INTRODUCTION
In recent years, endoscopic subureteral transurethral injection (STING) has become a first-line therapy for children with vesicoureteral reflux (VUR) because of its high success rates and few complications [1].
Debate over the ideal bulking agent in endoscopic therapy for children with VUR remains controversial, however [2,3]. The substance should be nontoxic, biocompatible, nonmigratory, and nonantigenic and should cause minimal local inflammation. Many bulking agents have been used to treat reflux, including polytetrafluoroethylene, collagen, autologous injectables, polydimethylsiloxane (Macroplastique®; Uroplasty, Minnetonka, USA), and dextranomer/hyaluronic acid copolymer (Deflux®; Oceana Therapeutics, Inc, Edison, USA).
Among these agents, Macroplastique is one of the most popular bulking agents and is used extensively in medical applications. Macroplastique, a nonbiodegradable substance, is reabsorbed and exchanged with a reactive transudate containing fibroblasts that then facilitate its encapsulation. Deflux was introduced in 1995 by Stenberg and Läckgren [4] and was approved by the Food and Drug Administration in 2001 as an acceptable implant for subureteral injection for VUR in children. Deflux represents a new biocompatible material without immunogenic properties and a lack of distant migration. Previous studies indicated high success rates of 68% to 90% with endoscopic injection using Macroplastique or Deflux [5-7].
This is the first study by a single surgeon in Korea to compare outcomes and complications of these two agents for endoscopic treatment of VUR in children.
MATERIALS AND METHODS
Between April 2001 and March 2008, 71 children (29 boys and 42 girls; 115 ureters) who underwent endoscopic subureteral injection with Macroplastique (from April 2001 to February 2004) or Deflux (from March 2004 to March 2008) for VUR were retrospectively evaluated.
Families were provided with information reflecting our current knowledge of VUR management. All families were counseled regarding the natural history of VUR with respect to resolution rates, based on grade of VUR, and the risks and benefits of antibiotic use, open surgery, and subureteral injection therapy [8]. All patients underwent preoperative renal and bladder ultrasonography, voiding cystourethrography (VCUG), and dimercapto-succinic acid (DMSA) renal scans. Reflux grades were evaluated according to the reflux grading system recommended by the International Reflux Study [9]. The indications for surgery included breakthrough infections during antibiotic prophylaxis, renal scarring, and persistent reflux. Exclusion criteria included duplicated refluxing ureters, neurogenic bladder determined by history, and failed surgical reimplantation.
The children's mean age was 6.2 years (range, 1.2-10.5 years). The mean period of follow-up was 26 months (range, 12-42 months). A single subureteral injection of Macroplastique (group I) was performed in 23 children (31 ureters; grade II: 4; grade III: 12; grade IV: 9; grade V: 6), and Deflux (group II) was used in 48 children (84 ureters; grade II: 24; grade III: 14; grade IV: 25; grade V: 21).
All procedures were performed by a single operator with the children in the lithotomy position under general anesthesia. Ureteral orifices were visualized by using a 9.5 Fr Wolf pediatric cystoscope. The 3.7 Fr needle was placed within the submucosa of the ureter at the 6 o'clock position, and Macroplastique or Deflux was injected inside the lumen of the ureter until an adequate subureteric mound was attained [10]. The mean amount of each substance injected into the ureter was 1.1 ml (range, 0.5-1.5 ml) in group I and 1.3 ml (range, 0.5-2.0 ml) in group II. The amount of each substance injected into the ureter was determined according to reflux grade or shape of the ureteral orifice.
Renal ultrasonography for detection of urinary obstruction was performed 1 day after injection. All patients were discharged 1 day after the operation. All patients underwent VCUG, ultrasonography, and urine culture from 3 months after discharge. Thereafter, basic laboratory studies (complete blood count with differential count, blood urea nitrogen, creatinine, urine analysis, gram stain, and culture) and renal ultrasonography were followed up annually. Follow-up VCUG was performed in children with recurrent urinary tract infection or newly developed hydronephrosis. Successful reflux correction was defined as absent or grade I reflux on follow-up VCUG [11].
Statistical analysis was performed by using SPSS statistical software, version 13.0 (SPSS Inc, Chicago, USA). Chi-square tests were used for data analysis. A value of p-value<0.05 was considered significant.
RESULTS
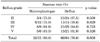
No significant difference in baseline characteristics (mean age, gender, reflux grade) were observed between group I and group II. The overall success rate after a single injection was 80.6% (25 of 31) for group I. VUR disappeared in 75.0% (3 of 4) for grade II, 75.0% (9 of 12) for grade III, 88.9% (8 of 9) for grade IV, and 83.3% (5 of 6) for grade V. Persistent grade I reflux was found in 1 patient. The success rate of group II was 78.6% (66/84). VUR disappeared in 87.5% (21/24) for grade II, 78.6% (11/14) for grade III, 84.0% (21/25) for grade IV, and 61.9% (13/21) for grade V. Persistent grade I reflux was found in 2 patients. There was no significant difference in cure rates between the two groups (p>0.05) (Table 1).
No intraoperative complications were noted. Postoperative ureteral obstruction was found in 2 patients (6.4%) after Macroplastique injection and in 3 patients (3.6%) after Deflux injection. Postoperative obstruction was diagnosed by renal ultrasonography 1 day after injection. Children with postoperative ureteral obstruction had symptoms that included flank pain, elevated creatinine levels, and aggravated or newly developed hydronephrosis. Following Deflux injection for bilateral VUR, one child required percutaneous ureteral stent placement, due to postoperative ureteral obstruction with serum creatinine level elevation, whereas others required no intervention. Following ureteral stent placement, the serum creatinine level decreased and hydronephrosis disappeared. We placed a percutaneous ureteral stent for 12 days and removed it after the hydronephrosis disappeared on follow-up renal ultrasonography.
Three (9.6%) patients in group I and two (2.4%) patients in group II had postoperative asymptomatic urinary tract infection during the follow-up period after successful injection therapy. These patients showed no recurrence of reflux on follow-up VCUG, nor did they show newly developed renal cortical defects on the DMSA renal scan.
Bladder calcification due to Macroplastique exposure from bladder mucosal necrosis or erosion was found in two patients at the 30- and 36-month follow-ups, and one patient underwent endoscopic removal.
DISCUSSION
The concept of subureteral injection was introduced by O'Donnell and Puri in the 1980s to create a less invasive treatment for VUR [12]. Endoscopic treatment is based on the principle of creating a solid support behind the intravesical ureter and elongating the intramural length of the ureter [13]. Many studies have reported that endoscopic treatment is effective and safe as a first-line therapy for VUR; however, the ideal agent has not yet been identified [14,15].
In 2002, Oswald et al reported on a comparison of a single endoscopic STING of Macroplastique versus Deflux for treatment of VUR in children [11]. Reflux was corrected in 86.2% of the Macroplastique group and in 71.4% of the Deflux group at the 3-month follow-up visit. Reflux correction was maintained in 80.9% of the Macroplastique group and in 67.6% of the Deflux group at 1 year of follow-up. No postoperative complications were observed in either group. Our success rate, 80.3% of group I and 78.6% of group II, is consistent with these data. Also, there were no significant differences in cure rate between the grades in the two groups (p>0.05). The success rate for grade V of group II was lower than that of group I (61.9% vs. 83.3%). However, the success rate was increased up to 67.8% after the second injection in group II.
Previous studies have indicated success rates of 70% to 90% by endoscopic injection using Macroplastique, and a recent meta-analysis reported a success rate of 76.6% [15]. Studies to date have demonstrated single-injection cure rates from 68% to 86.1% with endoscopic injection using Deflux [7,14,16]; however, long-term follow-up studies using Deflux show that its long-term success rate is less than that of Macroplastique.
Rates of local complications after the injection of endoscopic bulking agents are remarkably low. In particular, ureteral obstruction occurred in less than 1% of injected ureters using Macroplastique [17]. In our study, one child (1.2%) required percutaneous ureteral stent placement after Deflux injection for bilateral VUR. The rate of ureteral obstruction in our study is consistent with published data.
In an earlier study, Puri and Guiney described a series of 11 patients with neurogenic bladder, one of whom developed new hydronephrosis after the injection [18]. This patient also had a dysmorphic-appearing ureter on preoperative imaging. A decade later, Misra et al retrospectively reviewed their experiences with 51 children (69 ureters) with neurogenic bladder, one of whom (2%) developed ureteral obstruction requiring reimplantation [19]. Al-Hunayan et al observed a single case of symptomatic obstruction following polydimethylsiloxane injection [17]. However, they noted that an "excess amount" of substrate was injected in this case, and the obstruction was attributed to this factor. No further risk factors were identified. The injected Deflux volume was 3 ml in each ureter in the child with ureteral obstruction.
Bladder calcification due to Macroplastique exposure from bladder mucosal necrosis or erosion was found in 2 patients at 30 and 36 months of follow-up. Children with bladder calcification had microscopic hematuria. Because Macroplastique is a nonbiodegradable substance, the risk of bladder calcification is increased after correction because of the increased pressure and diminished perfusion of the overlying mucosa [20]. On the other hand, animal studies have demonstrated formation of a well-encapsulated foreign body reaction at the injection site, composed of giant cells, fibroblasts, and collagen, with no substantial risk of migration [21]. Development of bladder mucosal necrosis from Deflux exposure is also a possibility; however, because of the biodegradable nature of Deflux, spontaneous healing may occur. Long-term follow-up of patients injected with Macroplastique is required because of the risk of bladder mucosal necrosis.
To the best of our knowledge, we have reported on the first trial in Korea to compare two different bulking agents with regard to success rates and complications. However, several limitations of this study merit discussion. First, this study was not a prospective, randomized trial because of different introduction times for bulking agents in Korea. The success rate of STING with each bulking agent may have been affected by surgical technique before achievement of the learning curve because is the procedure was performed by a single surgeon. Second, we did not perform additional VCUG after successful injection therapy, other than for patients with asymptomatic urinary tract infection and bladder calcification. Deflux is a biodegradable material and, in animal studies, hydrolysis of dextranomer microspheres has been identified as the likely cause of decreased implant volume [22]. Because microspheres constitute 50% of the volume of Deflux, substantial decreases in volume after implantation may be anticipated. However, ingrowth of fibroblasts and production of endogenous collagen between microspheres appeared to occur, thus stabilizing implant volume, and the 12 month volume reduction in rats was 23% [22]. Such volume stability undoubtedly has an important role in maintaining the long-term efficacy of Deflux in humans [7].
CONCLUSIONS
Cure rates and complication rates did not differ significantly between Macroplastique and Deflux after a single endoscopic subureteral injection. Both Macroplastique and Deflux were safe materials for the treatment of VUR with few complications. However, long-term follow-up of patients injected with Macroplastique and Deflux is required because of the risk of bladder mucosal necrosis and substantial decreases in volume after implantation.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download