Abstract
Purpose
Primary treatment of children with vesicoureteral reflux (VUR) is antibiotic prophylaxis until the reflux resolves. But, it is not easy to determine in which patients the reflux resolves. We sought to determine whether renal scarring could help to predict the prognosis of reflux regarding reflux resolution and breakthrough infection.
Materials and Methods
A total of 90 children, 54 boys and 36 girls, mean age 15.1 (range: 1-98) months, with VUR were analyzed retrospectively. Eighty-six presented with febrile urinary tract infection (UTI) and 4 with prenatal hydronephrosis. Technetium Tc 99m dimercaptosuccinic acid (DMSA) scans were performed at 4 months after resolution of a febrile UTI. All children were initially treated with antibiotic prophylaxis (Bactrim®; TMX-SMX 2 mg/kg/day) and 40 underwent antireflux surgery. Median follow-up was 26.1 (range: 6-52) months. Reflux grade was defined by use of the International Classification System. We analyzed the incidence of renal scarring according to reflux grade, reflux resolution, and reason for antireflux surgery.
Results
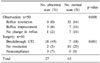
Normal DMSA scans were documented in 63 (70%) children and renal scarring in 27 (30%). Children with renal scarring presented high grade (III-V) VUR. VUR with renal scarring was not resolved spontaneously and increased the risk for breakthrough UTI. Renal scarring could help to predict the prognosis of reflux regarding reflux resolution and breakthrough infection. VUR grade, however, did not help to predict the prognosis of reflux.
Figures and Tables
References
1. Lenaghan D, Whitaker JG, Jensen F, Stephens FD. The natural history of reflux and long-term effects of reflux on the kidney. J Urol. 1976. 115:728–730.
2. Skoog SJ, Belman AB, Majd M. A nonsurgical approach to the management of primary vesicoureteral reflux. J Urol. 1987. 138:941–946.
3. Scholtmeijer RJ. Treatment of vesicoureteric reflux. Results of a prospective study. Br J Urol. 1993. 71:346–349.
4. Smellie JM, Poulton A, Prescod NP. Retrospective study of children with renal scarring associated with reflux and urinary infection. BMJ. 1994. 308:1193–1196.
5. Weiss R, Duckett J, Spitzer A. Results of a randomized clinical trial of medical versus surgical management of infants and children with grades III and IV primary vesicoureteral reflux (United States). The International Reflux Study in Children. J Urol. 1992. 148:1667–1673.
6. Preda I, Jodal U, Sixt R, Stokland E, Hansson S. Normal dimercaptosuccinic acid scintigraphy makes voiding cystourethrography unnecessary after urinary tract infection. J Pediatr. 2007. 151:581–584.
7. Garin EH, Olavarria F, Garcia Neito V, Valenciano B, Compos A, Young L. Clinical significance of primary vesicoureteral reflux and urinary antibiotic prophylaxis after acute pyelonephritis: a multicenter, randomized, controlled study. Pediatrics. 2006. 117:626–632.
8. Mingin GC, Nguyen HT, Baski LS, Harlen S. Abnormal dimercapto-succinic scans predict an increased risk of breakthrough infection in children with vesicoureteral reflux. J Urol. 2004. 172:1075–1077.
9. Woodward A. Vesico ureteric reflux and urinary tract infections in children. Aust Fam Physician. 1998. 27:1095–1097.
10. Yang SK, Choi SK. Validity of 99m Tc-dimercaptosuccinic acid scan for detection of renal scarring. Korean J Urol. 1991. 32:61–68.
11. Kim KS, Chung KH, Kim KM, Kim IW, Yeon KM, Choi H. The urologic abnormalities of urinary tract infection in children and their detection. Korean J Urol. 1989. 30:350–354.
12. Yeom MH, Chung SK, Lee KS, Kim KS, Park JS, Ryu DS, et al. Incidence of vesicoureteral reflux for prepuberty patients in Daegu city and Gyeongbuk area according to the clinical indications, gender and age. Korean J Urol. 2005. 46:1284–1289.
13. Elder JS. Guidelines for consideration for surgical repair of vesicoureteral reflux. Curr Opin Urol. 2000. 10:579–585.
14. Smellie JM, Ransley PG, Normand IC, Prescod N, Edwards D. Development of new renal scars: a collaborative study. Br Med J. 1985. 290:1957–1960.
15. Bellinger MF, Duckett JW. Vesicoureteral reflux: a comparison of non-surgical and surgical management. Contrib Nephrol. 1984. 39:81–93.
16. Noe HN. The long-term results of prospective sibling reflux screening. J Urol. 1992. 148:1739–1742.
17. Walker RD. Renal functional changes associated with vesicoureteral reflux. Urol Clin North Am. 1990. 17:307–316.
18. Knudson MJ, Austin JC, McMillan ZM, Hawtrey CE, Cooper CS. Predictive factors of early spontaneous resolution in children with primary vesicoureteral reflux. J Urol. 2007. 178:1684–1688.
19. Papachristou F, Printza N, Kavaki D, Koliakos G. The characteristics and outcome of primary vesicoureteric reflux diagnosed in the first year of life. Int J Clin Pract. 2006. 60:829–834.
20. Park SY, Park HY, Woo YN. The factors affecting the outcome after medical management of vesicoureteral reflux. Korean J Urol. 2006. 47:994–1000.
21. Sweeney B, Cascio S, Velayudham M, Puri P. Reflux nephropathy in infancy: a comparison of infants presenting with and without urinary tract infection. J Urol. 2001. 166:648–650.
22. Merguerian PA, Jamal MA, Agarwal SK, McLorie GA, Bagli DJ, Shuckett B, et al. Utility of SPECT DMSA renal scanning in the evaluation of children with primary vesicoureteral reflux. Urology. 1999. 53:1024–1028.
23. Stokland E, Hellstrom M, Jacobsson B, Jodal U, Sixt R. Renal damage one year after first urinary tract infection: role of dimercaptosuccinic acid scintigraphy. J Pediatr. 1996. 129:815–820.
24. Scherz HC, Downs TM, Caesar R. The selective use of dimercaptosuccinic acid renal scans in children with vesicoureteral reflux. J Urol. 1994. 152:628–631.
25. Rushton HG, Majd M, Jantausch B, Wiedermann BL, Belman AB. Renal scarring following reflux and nonreflux pyelonephritis in children: evaluation with 99mtechnetium-dimercaptosuccinic acid scintigraphy. J Urol. 1992. 147:1327–1332.
26. Ash JM, McLorie GA. Can DMSA detect early renal injury in children with vesicoureteral reflux. J Nucl Med. 1994. 35:449–450.
27. Goldman M, Bistritzer T, Horne T, Zoareft I, Aladjem M. The etiology of renal scars in infants with pyelonephritis and vesicoureteral reflux. Pediatr Nephrol. 2000. 14:385–388.
28. Levit SB, Duckett J, Spitzer A, Walker D, Weiss R, Lebowitz R, et al. Medical versus surgical treatment of primary vesicoureteral reflux: a prospective international reflux study in children. J Urol. 1981. 67:392–400.
29. Choi H, Oh SJ, So Y, Lee DS, Lee A, Kim KM. No further development of renal scarring after antireflux surgery in children with primary vesicoureteral reflux: review of the results of 99mtechnetium dimercapto-succinic acid renal scan. J Urol. 1999. 162:1189–1192.
30. Elder JS, Peters CA, Arant BS Jr, Ewalt DH, Hawtrey CE, Hurwitz RS, et al. Pediatric vesicoureteral reflux guidelines panel summary report on the management of primary vesicoureteral reflux in children. J Urol. 1997. 157:1846–1851.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download