INTRODUCTION
Benign prostatic hyperplasia (BPH) is one of the most common diseases in men of middle age and over in Korea. Its importance and frequency are rapidly increasing as the result of increases in the elderly population, increases in the accessibility of westernized diets, increases in desires for improvements in quality of life, and other medical, social, and economical changes [
1]. Treatment methods are also continuously changing. The early treatment chosen most often for BPH is pharmacotherapy, but it is not appropriate for some patients. When the side effects of pharmacotherapy, such as dry mouth and orthostatic hypotension, are severe, patients may choose surgical treatment instead. Also, in cases accompanied by repetitive urinary tract obstruction, infection, bladder stone, renal failure, and gross hematuria, surgery is considered first rather than medical therapy [
2]. Up to now, transurethral resection of the prostate (TURP) was the standard surgical method [
3], but TURP can have complications such as postoperative bleeding, urethral stricture, urinary incontinence, retrograde ejaculation, and transurethral resection (TUR) syndrome. [
4]. Photoselective vaporization of the prostate (PVP) by use of a laser was attempted as a minimally invasive treatment in order to reduce these side effects. Recently, PVP using an 80 W potassium-titanyl-phosphate (KTP) laser or 120 W lithium triborate (LBO) laser, which produces high energy, has been introduced and used. According to several studies, the treatment effects of PVP are similar to those of TURP. PVP was also reported to significantly reduce operation time, hospitalization period, and urethral Foley catheter indwelling duration and to reduce complications by reducing the amount of bleeding [
5-
7]. However, additional studies on the application range of PVP are required. In particular, the operation time becomes longer and complication rates increase after the operation compared with TURP if the prostate size is large. Enforcing PVP in this case is still controversial [
8,
9]. Still, because most previous studies dealt with patients with large prostates and analyzed the surgery results by comparison with TURP, it is not clear whether PVP results differ depending on prostate volume [
6,
8,
10-
13]. Therefore, in the present study, we divided patients who underwent PVP at our hospital into 2 groups: those with prostate volumes of less than 60 cc and those with volumes of 60 cc or greater. The two groups were compared in order to examine the utility and stability of PVP depending on prostate volume.
Go to :

MATERIALS AND METHODS
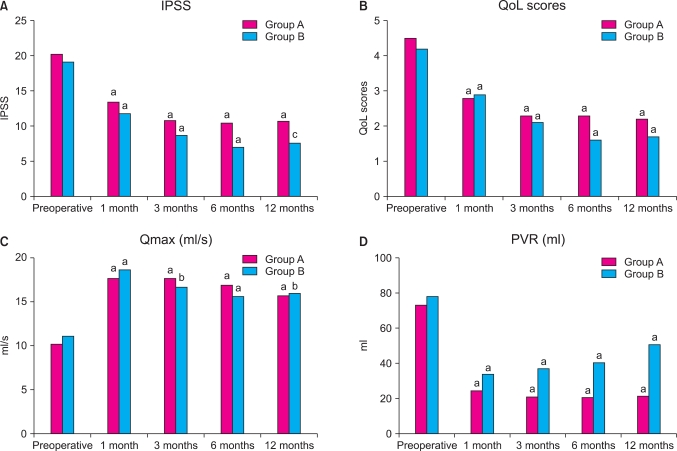
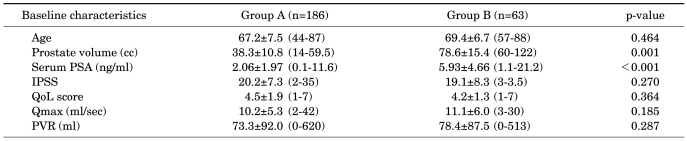
A total of 249 patients with a chief complaint of lower urinary tract obstruction due to BPH and who underwent PVP with an 80 W KTP laser or a 120 W LBO laser at two general hospitals from January 2006 to June 2008 were chosen as the subjects for this retrospective study. For comparison and analysis, the subjects were divided into group A, with prostate volumes of less than 60 cc, and group B, with prostate volumes of 60 cc or more, on the basis of transrectal ultrasonography performed before surgery. All patients underwent history taking, physical examination, transrectal ultrasonography, and a blood test for prostate-specific antigen (PSA) before surgery. Patients with palpable nodes on the digital rectal exam or with PSA levels over 4 ng/ml before surgery underwent prostate tissue biopsy to confirm the existence of prostate cancer. Those diagnosed with prostate cancer were excluded from the study. Patients showing a neurogenic bladder in the urodynamic studies or those with urinary tract infection or urethral stricture were also excluded. Indications for surgery were an International Prostate Symptom Score (IPSS) of 12 points or more before surgery and a maximal urinary flow rate (Qmax) lower than 15 ml/s, acute urinary tract obstruction, hydronephrosis or uremia, repetitive urinary tract infection due to excessive residual urine, bladder stone, and severe hematuria. Questionnaires to assess IPSS and quality of life (QoL) score and tests for examining Qmax and postvoid residual volume (PVR) were completed before surgery and 1, 3, 6, and 12 months after surgery. For the test items right after surgery, the total amount of energy used (kJ) and Foley catheter maintenance period were compared.
The operation was done with monitored control anesthesia for all patients. Under the guide of videoendoscopy, a 22.5 Fr continuous flow cystoscope with a 30° lens was used. An 80 W KTP laser or a 120 W LBO laser with a wave-length of 532 nm was used through a 6 Fr side-deflecting optical fiber. Normal saline (0.9%) was used as the irrigating solution. The size and maintenance period of the urethral Foley catheter applied after surgery were determined by considering the surgical findings and level of hematuria after surgery. Most patients had 20 Fr three-way Foley catheters, which were removed in the morning of the next day after surgery.
Results for treatment effects were evaluated with IPSS, QoL score, Qmax, and PVR, whereas stability was evaluated through operation time, Foley catheter maintenance period after surgery, hospitalization period, urethral stricture, and urinary tract infection. Statistical management was analyzed by using the Korean version of SPSS 12.0. Comparison between the two groups was done by Student's t-test. Preoperative and postoperative baseline values of continuous variables were compared by paired t-test. Relationship with complications due to prostate volume was examined by using the chi-square test. Each statistical value was determined to have a significant difference when the p-value was less than 0.05.
Go to :

DISCUSSION
The standard surgical treatment for BPH up until now has been TURP. However, TURP is associated with a risk of bleeding during surgery and complications such as TUR syndrome. The procedure requires a few days of Foley catheter insertion and hospitalization even after surgery. Other complications such as hematuria, urinary tract obstruction, retrograde ejaculation, urethral stricture, and urinary incontinence may occur. Therefore, interest has recently arisen in nonsurgical therapy and minimally invasive treatment. Among these, endoscopic treatment using a laser is known to have treatment effects similar to those of TURP but with fewer side effects. Many studies have been done on this issue [
5-
7].
The KTP and LBO lasers that are being commonly used at present all correspond to the green optical spectrum of 532 nm. They are not easily absorbed in water but are very soluble in hemoglobin. Because they are absorbed in the red blood cells in tissues with abundant blood vessels such as the prostate, they show excellent tissue removal and hemostatic effects through evaporation [
14]. Owing to these characteristics, PVP with lasers is associated with less bleeding during surgery than is TURP. It also secures a better endoscopic view, less hematuria occurs after surgery, and the Foley catheter maintenance period can be minimized. Reports continuously announce that the treatment effects of PVP are the same as after TURP [
5-
7].
However, some controversy exists about the application range and side effects of PVP. In particular, these opinions arise in cases of large prostates. Horasanli et al conducted a prospective randomized comparison study of PVP and TURP among 76 patients with prostate volumes over 70 cc [
8]. The group that received PVP showed a shorter period of Foley catheter maintenance and shorter hospitalization period than did the TURP group. However, operation time was longer and the patients showed less improvement in IPSS, Qmax, or PVR. Also, 7 patients (17.9%) among those who received PVP had to undergo surgery again. Thus, Horasanli et al reported than TURP was better than PVP in cases of large prostates. Sandhu et al, by contrast, conducted a 1-year follow-up study of 64 patients with prostate volumes of more than 60 cc who received PVP [
10]. At 1 year after surgery, Qmax increased from an average of 7.9 ml/s to 18.9 ml/s, PVR changed from 189 ml to 109 ml, and IPSS decreased from 18.4 to 6.7. Only one patient (2%) underwent surgery again within 1 year. The study concluded that PVP was also an effective treatment method for large prostates.
In Korea, Hwang et al reported treatment effects and complications of PVP depending on prostate volumes [
9]. According to their study, there were no improvements in IPSS or QoL scores for prostates of 60 cc or more. The Foley catheter maintenance period was longer and urinary frequency and urgency occurred more. Therefore, Hwang et al were opposed to enforcing PVP in patients with large prostates. Meanwhile, Choo et al conducted a 2-year follow-up study after PVP in 104 patients [
11]. When analyzing the results by a prostate volume cutoff of 60 cc, 86 patients with volumes less than 60 cc showed an increase of Qmax from an average of 8.3 ml/s to 14.2 ml/s at 2 years after surgery. Their PVR decreased from 72.3 ml to 45.8 ml, IPSS from 22.6 to 9.9, and QoL scores from 4.4 to 2.3. Eighteen patients with prostate volumes of 60 cc or more showed an increase of Qmax from an average of 8.3 ml/s to 15.5 ml/s, a decrease in the PVR from 128.4 ml to 71.9 ml, a decrease in IPSS from 21.5 to 9.7, and a decrease in QoL scores from 4.3 to 2.6 at 2 years after surgery. Our study also compared clinical indexes of IPSS, QoL score, Qmax, and PVR among patients with prostate volumes of less than 60 cc or 60 cc or more. All of these indexes showed statistically meaningful improvement like that in cases with prostate volumes less than 60 cc. We thus confirmed that PVP is an effective treatment for those with large prostates.
Among the clinical indexes, PVR showed a statistically significant increase in both groups A and B when preoperative values were compared with values 12 months after surgery. However, the PVR in group A was similar after surgery, whereas that in group B increased as time went by. This difference was statistically significant. Even so, it is difficult to determine whether this was a general propensity depending on prostate size because other urination indexes did not differ significantly by time. Only 26 (41.3%) patients were followed up to 12 months. The possibility of their PVR being relatively more can be considered. Sandhu et al also confirmed that PVR increased at 12 months after surgery, but statistical significance was not mentioned [
10]. More studies may be required to additionally analyze the relation of PVR with prostate volume.
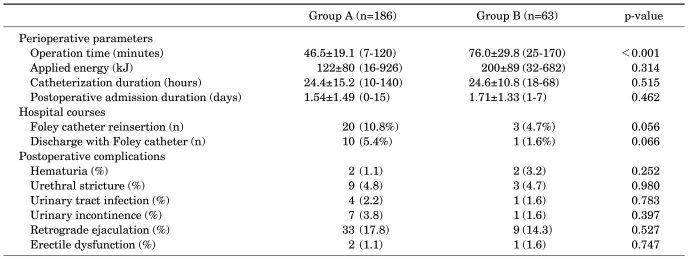
In this study, we observed a statistically significant difference in average operation time and the amount of energy used depending on prostate size. However, no statistically significant differences were seen in the Foley catheter maintenance period, hospitalization period, or Foley catheter reinsertion between the two groups. This is the same result that Lee et al reported from a study of PVP results in 38 patients with prostate volumes of 40 cc or more [
15]. Because 0.3-0.5 cc of prostate is evaporated per minute by PVP, the operation time and energy increased with prostate volume. Meanwhile, bleeding did not increase in larger prostates owing to the excellent hemostatic effects of the KTP laser. Hematuria and urinary tract obstruction did not occur, so prostate volume was not considered to have a significant effect on the Foley catheter maintenance period, hospitalization period after surgery, or Foley catheter reinsertion.
As for complications after surgery, retrograde ejaculation and urinary stricture occurred the most but there were no statistically significant differences depending on prostate size. The incidence of retrograde ejaculation is being reported differently [
5-
13,
15]. This may be because retrograde ejaculation cannot be evaluated objectively and is recognized only when a doctor asks at the outpatient clinic or when the patient complains about his symptoms. Nine (4.8%) patients in the group with prostate volumes less than 60 cc and 3 patients (4.7%) in the group with prostate volumes of 60 cc or more had urethral stricture. All patients underwent endoscopic internal urethrotomy and are receiving follow-up at the outpatient clinic without any other problems. The incidence of urethral stricture after PVP is also reported differently in different studies [
5-
13,
15]. This study is not any different from previous studies. However, whereas Hwang et al reported a high incidence of urethral strictures in patients with large prostates, it appeared that prostate volume did not affect the incidence of urethral strictures in our study [
9]. Long-term, large-scale analysis and research may be required on this subject in the future.
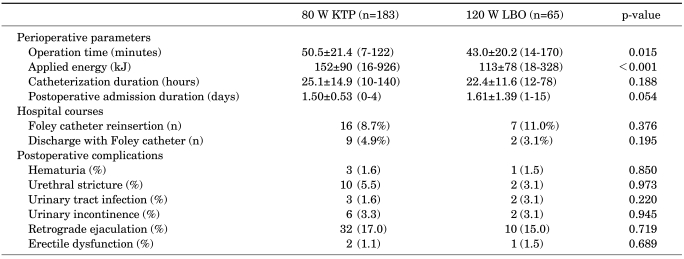
In the present study, we analyzed patients who underwent PVP with an 80 W KTP laser or a 120 W LBO laser. The surgical devices and methods used were almost identical, and there were no differences in preoperative or postoperative management. It may be difficult to understand why some items, including operation time, were completely the same because the output energy differed. However, we conclude that the final treatment results were identical because PVP with both lasers was carried out until an appropriate cavity was formed, like TURP, and analysis of stability and usefulness could be done as well. The supply of 120 W LBO lasers is increasing, so studies of only patients who received PVP with a 120 W LBO laser will become possible [
7].
Up until now, TURP was the gold standard for prostatic hypertrophy [
3]. If long-term follow-up results with various clinical data are sufficiently gathered instead of short-term results on PVP [
16-
18], we will be able to better evaluate the advantages and disadvantages of PVP compared with TURP.
Go to :





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download