are summarized in Table 3. There was no new development of anterior wall prolapse. The average level of point C changed from +1.08 (±2.72) to -6.09 (±1.16) (p<0.001). The changes in the 9 points of the POP-Q system from baseline and to 12 months postoperatively are summarized in Table 4.
After MUS for symptomatic or occult SUI, 15 of 16 women reported no leakage. No women experienced de novo SUI. In terms of the PFDI scale, the obstructive/discomfort, irritative, and stress subscale scores of the Urinary Distress Inventory were significantly improved. For the POP Distress Inventory, the general subscale score was improved but the anterior and posterior subscale scores were not significantly changed. For the Colo-Rectal-Anal Distress Inventory, only the rectal prolapse subscale score was significantly improved (Table 5). There were no statistically significant postoperative changes in the average MFR (from 15.8±8.0 ml/s to 14.6±8.1 ml/s, p = 0.379) or PVR (from 49.7±65.6 ml to 22.3±27.4 ml, p=0.230). Preoperatively, 2 patients showed an obstructive uroflowmetry pattern and 3 patients had large PVRs (≥150 ml). After successful correction of the anatomical defect, their uroflowmetry patterns returned to normal, and PVRs were reduced to less than 100 ml. Based on the 3-day FVC, frequency, nocturia, and functional bladder capacity were not significantly changed.
There was one case of increased intraoperative bleeding. One woman required transfusion with 2 pints of blood and the bleeding was controlled conservatively. No other intra- or postoperative complications were observed, including rectal or bladder perforation, wound infection, or mesh erosion.
Our study prospectively evaluated the anatomical and functional outcomes of P-IVS for apical prolapse. We reported data on 32 patients undergoing P-IVS for VP/UP. The anatomical cure rate was 65.6% and the improvement rate was 34.4% at 12 months after surgery with a success rate of 100%. In the initial preliminary results on P-IVS, success rates of over 90% were reported by Papa Petros [7] and Farnsworth [8]. In recent studies, success rates ranged from 95% to 98% with short-term and medium-term follow-up [9,10]. In a randomized controlled trial, the objective success rate of P-IVS was 95%, which was comparable to that of sacrospinous ligament fixation [11]. Regardless of how success is defined, the literature consistently shows an excellent success rate, suggesting that the P-IVS procedure is an effective treatment for restoration of the apical defect.
However, there is some evidence that the apical repair impacts the anterior vaginal wall prolapse. This is assumed to result from a change in the vaginal axis. In previous studies, a higher rate of de novo anterior wall prolapse was reported for sacrospinous ligament fixation than for other approaches such as abdominal sacral colpopexy [12,13]. During sacrospinous fixation, retroversion and fixation of the vaginal apex exposes the anterior vaginal wall to excessive pressure, which may result in the development of anterior prolapse. The incidence of postoperative anterior wall prolapse varies after sacrospinous fixation, ranging from 11% to 92% [14,15]. Such a wide range comes from the heterogeneity of the studies involved, with respect to combined surgical procedures performed in conjunction with apical repair. In a randomized controlled trial, 4.8% of the P-IVS and 25% of the sacrospinous fixation group reported having postoperative anterior vaginal wall prolapse [11]. In this study, there were 6 (18.8%) cases of postoperative recurrent anterior vaginal wall prolapse. In general, the incidence ranges from about 10% to 27% [16].
Petros and Farnsworth introduced the P-IVS as a novel procedure not only for reconstruction of the anatomical defect but also for improvement of the combined LUTS, grouped as posterior fornix syndrome [4], which comprises symptoms of frequency, urgency, nocturia, abnormal emptying, and pelvic pain. Richardson and colleagues [17] also reported that POP causes bladder outlet obstruction by increasing the urethral closure pressure and that women with POP would be expected to manifest an obstructed voiding pattern. Therefore, in assessing the outcomes of the prolapse surgery, functional outcomes should be evaluated in conjunction with the anatomical result. Although functional or symptomatic outcomes of prolapse surgery have been reported in a few articles, those studies often used nonstandardized assessment tools. In our study, LUTS were evaluated by means of a disease-specific questionnaire, FVC, and uroflowmetry. In terms of the PFDI, all of the obstructive, irritative, and stress symptoms were significantly improved after surgery. Also, the uroflow pattern was improved and PVRs were reduced in women with a preoperative obstructive uroflow pattern or large PVRs after successful correction of their anatomical defect. These results show that functional outcomes are correlated with anatomical success.
De novo SUI is one of the outcomes that is evaluated in the study of POP. Even though it is impossible to measure the effect of P-IVS on SUI owing to combined anti-incontinence surgeries, the incidence of de novo incontinence after P-IVS was reported in 0% to 5% of women [9,18,19]. Concomitant anti-incontinence surgeries were performed in most of the patients in our study. Postoperatively, none of our patients complained of de novo incontinence. One of 16 patients who received concomitant MUS reported persistent SUI after the surgery. It is suggested that massive vaginal prolapse may cause functional urethral obstruction and mask an incompetent continence mechanism. Following correction of the prolapse, SUI may occur or persist. Therefore, examination for potential SUI with reduction of the prolapse is important and necessary before POP surgery.
In sexually active women, postoperative vaginal shortening and sexual function should be considered when choosing the surgical options for apical prolapse, especially in patients who had a prior hysterectomy. Although sexual function was not evaluated, our study showed no significant change in the total vaginal length after surgery (from 8.4 cm to 8.2 cm, p=0.197). In general, sexual dysfunction or dyspareunia is associated with the traditional posterior colporrhaphy combined with an extensive levator ani plication due to constriction of the vaginal tube. Approximately 5% of women in whom the uterus was removed reported dyspareunia, whereas no women reported the symptom when the uterus was preserved during P-IVS [20,21].
There were no complications in our study except for one case of increased intraoperative bleeding in a woman with UP. She underwent combined surgeries for cystocele and SUI and received two pints of blood. Her hemoglobin level was 10.9 g/dl at the preoperative evaluation and dropped to 8.4 g/dl on the postoperative follow-up test 2 days after surgery. She had no symptoms and there was no hematoma or bleeding on the physical exam. Pelvic ultrasonography showed a small hematoma around the posterior bladder neck. In a review paper, the rate of transfusion after P-IVS was estimated to be 0% to 0.3% [22]. According to the Austrian registry, 7 of 577 (1.2%) patients were reported to have increased intraoperative bleeding [19]. This complication is more related to the concomitant surgeries, especially hysterectomy, than to the procedure of P-IVS [18,19]. Although hematomas requiring reoperation were reported in 0.9% of cases [19]; generally, the bleeding could be managed conservatively without surgical intervention [10,18,19].
Reported complications after P-IVS include mesh erosion in 8%, dyspareunia in 2%, followed by hematoma in 1%. Other complications include prolonged pain, blood transfusion, proctotomy, pararectal abscess, and fistula [23]. In terms of the mesh used in the P-IVS procedure, the nylon mesh initially used was replaced with polypropylene multifilament mesh as the result of high rates of erosions. Farnsworth [8] first reported an erosion rate of 10% with nylon tape, and the erosion rate was dropped to 0% after he started using polypropylene mesh. We used polypropylene multifilament mesh and there was no mesh erosion. The absence of mesh erosion in our study may have been due to insertion of the mesh under the rectovaginal fascia and the short follow-up period. According to the data of Luck et al, there was an 18% incidence of mesh erosion and it occurred late in the postoperative period [9]. Thus, our small study population and the short follow-up period, which were the main limitations of the current study, might have resulted in an underestimate of the rate of long-tem complications. Compared with the recently released Prolift system (Ethicon Women's Health and Urology, Somerville, USA), the mean mesh-related complication rate of P-IVS was lower, presumably because of the smaller amount of mesh used [23].
Another limitation of this study was that the outcomes were not only for P-IVS but also for the surgeries conducted in conjunction with P-IVS. Combined surgeries might confound the results. A stratified analysis is needed to eliminate such confounding factors. However, this study was under-powered to conduct stratified analysis and to detect differences in outcomes.
Figures and Tables
References
1. Seo JT, Kim JM. Pelvic organ support and prevalence by Pelvic Organ Prolapse-Quantification (POP-Q) in Korean women. J Urol. 2006. 175:1769–1772.
2. Richter K. Massive eversion of the vagina: pathogenesis, diagnosis, and therapy of the "true" prolapse of the vaginal stump. Clin Obstet Gynecol. 1982. 25:897–912.
3. Petros PE. New ambulatory surgical methods using an anatomical classification of urinary dysfunction improve stress, urge and abnormal emptying. Int Urogynecol J Pelvic Floor Dysfunct. 1997. 8:270–277.
4. Petros PE, Ulmsten UI. An integral theory and its method for the diagnosis and management of female urinary incontinence. Scand J Urol Nephrol. 1993. 153:Suppl. 1–93.
5. Bump RC, Mattiasson A, Bo K, Brubaker LP, DeLancey JO, Klarskov P, et al. The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am J Obstet Gynecol. 1996. 175:10–17.
6. Barber MD, Kuchibhatla MN, Pieper CF, Bump RC. Psychometric evaluation of 2 comprehensive condition-specific quality of life instruments for women with pelvic floor disorders. Am J Obstet Gynecol. 2001. 185:1388–1395.
7. Papa Petros PE. Development of generic models for ambulatory vaginal surgery--a preliminary report. Int Urogynecol J Pelvic Floor Dysfunct. 1998. 9:19–27.
8. Farnsworth BN. Posterior intravaginal slingplasty (infracoccygeal sacropexy) for severe posthysterectomy vaginal vault prolapse--a preliminary report on efficacy and safety. Int Urogynecol J Pelvic Floor Dysfunct. 2002. 13:4–8.
9. Luck AM, Steele AC, Leong FC, McLennan MT. Short-term efficacy and complications of posterior intravaginal slingplasty. Int Urogynecol J Pelvic Floor Dysfunct. 2008. 19:795–799.
10. Neuman M, Lavy Y. Posterior intra-vaginal slingplasty for the treatment of vaginal apex prolapse: medium-term results of 140 operations with a novel procedure. Eur J Obstet Gynecol Reprod Biol. 2008. 140:230–233.
11. de Tayrac R, Mathe ML, Bader G, Deffieux X, Fazel A, Fernandez H. Infracoccygeal sacropexy or sacrospinous suspension for uterine or vaginal vault prolapse. Int J Gynaecol Obstet. 2008. 100:154–159.
12. Benson JT, Lucente V, McClellan E. Vaginal versus abdominal reconstructive surgery for the treatment of pelvic support defects: a prospective randomized study with long-term outcome evaluation. Am J Obstet Gynecol. 1996. 175:1418–1421.
13. Paraiso MF, Ballard LA, Walters MD, Lee JC, Mitchinson AR. Pelvic support defects and visceral and sexual function in women treated with sacrospinous ligament suspension and pelvic reconstruction. Am J Obstet Gynecol. 1996. 175:1423–1430.
14. Nieminen K, Huhtala H, Heinonen PK. Anatomic and functional assessment and risk factors of recurrent prolapse after vaginal sacrospinous fixation. Acta Obstet Gynecol Scand. 2003. 82:471–478.
15. Holley RL, Varner RE, Gleason BP, Apffel LA, Scott S. Recurrent pelvic support defects after sacrospinous ligament fixation for vaginal vault prolapse. J Am Coll Surg. 1995. 180:444–448.
16. Morgan DM, Rogers MA, Huebner M, Wei JT, Delancey JO. Heterogeneity in anatomic outcome of sacrospinous ligament fixation for prolapse: a systematic review. Obstet Gynecol. 2007. 109:1424–1433.
17. Richardson DA, Bent AE, Ostergard DR. The effect of uterovaginal prolapse on urethrovesical pressure dynamics. Am J Obstet Gynecol. 1983. 146:901–905.
18. Vardy MD, Brodman M, Olivera CK, Zhou HS, Flisser AJ, Bercik RS. Anterior intravaginal slingplasty tunneller device for stress incontinence and posterior intravaginal slingplasty for apical vault prolapse: a 2-year prospective multicenter study. Am J Obstet Gynecol. 2007. 197:104.
19. Bjelic-Radisic V, Hartmann G, Abendstein B, Tamussino K, Riss PA. The posterior intravaginal slingplasty operation: results of the Austrian registry. Eur J Obstet Gynecol Reprod Biol. 2009. 144:88–91.
20. Jordaan DJ, Prollius A, Cronje HS, Nel M. Posterior intravaginal slingplasty for vaginal prolapse. Int Urogynecol J Pelvic Floor Dysfunct. 2006. 17:326–329.
21. Neuman M, Lavy Y. Conservation of the prolapsed uterus is a valid option: medium term results of a prospective comparative study with the posterior intravaginal slingoplasty operation. Int Urogynecol J Pelvic Floor Dysfunct. 2007. 18:889–893.
22. Dietz V, Schraffordt Koops SE, van der Vaart CH. Vaginal surgery for uterine descent; which options do we have? A review of the literature. Int Urogynecol J Pelvic Floor Dysfunct. 2009. 20:349–356.
23. Feiner B, Jelovsek JE, Maher C. Efficacy and safety of transvaginal mesh kits in the treatment of prolapse of the vaginal apex: a systematic review. BJOG. 2009. 116:15–24.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download