Abstract
Purpose
We assessed sexual function by using a questionnaire in women who were diagnosed with stress urinary incontinence and underwent mid-urethral tape sling surgery.
Materials and Methods
A retrospective survey was conducted of 151 women without evidence of detrusor overactivity or concomitant prolapse who underwent surgery (tension-free vaginal tape or tension-free vaginal tape-obturator) for stress urinary incontinence. The participants filled out a questionnaire regarding their preoperative and 6-month postoperative sexual function. Paired t-tests were used to compare changes over time. The generalized McNemar test was used to compare individual preoperative and postoperative findings. We considered a p-value less than 0.05 as significant.
Results
Of the 303 women who fulfilled the inclusion criteria, 204 (67.3%) returned the questionnaire. Of those 204 women, 151 were sexually active before and after surgery. No significant differences were observed after surgery in the frequency or appreciation of intercourse or the extent of sexuality. A significant reduction in leakage symptoms was observed after surgery (p<0.01). Of the 151 women, 29 (19.2%) reported an improvement in satisfaction with intercourse and 23 (15.2%) reported a deterioration after the anti-incontinence procedure. Partner discomfort remained unchanged. Of the 151 patients, 26 (17.2%) patients were unsatisfied with the surgical outcome because of persistence or recurrence of stress urinary incontinence and deterioration in satisfaction with intercourse after surgery.
Urinary incontinence is common in the female population. Female stress urinary incontinence (SUI) is known to affect psychological, social, and sexual function [1,2]. Mid-urethral tape sling operations such as tension-free vaginal tape (TVT) and transobturator tape (TOT) outside-in or inside-out have been performed on patients with stress incontinence during the last 10 years [3-5]. The effects of these procedures on a woman's sexual function remain poorly studied, however, with most efforts focusing on the cure of incontinence and its morbidity. Improvement could be related to the emotional amelioration resulting from the cessation of incontinence. In contrast, deterioration could occur from organic causes, such as fibrosis, stenosis, neuronal or vascular damage to the anterior vaginal wall and clitoral region after vaginal surgery, and placement of artificial material under the mid-urethra.
However, currently, there is no consensus on the changes in sexual function before and after SUI surgery. There are contradictory reports, with some suggesting a deterioration of sexual function [6,7], some an improvement [8-11], and others no change [12-17]. We examined the changes in sexual function after a mid-urethral tape sling operation and investigated the causes of such changes.
This retrospective survey included all women who had undergone TVT, TOT, or other mid-urethral tape sling operation for the treatment of SUI at the Department of Urology at Catholic University of Korea from January 2000 to December 2007. Patients were excluded from the study if they had any the following: (1) underwent anti-incontinence surgery; (2) a past history of pelvic surgery; (3) prolapse of the pelvic organ, urethral stricture, urethral diverticulum, or bladder neck contracture, etc; (4) spinal cord lesion; (5) urinary tract infection or diabetes; or (6) no evidence of detrusor overactivity or voiding dysfunction. The patient's sexual function was assessed with questionnaires that were based on one of Lemack and Zimmern and other questionnaires that have been previously used in retrospective and prospective studies [8,18,19]. Sexually inactive patients were asked to state the reason in the questionnaire (Appendix). Also, menopausal status, use of hormone replacement therapy, interval from surgery to sexual activity, and satisfaction with the surgery were assessed. All patients were mailed the questionnaire after surgery, as well as an introductory letter stating the purpose of the study. For some patients who sent incorrect or inadequate answers by mail, we rechecked or completed the questionnaire over the phone.
All data are presented as Means±SDs, and the SPSS program for PC was used for data analysis. Statistical analysis was performed by the application of Fisher's exact test, McNemar test, paired t-test, and unpaired t-test. A p-value less than 0.05 was considered as significant.
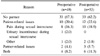
Of 303 women who fulfilled the inclusion criteria, 204 patients (67.3%) returned the questionnaire. Of those, 151 patients maintained sexual activity both before and after surgery. The baseline demographic and clinical parameters are shown in Table 1.
Among the respondents, 53 women (26.0%) were sexually inactive before and after surgery, and the reasons for their sexual inactivity are shown in Table 2. The focus of this report was on the 151 women who were sexually active both before and after surgery. The answers to the questionnaire are summarized in Tables 3 and 4. A total of 89.4% of the patients were sexually active within 8 weeks after surgery. There were no significant differences in the frequency of sexual relationships, appreciation of sexual intercourse, or the extent of sexuality. On the other hand, incontinence during sexual activity was significantly decreased after surgery (p<0.01).
Among the 151 patients who were sexually active, 29 patients (19.2%) reported an improvement in sexual satisfaction, 99 patients (65.6%) reported no change, and 23 patients (15.2%) reported deterioration. Among the 23 patients who reported a deterioration, 9 patients presented with new dyspareunia, 7 patients reported an aggravation of dyspareunia, and the remaining 7 patients did not answer. Among the 151 patients who were sexually active, 26 patients (17.2%) were dissatisfied with the surgical outcome, of whom 10 patients reported a continuation or recurrence of incontinence, 4 patients reported dysuria symptoms, 7 patients reported a deterioration in intercourse satisfaction, and the remaining 5 patients gave no answer to the cause of dissatisfaction with the surgical outcome. Age was not related to changes in sexual satisfaction (Fig. 1).
Total 151 patients who maintain sexual activity were compare by the sexual satisfaction outcome depend on each operation type. After TVT, 13 patients answered better than usual, 20 answered worse, and 61 answered that there was no change. After TOT, 10 patients answered better than usual, 9 answered worse, and 38 answered that there was no change. By all accounts, the type of surgical technique was not related to changes in sexual satisfaction (Fig. 2). Other factors such as menopausal status, use of hormonal therapy, previous hysterectomy history, type of surgery, and presence of coital incontinence were not related to satisfaction with intercourse.
Anti-incontinence surgery has been widely performed to cure SUI in the past 10 years; nonetheless, studies about the effect of these procedures on sexual function, which constitutes an important part of quality of life, are limited. Sexual excitement is dependent on the thickness and congestion of the vaginal wall or level of secretion of mucus or lubricants, etc [20,21]. These functions may deteriorate when vaginal surgery such as a mid-urethral sling operation is performed, because of narrowing of the vaginal lumen, scar formation, or tape erosion. Furthermore, the mid-urethral sling operation incises the anterior vaginal wall, which has abundant neurovascular bundles.
In addition, fibrosis may develop around the pudendal nerve, which terminates in the vicinity of the pubocervical fascia surrounding the urethra after incontinence surgery, resulting in difficulty in achieving orgasm [22]. Consequently, pain caused by dryness and other problems may result in these patients or their partners. On the other hand, with the disappearance of incontinence during intercourse, improvement of the hygienic condition of the genital organs can lead to satisfied sexual function [10].
Studies on sexual function after the mid-urethral sling operation are limited. Jha et al reported that surgical correction of incontinence was related to improvements of sexual function (TVT, 43 patients; TOT, 11 patients) [11]. In this study, comparison between TVT and TOT was not performed because the number of TOT surgeries was small. Murphy et al examined changes in sexual function in patients who underwent TVT and TVT-O in 36 and 103 patients, respectively [16]. In that study, sexual function did not differ significantly between the two surgical techniques. However, only 1.9% of patients showed a deterioration of sexual function after TVT-O, whereas 8.3% showed a deterioration after TVT. Caruso et al assessed the blood flow in the clitoris by using color Doppler ultrasonography in patients who underwent TVT or TOT surgery and reported that compared with TOT, the risk of deterioration of sexual function was higher after the TVT technique [23]. They explained that in TVT, the suburethral sling passes through the paraurethral space, leading to scar formation and reduced vaginal wall elasticity, resulting in a reduction in blood flow in the erectile tissues of the clitoris and thereby deteriorated sexual function. In contrast, the TOT procedure avoids the damage around the paraurethral space, which reduces the deterioration of sexual function [23].
In the present study, there was no significant difference between the two types of procedures in terms of changes in sexual function and satisfaction. We believe that both changes, improved sexual satisfaction due to the disappearance of incontinence and deteriorated sexual satisfaction due to scar formation and changed sensation at the anterior vaginal wall, influenced sexual function.
One of the limitations of this study is that the study was performed retrospectively and cross-sectionally. Because sexual function was not a primary aim of the care trial, characterization of sexual function was limited. As with any questionnaire that asks participants to recall their experience, responses of sexual activity may have been affected by recall bias. Also, sexual life is a sensitive personal problem, which may have lead to a low response rate. In the future, objective studies that select the proper subjects before and after surgery and evaluate the sexual function of individual patients are required.
Figures and Tables
 | Fig. 1Baseline replies to the questionnaire of the women who were sexually active both before and after surgery by age (p=0.57). |
 | Fig. 2Baseline replies to the questionnaire of the women who were sexually active both before and after surgery by procedures (TVT: tension-free vaginal tape, TOT: transobturator tape) (p=0.63). |
References
1. Yip SK, Chan A, Pang S, Leung P, Tang C, Shek D, et al. The impact of urodynamic stress incontinence and detrusor overactivity on marital relationship and sexual function. Am J Obstet Gynecol. 2003. 188:1244–1248.
2. Black NA, Bowling A, Griffiths JM, Pope C, Abel PD. Impact of surgery for stress incontinence on the social lives of women. Br J Obstet Gynaecol. 1998. 105:605–612.
3. Ulmsten U, Henriksson L, Johnson P, Varhos G. An ambulatory surgical procedure under local anesthesia for treatment of female urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct. 1996. 7:81–85.
4. Delorme E, Droupy S, de Tayrac R, Delmas V. Transobturator tape (Uratape): a new minimally-invasive procedure to treat female urinary incontinence. Eur Urol. 2004. 45:203–207.
5. de Leval J, Waltregny D. New surgical technique for treatment of stress urinary incontinence TVT-Obturator: new developments and results. Surg Technol Int. 2005. 14:212–221.
6. Mazouni C, Karsenty G, Bretelle F, Bladou F, Gamerre M, Serment G. Urinary complications and sexual function after the tension-free vaginal tape procedure. Acta Obstet Gynecol Scand. 2004. 83:955–961.
7. Yeni E, Unal D, Verit A, Kafali H, Ciftci H, Gulum M. The effect of tension-free vaginal tape (TVT) procedure on sexual function in women with stress urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct. 2003. 14:390–394.
8. Elzevier HW, Venema PL, Lycklama A, Nijeholt AA. Sexual function after tension-free vaginal tape (TVT) for stress incontinence: results of a mailed questionnaire. Int Urogynecol J Pelvic Floor Dysfunct. 2004. 15:313–318.
9. Ghezzi F, Serati M, Cromi A, Uccella S, Triacca P, Bolis P. Impact of tension-free vaginal tape on sexual function: results of a prospective study. Int Urogynecol J Pelvic Floor Dysfunct. 2006. 17:54–59.
10. Rogers RG, Kammerer-Doak D, Darrow A, Murray K, Qualls C, Olsen A, et al. Does sexual function change after surgery for stress urinary incontinence and/or pelvic organ prolapse? A multicenter prospective study. Am J Obstet Gynecol. 2006. 195:e1–e4.
11. Jha S, Moran P, Greenham H, Ford C. Sexual function following surgery for urodynamic stress incontinence. Int Urogynecol J Pelvic Floor Dysfunct. 2007. 18:845–850.
12. Maaita M, Bhaumik J, Davies AE. Sexual function after using tension-free vaginal tape for the surgical treatment of genuine stress incontinence. BJU Int. 2002. 90:540–543.
13. Glavind K, Tetsche MS. Sexual function in women before and after suburethral sling operation for stress urinary incontinence: a retrospective questionnaire study. Acta Obstet Gynecol Scand. 2004. 83:965–968.
14. Shah SM, Bukkapatnam R, Rodriguez LV. Impact of vaginal surgery for stress urinary incontinence on female sexual function: Is the use of polypropylene mesh detrimental? Urology. 2005. 65:270–274.
15. Marszalek M, Roehlich M, Racz U, Metzenbauer M, Ponholzer A, Rauchenwald M, et al. Sexual function after tension-free vaginal tape procedure. Urol Int. 2007. 78:126–129.
16. Murphy M, van Raalte H, Mercurio E, Haff R, Wiseman B, Lucente VR. Incontinence-related quality of life and sexual function following the tension-free vaginal tape versus the "inside-out" tension-free vaginal tape obturator. Int Urogynecol J Pelvic Floor Dysfunct. 2008. 19:481–487.
17. Sentilhes L, Berthier A, Caremel R, Loisel C, Marpeau L, Grise P. Sexual function after transobturator tape procedure for stress urinary incontinence. Urology. 2008. 71:1074–1079.
18. Lemack GE, Zimmern PE. Sexual function after vaginal surgery for stress incontinence: results of a mailed questionnaire. Urology. 2000. 56:223–227.
19. Sentilhes L, Berthier A, Sergent F, Verspyck E, Descamps P, Marpeau L. Sexual function in women before and after transvaginal mesh repair for pelvic organ prolapse. Int Urogynecol J Pelvic Floor Dysfunct. 2008. 19:763–772.
20. Tunuguntla HS, Gousse AE. Female sexual dysfunction following vaginal surgery: a review. J Urol. 2006. 175:439–446.
21. Barber MD, Visco AG, Wyman JF, Fantl JA, Bump RC. Sexual function in women with urinary incontinence and pelvic organ prolapse. Obstet Gynecol. 2002. 99:281–289.
22. Yucel S, De Souza A Jr, Baskin LS. Neuroanatomy of the human female lower urogenital tract. J Urol. 2004. 172:191–195.
23. Caruso S, Rugolo S, Bandiera S, Mirabella D, Cavallaro A, Cianci A. Clitoral blood flow changes after surgery for stress urinary incontinence: pilot study on TVT versus TOT procedures. Urology. 2007. 70:554–557.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download