Intravesical Bacille Calmette-Guerin (BCG) instillation therapy for superficial transitional cell carcinoma of the bladder is commonly used and is generally safe. However, this therapy may rarely be complicated by tuberculous granulomatous infection of the urinary tract. We report a case of a prostatic abscess related to intravesical BCG therapy for carcinoma in situ with a brief review of the literature.
CASE REPORT
A 63-year-old man was evaluated for a week's dysuria and microscopic hematuria. There were no notable findings in his medical and family history. His physical examination was normal. Excretory urography was normal and subsequent cystoscopy revealed a papillary bladder tumor on the left lateral wall and a velvet-like erythematous lesion around the ipsilateral ureteral orifice. Preoperative chest PA and an abdominal computed tomography (CT) scan showed nonspecific findings. The papillary mass was removed by transurethral resection, and the erythematous lesion was biopsied. Histologically, the papillary mass was a grade 3 transitional cell carcinoma without invasion of lamina propria (pTa), and carcinoma in situ was detected on the erythematous lesion. Intravesical BCG instillations (OncoTICE®, Organon, Netherlands) were started 2 weeks after the operation and were administered once per week for 6 weeks. There were no difficulty with instillation and evidence of BCG toxicity except mild urethral discomfort. No relapse was found in follow-up cystoscopy conducted 3 months after the operation.
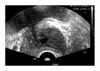
Two months after the last cystoscopy, the patient visited the hospital again owing to hesitancy and weak stream. On digital rectal examination, the prostate was symmetrically mildly enlarged and there was no palpable nodule. The prostate-specific antigen (PSA) level was raised at 6.19 ng/ml. Transrectal ultrasonography showed a relatively well-defined focal anechoic lesion in the right transitional zone, arousing suspicion of a prostatic abscess (Fig. 1), and the volume of the prostate was 36 cc. For diagnosis and improvement of the symptoms, a transurethral resection of the prostate was performed, and subsequent histology showed granulomatous prostatitis with acid-fast bacilli (Fig. 2). The patient received 300 mg of isoniazid, 600 mg of rifampicin, and 1,000 mg of pyrazinamide for 2 months, and in the following 4 months, 600 mg of isoniazid and 900 mg of rifampicin 3 times per week. No signs of bladder cancer recurrence or aggravation of urination symptoms were found in follow-up observations for 25 months.
DISCUSSION
Intravesical BCG instillation therapy was first used in 1976 as a nonspecific immune stimulant.1 It is currently in wide use as an effective treatment option for the removal and suppression of recurrence of superficial transitional cell carcinoma and carcinoma in situ.2
Granulomatous prostatitis after BCG therapy is not a rare complication, being reported by Lamm et al3 to have occurred in 0.9% of 1,278 cases. However, the reported cases of granulomatous prostatitis were not confirmed to be associated with BCG infection. In Korea, Kim et al4 also reported a case of granulomatous prostatitis after BCG therapy, but they could not find any evidence of tuberculous infection. Thus, there are few reports of localized BCG infection of the genitourinary tract related to BCG therapy.
Two cases of tuberculous prostatic abscess that developed after BCG therapy were found through a review of the literature. The first reported case was a transitional cell carcinoma of the bladder accompanied by carcinoma in situ. Forty-four months after diagnosis of carcinoma in situ, perineal pain developed and the patient was on BCG maintenance therapy. The diagnosis of prostatic abscess was confirmed by CT, and the patient was treated by transperineal drainage.5 The second case was a recurrent carcinoma in situ. Symptoms appeared 5 weeks after BCG therapy, and digital rectal examination aroused suspicion of a prostatic abscess. Without further radiologic workup, the patient was treated by transurethral prostatic resection.6 Anti-tuberculosis drugs were administered after the operation in both cases, for 12 and 9 months, respectively.
Considering the increased usage of BCG therapy for superficial transitional cell carcinoma, it is important to recognize the possibility of this tuberculous prostatic infection in cases with localized or voiding symptoms.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download