Abstract
Purpose
We evaluated the safety and feasibility of transperitoneal laparoscopic upper pole heminephrectomy (TLUHN) in pediatric patients by comparing an age-matched cohort undergoing open upper pole heminephrectomy (OUHN) by a single surgeon.
Materials and Methods
A total of 10 OUHNs were performed between 1995 and 2003 and 10 TLUHNs between 2003 and 2008. The 10 patients in each group were matched by age (p=0.94), gender (p=1.0), and body weight (p=0.91).
Results
There was no open conversion in the TLUHN group. The median operative time in the TLUHN and OUHN groups was 174 minutes (range, 98-205) and 190 minutes (range, 120-258), respectively (p=0.19). In the TLUHN and OUHN groups, the median blood loss was 25 ml (range, 20-30) and 35 ml (range, 20-100) (p=0.74), the median analgesic requirement was 0 hours (range, 0-42) and 0 hours (range, 0-87) (p=0.16), and the median hospital stay was 5.5 days (range, 3-7) and 7 days (range, 3-19) (p=0.01), respectively. There were no intraoperative complications in either group. Postoperative atelectasis occurred in two and five patients in the TLUHN and OUHN groups, respectively. Similar results were found in the subanalysis of patients younger than 24 months.
Laparoscopic renal surgeries in pediatric patients have made remarkable progress in the past decade. Laparoscopic nephrectomy in pediatric patients is now considered to be a safe and feasible procedure with a decreased length of hospital stay [1]. Since the first experience of laparoscopic heminephrectomy was reported by Jordan and Winslow in 1993 [2], the operation has been reported as using either a transperitoneal or retroperitoneal approach [3]. However, the advantages of laparoscopic heminephrectomy over open surgery have not yet been verified. Moreover, some reports showed that laparoscopic heminephrectomy was not superior in terms of operative time or cost and was not safe in infants [4,5].
Thereafter, a few retrospective studies comparing the two operative methods found that laparoscopic heminephrectomy had an equivalent operative time, improved cosmesis, negligible blood loss, and shorter hospitalization [6,7]. Because laparoscopic heminephrectomy has not been found to be superior to open surgery in younger children and infants, some investigators have performed comparative analysis of age-matched groups of pediatric patients, including infants, undergoing laparoscopic or open heminephrectomy [8,9]. However, populations undergoing lower pole heminephrectomy or heminephroureterectomy for vesicoureteral reflux (VUR) were included in those studies, and operations were performed by various surgeons. A lower pole heminephrectomy is more technically demanding than an upper pole heminephrectomy [6], and heminephroureterectomy for VUR requires complex laparoscopic suturing technique. Therefore, we evaluated the safety and feasibility of transperitoneal laparoscopic upper pole heminephrectomy (TLUHN) in pediatric patients by comparing an age-matched cohort undergoing open upper pole heminephrectomy (OUHN) by a single surgeon in terms of operative and convalescence parameters.
A total of 10 OUHNs were performed between 1995 and 2003 and 10 TLUHNs between 2003 and 2008 at our institution. All operations were performed by a single surgeon (KSK). Because TLUHN requires advanced laparoscopic skills, the surgeon performed this operation after he surmounted the learning curve of other laparoscopic renal surgeries such as nephrectomy and nephroureterectomy [10].
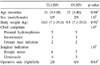
Patient and surgical demographics are presented in Table 1. The 10 patients in each group were matched by age (p=0.94), gender (p=1.0), and body weight (p=0.91). A subanalysis of patients younger than 24 months at surgery was also performed. Ectopic ureter and ureterocele were included in the surgical indications, and no concomitant procedure was performed at the same time.
OUHN was performed retroperitoneally via a subcostal flank approach with an incision below the 12th rib. The ureter draining the upper pole was identified and mobilized. It was transected and left open subsequently. The proximal ureter was used as a handle to manipulate and to resect the upper pole. Without dissecting the main renal vessels supplying the lower pole, the vessels branching to the upper pole were separated and ligated with silk tie. The parenchyma of the upper pole was dissected from the lower pole and cut using an electrocautery. Hemostasis of the renal edges was achieved also by electrocautery. A Penrose drain was inserted and then the incision was closed.
TLUHN was performed transperitoneally at around a 45℃ lateral position. A 10 mm camera port was inserted around the umbilicus by means of a Hasson trocar technique. Additionally, two or three working 5 mm ports were inserted under direct vision. Without dissecting the main renal vessels supplying the lower pole, the vessels branching to the upper pole were separated and ligated with Hem-o-lok. When there was a severe dilation in the upper pole ureter, the proximal ureter was cut and then used as a handle to identify and isolate the upper pole. Transection of the renal parenchyma was performed by using a harmonic scalpel. When the ureter was not dilated and the parenchyma was severely dysplastic, the boundary with the lower pole was marked by using an electrocautery, and then the upper pole was lifted upward and resected by using a harmonic scalpel. Hemostasis of the renal edges was achieved by an electrocautery or argon beam coagulator. A Jackson-Pratt drain was inserted through a 5 mm port site and the incisions were then closed.
Outcome data were retrospectively collected by chart review. Operative time was determined based on anesthesia and nursing records. The operative time indicated the time between skin incision and skin closure in the OUHN group, and between skin incision for the first trocar placement and skin closure for the trocar wounds in the TLUHN group. Blood loss described as 'minimal' was estimated as less than 20 ml [10]. Analgesic requirement was defined as the time between the operation and the last injection of intravenous analgesics. The administration of intravenous analgesics is decided pro re nata (PRN) by a request of parents or judgment of physicians. The median follow-up period was 10 months (range, 1-41) for the TLUHN group and 65.5 months (range, 8-155) for the OUHN group.
Continuous variables were analyzed by using the Mann-Whitney U test, and categorical variables were analyzed by using Fisher's exact test. Quantitative data were expressed as median (range). Statistical significance was set at p<0.05 for all analyses. All calculations were performed by using the Statistical Package for the Social Sciences, version 12.0 (SPSS Inc, Chicago, USA).
The surgical outcomes of all patients are represented in Table 2. No patient underwent open conversion in the TLUHN group. There were no significant differences in operative time, estimated blood loss, analgesic requirements, or time to returning to regular diet between the TLUHN and OUHN groups. The median hospital stay was 5.5 days (range, 3-7) for the TLUHN group and 7 days (range, 3-19) for the OUHN group (p=0.01). There were no intraoperative complications in either group. Postoperative fever (≥38℃) caused by atelectasis occurred in two and five patients in the TLUHN and OUHN groups, respectively. All atelectasis was recovered by physiotherapy without further complications.
The surgical outcomes for patients younger than 24 months at surgery are presented in Table 3. Patients in each group had identical age, sex, body weight, surgical indication, and operative side. These subgroups also had no significant differences in operative or convalescence parameters, except hospital stay (p=0.04).
The indications for a heminephrectomy in pediatric patients are to remove a nonfunctioning renal pole in a complicated duplex kidney and a renal pole with ectopic ureter causing urinary incontinence. Since the first reported laparoscopic heminephrectomy in pediatric patients in 1993 [2], the operation has been tested and determined to be as a standard operative method to substitute for open surgey [7]. The advantages of the laparoscopic approach include magnification of vision, shorter hospital stay, and less surgical scarring [6,11]. In addition to its general advantages over open surgery, laparoscopic heminephrectomy has other benefits. First, the risk of vasospasm or vascular injury, which causes a problem in the blood supply to the remnant pole, is low in laparoscopic surgery [3]. Because the magnified image of laparoscopy makes it easier to observe the renal pedicle, the laparoscopic approach requires minimal dissection and traction of the remnant pole, which results in less damage. Second, if complete ureterectomy is required, the entire procedure can be done under laparoscopy without additional incisions as demanded in open surgery [12].
Some reports had a negative view of laparoscopic heminephrectomy with regard to safety and feasibility in infants [4,5]. In a younger cohort of patients (mean age of 15.5 months), laparoscopic transperitoneal heminephrectomy revealed increased operative time and costs. On the other hand, Lee et al and Chertin et al reported that retroperitoneal and transperitoneal laparoscopic heminephrectomy in patients younger than 2 years had equivalent operative time and decreased postoperative narcotic requirements and hospitalization relative to open surgery, respectively [8,9]. However, two reports had heterogeneous study populations in terms of surgical indications or operators. A lower pole heminephrectomy is more technically demanding than an upper pole heminephrectomy, requiring more extensive dissection [6]. If the affected pole accompanies VUR, resection of the distal portion of the affected ureter and suture of the vesical hiatus are required. In the present study, we compared age- and weight-matched groups of patients with equivalent distributions by sex, surgical indication, and operative side in a consecutive upper pole heminephrectomy series by a single surgeon.
Although not significant, the median operative time for the TLUHN group was shorter than that for the OUHN group in the analysis of all patients and in the subanalysis of patients younger than 24 months. In two age-matched studies, laparoscopic heminephrectomy revealed similar operative time to open surgery regardless of the patient's age [8,9]. The reason for the shorter operative time in the TLUHN group may be that the surgeon overcame the learning curve of other laparoscopic renal surgeries, and our study population did not include complex cases such as lower pole heminephrectomy or nephroureterectomy [4,7]. Another explanation is that the two types of operation were not performed during the same period, and the OUHN group did not take the learning curve into consideration.
The TLUHN group tended to require less intravenous analgesics than the OUHN group, but this finding was obscured in the subanalysis of patients younger than 24 months. Although other studies have reported similar results, the methods defining analgesic requirements were different. Previous studies defined analgesic requirements by comparing analgesic use qualitatively and quantitatively [4] or by comparing the milligrams/kg of narcotics [7,8]. Because intravenous analgesics were administered pro re nata (PRN) by a request of parents or judgment of physicians in our study, our definition is qualitative rather than quantitative.
The TLUHN group was superior to the OUHN group regarding the length of hospital stay after surgery. Thus, our results confirmed those of earlier studies [6-9]. This finding indicates indirectly that children in the TLUHN group might be more comfortable after surgery. In our study, the TLUHN group showed a tendency for reduced intravenous analgesic requirements and occurrence of postoperative atelectasis. So we speculate that a low level of pain and decreased incidence of postoperative atelectasis may contribute to decreasing the length of hospital stay in LTUHN.
Our study has the advantage of an age-matched cohort in which the distributions of sex and body weight were equal, and to our knowledge it is the first study that compared two operative approaches of upper pole heminephrectomy that were performed consecutively by a single surgeon. However, there were several limitations in our study owing to its retrospective design. First, because two types of operation were performed during different periods, these results may be biased by various factors, such as surgeon's experience and changes in the discharging policy. Second, blood loss was described as 'minimal' in 12 patients. However, because postoperative hemoglobin was not routinely checked, it was not possible to get objective data. Therefore, the estimated blood loss was biased by the surgeon's intuition. Third, the level of pain is difficult to quantify because of a lack of a validated pain scoring system, nonstandardized pain management, and a variety of analgesics administered.
We favor the transperitoneal approach for several reasons. First, the transperitoneal approach provides a wider working space and makes it easy to manipulate the laparoscopic instruments in small children [13]. Second, the transperitoneal approach allows the removal of the entire ureter during surgery [7]. The need to remove a distal ureter was reported in patients with ectopic ureters from open or laparoscopic series [14,15]. In the OUHN group, two patients required interventions for an infected distal ureteral stump (ultrasono-guided aspiration at postoperative 9 months and laparoscopic distal ureterectomy at postoperative 85 months). In the TLUHN group, one patient revealed a silent distal ureteral stump at 31 months postoperatively. The median follow-up period was significantly shorter in the TLUHN group, so long-term follow-up would be mandatory to study these anatomic results appropriately. Third, higher open conversion and complication rates are reported in the retroperitoneal approach [16]. We experienced one retroperitoneal heminephrectomy during the same study period, and the case revealed complete functional loss of the remnant pole.
Figures and Tables
References
1. Kim HH. Laparoscopic surgery in urology (II). Korean J Urol. 2003. 44:1071–1081.
2. Jordan GH, Winslow BH. Laparoscopic upper pole partial nephrectomy with ureterectomy. J Urol. 1993. 150:940–943.
3. Peters CA. Laparoscopy in pediatric urology. Curr Opin Urol. 2004. 14:67–73.
4. Robinson BC, Snow BW, Cartwright PC, De Vries CR, Hamilton BD, Anderson JB. Comparison of laparoscopic versus open partial nephrectomy in a pediatric series. J Urol. 2003. 169:638–640.
5. Wallis MC, Khoury AE, Lorenzo AJ, Pippi-Salle JL, Bägli DJ, Farhat WA. Outcome analysis of retroperitoneal laparoscopic heminephrectomy in children. J Urol. 2006. 175:2277–2280.
6. El-Ghoneimi A, Farhat W, Bolduc S, Bagli D, McLorie G, Khoury A. Retroperitoneal laparoscopic vs open partial nephroureterectomy in children. BJU Int. 2003. 91:532–535.
7. Piaggio L, Franc-Guimond J, Figueroa TE, Barthold JS, González R. Comparison of laparoscopic and open partial nephrectomy for duplication anomalies in children. J Urol. 2006. 175:2269–2273.
8. Lee RS, Retik AB, Borer JG, Diamond DA, Peters CA. Pediatric retroperitoneal laparoscopic partial nephrectomy: comparison with an age matched cohort of open surgery. J Urol. 2005. 174:708–711.
9. Chertin B, Ben-Chaim J, Landau EH, Koulikov D, Nadu A, Reissman P, et al. Pediatric transperitoneal laparoscopic partial nephrectomy: comparison with an age-matched group undergoing open surgery. Pediatr Surg Int. 2007. 23:1233–1236.
10. You D, Bang JK, Kim KS. Analysis of the learning curve for laparoscopic renal surgeries in children. Korean J Urol. 2009. 50:380–386.
11. Horowitz M, Shah SM, Ferzli G, Syad PI, Glassberg KI. Laparoscopic partial upper pole nephrectomy in infants and children. BJU Int. 2001. 87:514–516.
12. Janetschek G, Seibold J, Radmayr C, Bartsch G. Laparoscopic heminephroureterectomy in pediatric patients. J Urol. 1997. 158:1928–1930.
13. You D, Kim KS. Selection of approach method during laparoscopic renal surgeries in pediatric patients. Korean J Urol. 2007. 48:276–282.
14. Plaire JC, Pope JC 4th, Kropp BP, Adams MC, Keating MA, Rink RC, et al. Management of ectopic ureters: experience with the upper tract approach. J Urol. 1997. 158:1245–1247.
15. Dénes FT, Danilovic A, Srougi M. Outcome of laparoscopic upper-pole nephrectomy in children with duplex systems. J Endourol. 2007. 21:162–168.
16. Valla JS, Breaud J, Carfagna L, Tursini S, Steyaert H. Treatment of ureterocele on duplex ureter: upper pole nephrectomy by retroperitoneoscopy in children based on a series of 24 cases. Eur Urol. 2003. 43:426–429.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download