Abstract
Purpose
To evaluate the efficacy and safety of artificial urinary sphincter (AUS) for the treatment of stress urinary incontinence (UI) after prostate surgery.
Materials and Methods
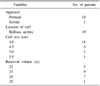
We performed a retrospective chart review of 19 patients who underwent AUS implantation from July 2003 to November 2008. Efficacy was evaluated in terms of the postoperative changes in daily pad use, incontinence visual analogue scale (I-VAS), International Continence Society male-Short Form questionnaire (ICS-male SF), Incontinence Quality of Life questionnaire (I-QoL), and patients' satisfaction postoperatively. No pad use was defined as cure, and use of 1 pad or fewer per day as improvement. Cure and improvement were regarded as success. Complications and durability of the AUS were evaluated.
Results
The median age of the patients was 70.0 years (range, 47-76 years). With a median follow-up period of 11.8 months (range, 6.2-48.1 months), the success rate was 68.4% (13/19; cure in 12 and improvement in 1). I-VAS, subscale scores of ICS-male SF (incontinence and QoL), and total and subscale scores of I-QoL (psychosocial impact, social embarrassment, avoidance, and limiting behaviors) were significantly improved. Fifteen (78.9%) patients reported being satisfied. Six (31.5%) patients required revision: volume adjustment for 2, second cuff implantation for 2, pump reposition for 1, and pump reposition, volume adjustment, and second cuff implantation for 1. One of the patients who had a second cuff implantation had the sphincter explanted for infection.
Figures and Tables
References
1. Gaker DL, Gaker LB, Stewart JF, Gillenwater JY. Radical prostatectomy with preservation of urinary continence. J Urol. 1996. 156:445–449.
2. Arai Y, Okudo K, Aoki Y, Maekawa S, Okada T, Maeda H, et al. Patient-reported quality of life after radical prostatectomy for prostate cancer. Int J Urol. 1999. 6:78–86.
3. Gundian JC, Barrett DM, Parulkar BG. Mayo Clinic experience with the AS800 artificial urinary sphincter for urinary incontinence after transurethral resection of prostate or open prostatectomy. Urology. 1993. 41:318–321.
4. Penson DF, McLerran D, Feng Z, Li L, Albertsen PC, Gilliland FD, et al. 5-year urinary and sexual outcomes after radical prostatectomy: results from the prostate cancer outcomes study. J Urol. 2005. 173:1701–1705.
5. Begg CB, Riedel ER, Bach PB, Kattan MW, Schrag D, Warren JL, et al. Variations in morbidity after radical prostatectomy. N Engl J Med. 2002. 346:1138–1144.
6. Steineck G, Helgesen F, Adolfsson J, Dickman PW, Johansson JE, Norlen BJ, et al. Quality of life after radical prostatectomy or watchful waiting. N Engl J Med. 2002. 347:790–796.
7. Cespedes RD, Leng WW, McGuire EJ. Collagen injection therapy for postprostatectomy incontinence. J Urol. 1999. 54:597–602.
8. Castle EP, Andrews PE, Itano N, Novicki DE, Swanson SK, Ferrigni RG. The male sling for post-prostatectomy incontinence: mean followup of 18 months. J Urol. 2005. 173:1657–1660.
9. Litwiller SE, Kim KB, Fone PD, White RW, Stone AR. Post-prostatectomy incontinence and the artificial urinary sphincter: a long-term study of patient satisfaction and criteria for success. J Urol. 1996. 156:1975–1980.
10. Scott FB, Bradley WE, Timm GW. Treatment of urinary incontinence by implantable prosthetic sphincter. Urology. 1973. 1:252–259.
11. Montague DK, Angermeier KW, Paolone DR. Long-term continence and patient satisfaction after artificial sphincter implantation for urinary incontinence after prostatectomy. J Urol. 2001. 166:547–549.
12. Moon YT, Lee KB, Moon WC, Soh BU, Kim SC. A case of urinary incontinence treatment using AMS 800-artificial sphincter. Korean J Urol. 1986. 27:337–344.
13. Perez LM, Webster GD. Successful outcome of artificial urinary sphincters in men with post-prostatectomy urinary incontinence despite adverse implantation features. J Urol. 1992. 148:1166–1170.
14. Gomha MA, Boone TB. Artificial urinary sphincter for post-prostatectomy incontinence in men who had prior radiotherapy: a risk and outcome analysis. J Urol. 2002. 167:591–596.
15. Gousse AE, Madjar S, Lambert MM, Fishman IJ. Artificial urinary sphincter for post-radical prostatectomy urinary incontinence: long-term subjective results. J Urol. 2001. 166:1755–1758.
16. Martins FE, Boyd SD. Post-operative risk factors associated with artificial urinary sphincter infection-erosion. Br J Urol. 1995. 75:354–358.
17. Light MR, Montague DK, Angermeier KW, Lakin MM. Cultures from genitourinary prostheses at reoperation: questioning the role of Staphylococcus epidermidis in periprosthetic infection. J Urol. 1995. 154:387–390.
18. Martins FE, Boyd SD. Artificial urinary sphincter in patients following major pelvic surgery and/or radiotherapy: Are they less favorable candidates? J Urol. 1995. 153:1188–1193.
19. Elliott DS, Barrett DM. Mayo Clinic long-term analysis of the functional durability of the AMS 800 artificial urinary sphincter: a review of 323 cases. J Urol. 1998. 159:1206–1208.
20. Clemens JQ, Schuster TG, Konnak JW, McGuire EJ, Faerber GJ. Revision rate after artificial urinary sphincter implantation for incontinence after radical prostatectomy: actuarial analysis. J Urol. 2001. 166:1372–1375.
21. Kim SP, Sarmast Z, Daignault S, Faerber GJ, McGuire EJ, Latini JM. Long-term durability and functional outcomes among patients with artificial urinary sphincters: a 10-year retrospective review from the University of Michigan. J Urol. 2008. 179:1912–1916.
22. Raj GV, Peterson AC, Toh KL, Webster GD. Outcomes following revisions and secondary implantation of the artificial urinary sphincter. J Urol. 2005. 173:1242–1245.
23. Webster GD, Sherman ND. Management of male incontinence following artificial urinary sphincter failure. Curr Opin Urol. 2005. 15:386–390.
24. Wilson SK, Delk JR 2nd, Henry GD, Siegel AL. New surgical technique for sphincter urinary control system using upper transverse scrotal incision. J Urol. 2003. 169:261–264.
25. Henry GD, Graham SM, Cleves MA, Simmons CJ, Flynn B. Perineal approach for artificial urinary sphincter implantation appears to control male stress incontinence better than the transscrotal approach. J Urol. 2008. 179:1475–1479.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download