Abstract
Purpose
This study was designed to objectively assess the impediment of incontinence to quality of life (QoL) in females and its improvement by the midurethral sling (MUS) procedure.
Materials and Methods
From June 2006 to June 2007, 93 female patients underwent the MUS procedure at our institute because of urinary incontinence. The incontinence quality of life (I-QoL) questionnaire was administered to measure the QoL of the incontinent patients before and 1 and 12 months after the MUS procedure. Preoperative data and urodynamic factors were analyzed retrospectively by I-QoL scores to identify factors that may affect the QoL of incontinent patients.
Results
The average preoperative I-QoL score of the 93 patients was 61.1±21.0 points. At 1 year after surgery, the average I-QoL score was found to have improved to 98.4±20.7 points. There were no significant differences between stress and mixed urinary incontinence in terms of cure and satisfaction (p>0.05). I-QoL scores of the cured and improved patients increased at 1 year after surgery (p<0.01). There were no statistically significant differences in the increment of I-QoL between cured and improved patients (p>0.05). Although urinary urgency and large urine leak amounts significantly reduced preoperative QoL in incontinent patients, the MUS procedure effectively improved the QoL regardless of these factors.
The surgical technique of the midurethral sling (MUS) procedure is much simpler than previous anti-incontinence surgeries, and the procedure can be performed under local anesthesia. The success rate of the procedure is reported to have reached 90% [1-4]. Interlocked with the increase in social interest in urinary incontinence and in social activities of aged women, these advantages of the MUS procedure have resulted in an explosive increase in operations for female urinary incontinence.
Most previous reports regarding MUS outcomes generally tended to investigate only patients' subjective satisfaction, but recent reports have strived to systematically observe improvement in quality of life (QoL) by means of objective methods.
We intended to investigate the impact of the MUS procedure on not only cure and satisfaction with the surgery but also on the objective QoL of incontinent patients. In addition, we intended to define clinical and urodynamic factors that affect the QoL of female patients with urinary incontinence.
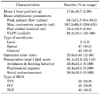
Between June 2006 and June 2007, 118 consecutive female patients with a complaint of urinary incontinence underwent the MUS procedure by a single operator in our institute. Because the QoL of patients who had failed previous anti-incontinence surgery can differ from that of patients who had not undergone an operation previously, the former group was excluded. Of the 118 patients, 93 patients (Mean±SD age, 54.5±10.2 years) received follow-up tests at 1 month and 1 year after surgery and responded to the I-QoL questionnaire [5]. The remaining 25 patients who did not respond for follow-up tests were excluded.
Preoperative evaluations included a medical history, I-QoL questionnaire, obstetric history, and physical examination including Q-tip test, stress test, 3-days' voiding diary, 1-hour pad test, and multi-channel urodynamic investigation. Urodynamic studies were performed according to the standards of the International Continence Society [6]. The analysis of urodynamic parameters included peak urinary flow, maximum cystometric capacity, post-void residue (PVR), and Valsalva leak-point pressure (VLPP).
Each of the procedures [tension-free vaginal tape (TVT), intravaginal slingplasty (IVS), and transobturator sling (TOT)] was performed by a single experienced surgeon using the standard technique. Anesthesia was selected from among a combination of light sedation with local anesthesia, spinal anesthesia, or general anesthesia after consultation with the patients and according to their general health status.
All patients were asked to visit the clinic at 1 month and 1 year after surgery. At those times, they were evaluated with a careful symptom review, stress test, I-QoL questionnaire, uroflowmetry, and PVR measurement and for postoperative complications. Questions about satisfaction with the procedure were completed by the patient.
The I-QoL questionnaire consisted of 22 questions [7]. The total score was the sum of all questions (range, 0-110). A low total score meant that the patient was deeply troubled; on the other hand, higher scores meant that the patient was less burdened. The I-QoL questionnaire consisted of three subscales: avoidance and limiting behavior (AL), psychosocial impacts (PI), and social embarrassment (SE). A formula was used to calculate the subscale scores. The subscale scores focus on patients' bothersome problems and may help in counseling. The subscale formula was as follows:
*Subscale score (range: 0-100)=[(The sum of the items-lowest possible score)×100/[(highest possible score-lowest possible score)]
Cure of urinary incontinence was defined as the absence of any episodes of involuntary urine leakage during stressful activities and a stress cough test. The cough test was performed with the patient in a standing position with a full bladder. Improvement was defined subjectively as a significant reduction of urine leakage, such that it did not require further treatment [8]. All other outcomes were regarded as failures. Patients were classified as "satisfied," "so-so," and "dissatisfied," for the assessment of satisfaction after surgery. Urgency was defined as a sudden compelling desire to pass urine that was difficult to defer. Mixed urinary incontinence (MUI) was defined as complaint of an involuntary leakage of urine associated with urgency and also with symptoms of stress urinary incontinence (SUI).
We analyzed clinical and urodynamic factors to determine which preoperative and intraoperative factors influenced cure and satisfaction by MUS for urinary incontinence. Univariate analysis was performed by using Fisher's exact and chi-square tests. To determine predictive factors affecting cure and satisfaction, univariate analysis was performed by using logistic regression analysis. Both "so-so" and "dissatisfied" were sorted as "not satisfied" for the analysis of satisfaction.
Student's t-test was used to determine which clinical symptoms and urodynamic factors affected the QoL of the incontinent patients. A 5% level of significance was used for all statistical testing, and all statistical tests were two-sided. Analysis was performed by using the statistical software SPSS (14.0KO for windows, Release 14.0.2).
On the basis of the Stamey grading system, the number of female patients with grade I incontinence was 74 (79.6%), the number with grade II was 14 (15.1%), and the number with grade III was 5 (5.4%). The average operation time was 23.9±6.45 minutes. Clinical and urodynamic data and results from the preoperative tests are shown in Table 1 and Table 2.
In the preoperative assessment of I-QoL, the total I-QoL score and subscale points (AL, PI, and SE points) were 61.1±21.0, 45.9±23.4, 48.4±26.2, and 34.9±26.5 points, respectively. At 1 month after surgery, the I-QoL scores were higher than preoperatively (89.0±17.9, 75.1±16.7, 79.0±20.9, and 72.1±24.1 points, respectively; p<0.01). At 1 year, I-QoL scores were higher than at 1 month (98.4±20.7, 83.7±24.9, 89.8±22.8, and 86.5±24.5 points, respectively; p<0.05) (Fig. 1).
At 1 year after surgery, 67.7% of patients were rated as "cured", 87.1% as "cured and improved", and 71.0% as "satisfied." There was no significant difference between SUI and MUI in terms of cure and satisfaction (p>0.05) (Table 3). Preoperative average I-QoL scores of "cured", "Improved", and "failed" patients were 62.7±21.7, 56.7±17.2, and 66.2±22.1 points, respectively. I-QoL scores at 1 year after surgery were 107.7±4.3, 94.7±7.3, and 54.6±7.3 points, respectively. I-QoL scores of the cured and improved patients increased at 1 year after surgery (p<0.01). There were no statistically significant differences in the increase in I-QoL between cured and improved patients (p>0.05). Patients in whom the operation had failed did not show any improvement of QoL after the procedure (p>0.05) (Fig. 2).
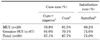
Patients who had urgency or large amounts of urine leakage (more than 10 g in a 1 hour pad test) before surgery showed lower total I-QoL scores than did patients without urgency or with small amounts of leakage (p<0.05).
At 1 year after surgery, total I-QoL and the increase in the I-QoL score of the patients who had large amounts of urine leakage preoperatively were higher than in the patients with small amounts of leakage (p<0.01) (Table 4).
Medical reports on the success rates or treatment effects of various treatments have been precisely performed with objective methods. Reports about QoL and patient satisfaction after treatment, however, generally tend to rely on only simple subjective measures. Recently, many medical reports have strived to objectively observe the QoL associated with disease and its change after treatment. Accordingly, several questionnaires have been developed and used in the field of female urology, including urinary incontinence. Many questionnaires for assessment of QoL in urinary incontinence are being used internationally after proper official linguistic validation; typical questionnaires include the I-QoL and the King's Health Questionnaire [9]. The I-QoL questionnaire, which was used in the present study, was recommended most preferentially at the 2nd International Consultation on Incontinence for assessing the QoL of patients with urinary incontinence [10].
Papanicolaou et al assessed the negative impact of urinary incontinence on QoL in female European patients through use of the I-QoL questionnaire [11]. They reported that the I-QoL scores of patients with "low grade" or "middle or high grade" incontinence were 84.5 and 64.5 points, respectively, and that decreases in the I-QoL score of incontinent patients were significantly dependent on symptom grade [11]. In several studies of the MUS procedure, the I-QoL questionnaire has been used to assess the QoL of incontinent patients and changes in QoL after the procedure. Campeau et al reported an increment of 38.7 points in the I-QoL after the TVT procedure (from 57.8 to 96.5 points) [2], and Kim et al reported an increment of 32.9 points in the I-QoL after the IVS procedure (from 61.5 to 94.4 points) [3]. Also, Kocjancic et al reported an increment of 40 points in the I-QoL after the TOT procedure (50.6 to 90.6 points) [12]. Scores in our study at 1 year after the MUS procedure showed an increment of more than 30 points in the I-QoL from the preoperative state (61.1 to 98.4 points). Our study included all patients who underwent the TVT, IVS, and TOT procedures. Because there are differences in approach and in the types of mesh used in each type of MUS procedure, however, objections to the design of our study may arise. However, many articles have observed that there are no differences in cure or satisfaction between each type of MUS [13,14].
The Stamey grades of the patients in this study tended toward grade I and II. Because the success rate of the MUS procedure in patients with Stamey grade III incontinence is lower than that in patients with grade I and II, grade III patients received the REMEEX system [15] procedure if indicated. This was the reason for the inclination in Stamey grade.
In this study, the significant rise in I-QoL at 1 month and 1 year after surgery can be shown as gradual improvement in QoL as time elapsed after the procedure. At 1 month after surgery, however, surgical wound pain, temporary vaginal bleeding or discomfort caused by vaginal discharge may affect QoL. Because patients are prohibited from sexual intercourse for 1 month after surgery, question no. 22 on the I-QoL about sexual intercourse may cause confusion. Therefore, in order to observe the changes in the QoL by time more accurately, the first postoperative I-QoL assessment should be measured at least 3 months after surgery.
In this study, patients who had urgency or large amounts of urine leakage before surgery showed lower total I-QoL scores than did patients without urgency or with small amounts or urine leakage. However, this difference in I-QoL scores was no longer evident after the procedure. Higher I-QoL and increment of I-QoL scores were observed at 1 year after surgery in patients with large amounts of urine leakage. It may be that patients with large amounts of urine leakage were severely bothered by their symptoms and experienced a higher satisfaction with the MUS procedure, resulting in a larger increase in 1-year I-Qol. Our finding of no difference in the average increase in I-Qol between the cured and improved groups implies that simply improving symptoms through MUS considerably enhances the QoL of incontinent patients. Therefore, for the improvement of QoL, the MUS procedure should be actively applied in incontinent patients, even in patients with urgency or large amounts of urine leakage.
The I-QoL assessment revealed a significant impairment of QoL in incontinent women compared with that in continent women without voiding symptoms, but the MUS procedure effectively improved these women's QoL.
Although urinary urgency and large amounts of urine leakage significantly reduced the preoperative QoL in patients with urinary incontinence, the MUS procedure effectively improved the QoL regardless of these factors. Even the QoL of patients with only symptom improvements and who were still incontinent showed significant recovery; therefore, the MUS procedure should be actively applied to improve QoL in incontinent patients, even in women with urgency or large amounts of urine leakage.
Figures and Tables
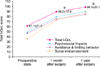 | FIG. 1Changes in the total I-QoL and I-QoL subscale scores before and after surgery. I-QoL: incontinence-quality of life, a: p<0.01, b: p<0.05. |
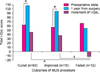 | FIG. 2Comparison of the total I-QoL score between before surgery and at 1 year of follow-up (sorted by objective operation results). I-QoL: incontinence-quality of life, MUS: midurethral sling, a: p<0.01. |
References
1. Campeau L, Tu LM, Lemieux MC, Naud A, Karsenty G, Schick E, et al. A multicenter, prospective, randomized clinical trial comparing tension-free vaginal tape surgery and no treatment for the management of stress urinary incontinence in elderly women. Neurourol Urodyn. 2007. 26:990–994.
2. Kim JC, Chung BS, Choi JB, Lee JY, Lee KS, Park WH, et al. A safety and quality of life analysis of intravaginal slingplasty in female stress incontinence: a prospective, open label, multicenter, and observational study. Int Urogynecol J Pelvic Floor Dysfunct. 2007. 18:1331–1335.
3. Choo MS. Recent trends in the surgical treatment of female stress urinary incontinence. Korean J Urol. 2004. 45:509–517.
4. Song PH, Hyun CH, Lim HS, Jung HC. Five-year outcomes of the IRIS procedure for the treatment of female stress urinary incontinence: comparison with the TVT procedure. Korean J Urol. 2009. 50:767–773.
5. Wagner TH, Patrick DL, Bavendam TG, Martin ML, Buesching DP. Quality of life of persons with urinary incontinence: development of a new measure. Urology. 1996. 47:67–71.
6. Abrams P, Blaivas JG, Stanton SL, Andersen JT. The standardisation of terminology of lower urinary tract function. The International Continence Society Committee on Standardisation of Terminology. Scand J Urol Nephrol Suppl. 1988. 114:Suppl. 5–19.
7. Oh SJ, Park HG, Lim SH, Hong SK, Kim SW, Kim HH, et al. Translation and linguistic validation of Korean version of the incontinence quality of life (I-QoL) instrument. J Korean Continence Soc. 2002. 6:10–23.
8. Stamey TA. Endoscopic suspension of the vesical neck for urinary incontinence in females. Report on 203 consecutive patients. Ann Surg. 1980. 192:465–471.
9. Kelleher CJ, Cardozo LD, Khullar V, Salvatore S. A new questionnaire to assess the quality of life of urinary incontinent women. Br J Obstet Gynaecol. 1997. 104:1374–1379.
10. Donovan J, Bosch R, Corcos J, Gotoh M, Kelleher C, Naughton M. Abrams P, Cardozo L, Khoury S, Wein A, editors. Symptom and quality of life assessment. Incontinence. 2002. 2nd ed. Plymouth: Health Publication;267–316.
11. Papanicolaou S, Hunskaar S, Lose G, Sykes D. Assessment of bothersomeness and impact on quality of life of urinary incontinence in women in France, Germany, Spain and the UK. BJU Int. 2005. 96:831–838.
12. Kocjancic E, Crivellaro S, Oyama IA, Singla A, Ranzoni S, Carone R, et al. Transobturator tape in the management of female stress incontinence: clinical outcomes at medium term follow-up. Urol Int. 2008. 80:275–278.
13. Meschia M, Pifarotti P, Bernasconi F, Magatti F, Vigano R, Bertozzi R, et al. Tension-free vaginal tape (TVT) and intravaginal slingplasty (IVS) for stress urinary incontinence: a multicenter randomized trial. Am J Obstet Gynecol. 2006. 195:1338–1342.
14. Chene G, Tardieu AS, Cotte B, Chauleur C, Savary D, Krief M, et al. Health-related quality of life in women operated on by surgical anti-incontinence procedures: comparison of three techniques. Gynecol Obstet Fertil. 2009. 37:3–10.
15. Iglesias X, Espuña M. Surgical treatment of urinary stress incontinence using a method for postoperative adjustment of sling tension (Remeex System). Int Urogynecol J Pelvic Floor Dysfunct. 2003. 14:326–330.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download