Urothelial carcinoma of the upper urinary tract accounts for 5% of all urothelial malignancies [1]. Radical nephroureterectomy with an ipsilateral bladder cuff is the gold standard therapy for upper-tract cancers. However, a number of investigators have reported favorable outcomes with more conservative surgical approaches in appropriately selected patients. These conservative approaches were initially applied to patients with a solitary kidney, renal insufficiency, or bilateral tumors, but the indications were later extended to include patients with a normal contralateral upper tract. Selected patients with a normal contralateral kidney who have small, low-grade lesions might also be candidates for endoscopic ablation of ureteral transitional cell carcinoma (TCC). Distal ureterectomy is an option for patients with high-grade, invasive, or bulky tumors of the distal ureter not amenable to endoscopic management [2]. In appropriately selected patients, outcomes following distal ureterectomy are similar to those of radical nephroureterectomy [2]. When ureteral length is insufficient for direct reimplantation, additional length can be gained with either a psoas hitch or a Boari flap.
The first robot-assisted laparoscopic radical prostatectomy was performed in 2005 in Korea [3]. Since then, robot systems have been used for other surgeries in the field of urology, including partial nephrectomy, radical nephrectomy, radical cystectomy, nephroureterectomy, and pyeloplasty [3]. We investigated the feasibility of robot-assisted distal ureterectomy and ureteral reconstruction for urothelial carcinoma. To the best of our knowledge, robot-assisted distal ureterectomy and ureteral reimplantation has not been previously reported in Korea. We describe our technique for robot-assisted laparoscopic distal ureterectomy and ureteral reimplantation.
CASE REPORT
1. Case
A 74-year-old man visited because of total painless gross hematuria. On physical examination, there were no specific abnormal findings, including costovertebral angle (CVA) tenderness. His vital signs, such as blood pressure, pulse rate, and body temperature, were normal. The results of a preoperative evaluation, including liver function test, chest X-ray, and cystoscopy, were normal, but malignant cells were seen in urine cytology. The upper urinary tract was evaluated with a computed tomography (CT) scan and post-CT KUB. The CT scan showed suspicious enhancing wall thickening in the distal ureter, and post-CT KUB showed left hydronephroureterosis with distal ureteral obstruction (Fig. 1). On the preoperative ureteroscopic examination, a solitary papillary ureteral lesion was found in the distal ureter and there was no bladder lesion. A ureteroscopic biopsy confirmed high-grade urothelial carcinoma.
2. Surgical technique
The patient was placed in the lithotomy position with both legs tightly secured in boot holders. The patient was placed in a Trendelenburg position of approximately 30° to allow the bowels to fall back and open the pelvic cavity. Pneumoperitoneum was achieved by the open Hasson technique with a 10 mm blunt tip trocar (Tyco, Norwalk, USA) in the umbilical region. Two 8 mm robotic instrument ports were placed at the lateral edge of the rectus muscle at the level of the umbilicus on each side, and a 5 mm port was placed two finger widths above the right anterior superior iliac spine for the assistant (Fig. 2). The robot was then docked over the patient. The laparoscope was positioned on the da Vinci robot with the 30 lens angled downward.
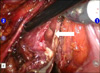
Dissection was started at the point where the left ureter crossed the iliac vessels, and the ureter was mobilized proximally and was encircled with a vessel loop for traction. The ureteral mass was grossly identified, and then direct contact with the tumor was avoided. Before the urinary tract was entered, Hem-o-lok clips were placed on the ureter, distal and proximal to the tumor, to prevent tumor spillage. For distal ureterectomy, the ureter was dissected distally to include a cuff of bladder (Fig. 3). The bladder was opened immediately adjacent to the ureter. The bladder cuff was excised sufficiently including the ureteral orifice. Proximally, the ureter was then transected 1 cm above the mass. The specimen was placed in an entrapment bag and retrieved, and the proximal margin was examined by frozen section analysis. After the ureterectomy with bladder cuff excision, the opening in the bladder was closed in three layers with absorbable suture.
Bladder reimplantation was performed at a site that is amenable for future upper-tract access, because recurrence rates are not insignificant. The external tunnel method of ureteral reimplantation was performed by making an opening in the bladder and performing an anastomosis to a spatulated ureter. A running anastomosis was then created between the bladder and the spatulated ureter with 4-0 Vicryl suture (Fig. 4). A double-J stent was then placed through a 5 mm port before completing the ureteric re-implantation. An ipsilateral regional pelvic lymphadenectomy was performed from the bifurcation of the common iliac artery to the node of Cloquet. An intraperitoneal drain was placed at the conclusion of the procedure. The ureteral stent was left in place for 6 weeks.
Total operative time was 207 minutes and estimated blood loss was 30 ml. The final pathologic result was high-grade, muscle-invasive urothelial carcinoma. The resected longitudinal ureteral length was about 3.8 cm, and the tumor size was about 1.9 cm. The proximal and distal ureteral resection safety margin from the tumor was 0.9 cm, respectively, and there were no positive lymph nodes. On the fifth hospital day, the patient was discharged home. He was doing well without disease recurrence after 12 months of follow-up.
DISCUSSION
The treatment of choice for TCC of the distal ureter remains controversial. Although the gold standard for urothelial tumors involving the upper urinary tract has been complete excision of the entire kidney and ureter, distal ureterectomy with reimplantation is a reasonable alternative for patients with high-grade, invasive, or bulky tumors of the distal ureter that are not amenable to endoscopic ablation. Preservation of the ipsilateral renal moiety is particularly advantageous for patients with borderline renal function who might require adjuvant cisplatin-based chemotherapy regimens. It is essential to exclude the presence of concurrent proximal ureteral or renal pelvic disease, which would necessitate a complete nephroureterectomy.
In recent years, urologic surgery has been advanced toward the direction of less-invasive surgery, while the principle of open surgery is still observed. Laparoscopic surgeries have several advantages, including shorter length of hospital stay due to faster recovery, cosmetic factors, and lower risk of developing postoperative complications. Laparoscopic surgeries have also been used for the management of ureteral and renal pelvic tumors. Laparoscopic radical nephroureterectomy is now offered routinely in many centers. In addition to malignant pathology, laparoscopic techniques have been used for benign ureteral conditions, such as distal strictures, iatrogenic injuries, and endometriosis [4-6].
Nevertheless, reconstructive urologic surgery remains largely performed by open techniques. One of the reasons for this is the technical demands faced by the surgeon in undertaking a reconstructive procedure laparoscopically, a complexity that is reflected in the lengthy operative times reported to date.
Symons et al reported through their own experience and literature review that laparoscopic ureteral reimplantation is a feasible procedure with good functional short-term outcomes in benign ureteral strictures [7]. However, they said that the creation of both the ureteroneocystotomy and Boari flap require advanced laparoscopic skills, and a definite learning curve exists in mastering such techniques. In addition to reports in benign ureteral strictures, the technique of laparoscopic ureteral reimplantation has now been extended to malignant disease. Laparoscopic ureterectomies have previously been reported for a distal ureteral tumor as well as for a proximal ureteral tumor. Roupret et al reported six patients who underwent laparoscopic distal ureterectomy and anastomosis for urothelial carcinoma [8]. Two patients needed a psoas hitch in their series.
The use of the da Vinci surgical robot offers certain advantages over both open and conventional laparoscopic surgery. These include three-dimensional vision, prevention of tremors, and accurate mobility provided by the wristed instruments. For these reasons, robot assistance has been applied to a broad range of areas including prostatectomy, pyeloplasty, partial nephrectomy, cystectomy, and donor nephrectomy. Uberoi et al first described the technique for robot-assisted distal ureterectomy [9]. They reported using a Collings knife to score the mucosa surrounding the ureteral orifice to facilitate resection of the bladder cuff. In that report, the robot simplified the intracorporeal suturing necessary for the psoas hitch and ureterovesical anastomosis. The better visibility achieved by the magnification and stereotactic vision allowed precise dissection of the intramural ureter, leaving a small bladder defect that often can be left open or, if necessary, closed with a single stitch. Glinianski et al reported that all patients in their series had a tumor in the distal half of the ureter [10].
In robot-assisted and laparoscopic surgery for malignancies, tumor seeding is a concern. Glinianski et al recommended that care be taken to avoid spillage of the tumor [10]. When performing segmental ureteral resections, the ureters were tied both proximal and distal to the tumor before excising the diseased segment. In our case, Hem-o-lok clips were applied on the ureter, distal and proximal to the tumor, to minimize urine spillage during the dissection, which was similar to a technique used by other authors.
Owing to the rarity of upper-tract TCC, there are no definitive data supporting the use of lymph node dissection. Most conclusions about the therapeutic benefit of lymphadenectomy are extrapolated from bladder TCC data, which suggest that the number of lymph nodes removed and the lymph node density are important prognostic variables in patients undergoing cystectomy with pathologic evidence of lymph node metastases [2]. Distal ureteral tumors metastasize to pelvic nodes, and an ipsilateral pelvic lymphadenectomy should be conducted for distal ureteral tumors [2]. According to these references, we performed ipsilateral regional pelvic lymphadenectomy, and the final pathology result showed no positive lymph nodes.
With regard to intraoperative data, our operative time and estimated blood loss were 207 minutes and 30 ml, respectively. These were comparable to the 252 minutes (range, 100-432) and 44 ml (range, 20-100) reported by Glinianski et al [10].
In summary, our case and a review of the literature indicate that distal ureterectomy with ureteroneocystostomy can safely be performed robotically. As the availability of the surgical robot increases, surgeons should be open to novel applications of this technological advancement, with the goals of improving patient outcomes and reducing patient morbidity.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download