Abstract
Purpose
With recent technological advances, the indications for retrograde intrarenal surgery (RIRS) have gradually increased. We evaluated the efficacy and treatment outcomes of RIRS for the treatment of renal stones.
Materials and Methods
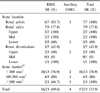
We retrospectively reviewed the medical records of 23 patients with renal stones (7 in the renal pelvis, 9 in the renal calyx, and 7 in the renal diverticulum) treated with RIRS from January 2001 to July 2008. Mean stone burden was 110 mm2 (range, 9.42-428.6 mm2), and all operations were performed under general anesthesia using a semi-rigid ureteroscope in 9 cases, a flexible ureteroscope in 11 cases, and both types simultaneously in 3 cases. The holmium:yttrium-aluminum-garnet (Ho: YAG) laser and the nitinol basket were used for stone fragmentation and retrieval. The patients were followed up postoperatively with KUB (21 cases) or nonenhanced computed tomography (CT; 2 cases). Success was defined as no visible stones on KUB or nonenhanced CT.
Results
The mean operating time was 93 minutes (range, 30-205 minutes) and the mean hospital stay was 3.7 days (range, 1-9 days). Of 23 patients, 16 (70%) experienced complete elimination of the stone after only a single intervention. After ancillary extracorporeal shock wave lithotripsy (ESWL), the success rate was increased to 74% (17/23). In the remaining 6 patients, residual stone findings were less than 3 mm and were followed up with X-ray.
Conclusions
RIRS is a feasible procedure for treating renal stone disease with minimal complications. The results of our study suggest that RIRS can be recommended as a primary modality in the management of renal stone disease in selected patients such as those with ESWL failure and renal diverticular stones.
Figures and Tables
References
1. Segura JW, Preminger GM, Assimos DG, Dretler SP, Kahn RI, Lingeman JE, et al. The American Urological Association. Ureteral Stones Clinical Guidelines Panel summary report on the management of ureteral calculi. J Urol. 1997. 158:1915–1921.
2. Lam JS, Greene TD, Gupta M. Treatment of proximal ureteral calculi: holmium:YAG laser ureterolithotripsy versus extracorporeal shock wave lithotripsy. J Urol. 2002. 167:1972–1976.
3. Parker BD, Frederick RW, Reilly TP, Lowry PS, Bird ET. Efficiency and cost of treating proximal ureteral stones: shock wave lithotripsy versus ureteroscopy plus holmium:yttrium-aluminum-garnet laser. Urology. 2004. 64:1102–1106.
4. Chen RN, Streem SB. Extracorporeal shock wave lithotripsy for lower pole calculi: long-term radiographic and clinical outcome. J Urol. 1996. 156:1572–1575.
5. Sampaio FJ, Aragao AH. Limitations of extracorporeal shockwave lithotripsy for lower caliceal stones: anatomic insight. J Endourol. 1994. 8:241–247.
6. Vandeursen H, Baert L. Extracorporeal shock wave lithotripsy monotherapy for staghorn stones with the second generation lithotriptors. J Urol. 1990. 143:252–256.
7. Park J, Hong B, Park T, Park H. The effectiveness of noncontrast computerized tomography (CT) in evaluation of residual stones after percutaneous nephrolithotomy. Korean J Urol. 2006. 27:1315–1319.
8. You D, Park T, Park HK. Endourologic management for calyceal diverticular stone. Korean J Urol. 2005. 46:144–148.
9. Khaitan A, Gupta NP, Hemal AK, Dogra PN, Seth A, Aron M. Post-ESWL, clinically insignificant residual stones: reality or myth? Urology. 2002. 59:20–24.
10. Fabrizio MD, Behari A, Bagley DH. Ureteroscopic management of intrarenal calculi. J Urol. 1998. 159:1139–1143.
11. Perlmutter AE, Talug C, Tarry WF, Zaslau S, Mohseni H, Kandzari SJ. Impact of stone location on success rates of endoscopic lithotripsy for nephrolithiasis. Urology. 2008. 71:214–217.
12. Oh BS, Hwang EC, Chae MJ, Oh KJ, Kang TW, Kwon DD, et al. Efficacy of the 3rd generation extracorporeal shock wave lithotriptor (Piezolith 3000®) for treating patients with urinary tract calculi. Korean J Urol. 2005. 46:1278–1283.
13. Grasso M, Ficazzola M. Retrograde ureteropyeloscopy for lower pole caliceal calculi. J Urol. 1999. 162:1904–1908.
14. Mitchell S, Havranek E, Patel A. First digital flexible ureterorenoscope: initial experience. J Endourol. 2008. 22:47–50.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download