Abstract
Extramammary Paget's disease (EMPD) is a rare intraepithelial adenocarcinoma. To date, about 200 cases of EMPD have been reported since the first report in 1889. There has been only one case of EMPD involving the umbilicus, in a patient with prostatic carcinoma. This is the first report of EMPD occurring concurrently in the scrotum and umbilicus. The patient had recurrent, eczematous, and pruritic lesions of the left scrotum and umbilicus 2 years previously. Biopsy and surgical resection were performed and EMPD was diagnosed. There was no evidence of recurrence at 34 months after surgery.
Extramammary Paget's disease (EMPD) is a rare intraepithelial adenocarcinoma that usually arises in areas of the skin bearing apocrine and exocrine glands, including the vulva, perianal, penoscrotal, and axillary areas. EMPD may also occur in other areas, including the eyelids, umbilicus, ear canals, and thigh [1]. To date, about 200 cases of EMPD have been reported since the first report in 1889 [2]. In contrast, there has been only one case of EMPD involving the umbilicus, in a patient with prostatic carcinoma. It is difficult to distinguish EMPD from malignant melanoma, Bowen's disease, squamous cell carcinoma in situ, leukoplakia, superficial fungal infection, psoriasis, or eczematous dermatitis. We describe here a patient with EMPD involving both the scrotum and the umbilicus that had been misdiagnosed as eczematous dermatitis for two years. The EMPD was removed by surgical excision.
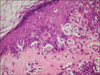
A 56-year-old Korean male had presented with a 2×3 cm sized, recurrent, eczematous, and pruritic lesion of the left scrotum 2 years previously. At first, the lesion was diagnosed as eczema and was treated accordingly. However, the patient's symptoms did not improve and the size of the lesion increased. After biopsy, the scrotal lesion was defined as EMPD. There was nothing notable in the patient's past medical history or family history, and the patient was in generally good health. Physical examination revealed a 2×3 cm sized, painless, and dark-reddish-brown lesion in the left upper scrotum and a 1×1 cm sized lesion in the umbilicus, both of which had exfoliations with fairly distinctive borders (Fig. 1). The inguinal lymph node was not enlarged. The results of a complete blood count (CBC), electrolyte battery, and liver function, renal function, and urine tests were within normal limits, as were the results of tests for serum tumor markers (CEA, CA 19-9, a-FP, and prostate-specific antigen [PSA]), which thus failed to show the presence of any underlying tumor. There were no specific findings on a chest x-ray or on computerized tomography of the abdomen-pelvis, except for a simple, 1 cm sized cyst on the left kidney. There were no specific findings on esophagogastroduodenoscopy or colonoscopy, except for chronic colitis. These findings indicated that the patient had EMPD of the scrotum and umbilicus, and a wide local excision was performed to remove visible lesions and surrounding areas (with safety resection margins of 2 cm for the scrotum and 3 cm for the umbilicus), followed by primary repair. Intraoperative cystoscopy showed a bullous edema at the bulbous urethra, but biopsy of this lesion showed no tumor cells. Intraoperative frozen biopsy of the surgical margins of the scrotal (four sites) and umbilical (nine sites) lesions also confirmed the absence of tumor cells. Microscopic examination of the resected scrotal and umbilical lesions revealed clusters, in both, of Paget's cells scattered throughout the epithelium. These cells had pale cytoplasm and larger nuclei than the surrounding normal epithelial cells and were apparently growing upward from the basement membrane. The basement membrane was intact and there was no invasion of tumor cells into the dermis (Fig. 2, 3). Immunohistochemically, these cells were positive for periodic acid-Schiff (PAS) and Alcian blue staining, but negative for S-100, indicative of EMPD. At the present time, 34 months after surgery, there have been no signs of recurrence or metastasis and no further symptoms of EMPD (Fig. 4).
EMPD rarely occurs in the anogenital region. Clinically, EMPD appears as an erythema, eczema, ulceration, hemorrhage, papillar cluster, or crust, accompanied by pain or pruritus, with a border that clearly distinguishes EMPD from the surrounding tissues. If EMPD lesions are complicated by bacterial or fungal infection, however, the clinical signs are indistinct. As such, gross findings are common and the symptoms are not specific. Thus, diagnosis may take 1 month to 17 years, and EMPD lesions are sometimes overlooked. Any unusual, chronic cutaneous lesion with clinical progression that is unresponsive to conservative treatment should therefore be biopsied. EMPD occurs mostly in areas of the epithelium rich in apocrine glands, but may also occur in keratinocytes, melanocytes, pluripotent germinative epidermal cells, and exocrine glands. EMPD is usually localized to the labia major, eyelids, umbilicus, thighs, and perianal, penoscrotal, and axillary areas [1]. Before this report, there was only one report of umbilical EMPD, which was successfully treated by surgical excision, in a patient with underlying prostatic carcinoma [3]. Thus, to the best of our knowledge, this is the first report of EMPD occurring concurrently in the scrotum and umbilicus.
The average age at diagnosis of patients with EMPD is 64 years (range, 51-79 years). Most patients are diagnosed by biopsy at departments of dermatology and are then transferred for surgical treatment. Lesion size has been found to vary, from less than 3 cm2 to 15×10 cm2 (average, 25.2 cm2) [4]. About 20% of patients with EMPD show partial invasion of the dermal layer, and about 12% have internal malignancies at the time of diagnosis, making screening for any accompanying internal malignancies essential. In the present case, serum tumor markers, including CEA, CA 19-9, a-FP, and PSA, were measured, and chest x-ray, esophagogastroduodenoscopy, colonoscopy, and cystoscopy were performed, all of which confirmed the absence of internal malignancy.
Histologically, EMPD must show pathognomonic intraepidermal Paget's cells. These cells are larger in size than surrounding keratinocytes, and their cytoplasm is clear and rich, with larger, irregularly shaped nuclei and polymorphic nucleoli [5]. Immunohistochemically, Paget's cells show positive responses to PAS, mucicarmine, Alcian blue, aldehyde-fuchsin, and toluidine blue because of the presence of sialomucin in the cytoplasm [6]. It is difficult to distinguish EMPD from malignant melanoma, Bowen's disease, squamous cell carcinoma in situ, leukoplakia, superficial fungal infection, psoriasis, or eczematous dermatitis [7].
Treatment is dependent on the aggressiveness of the lesion. Lesions may be removed surgically or by noninvasive methods including cryotherapy, laser excision, intralesional interferon, topical treatment with ointment, photodynamic therapy, antiandrogens, radiation therapy, or systemic chemotherapy. The basic principle of surgical treatment is the wide and complete excision of the epithelial and subcutaneous layers that have been invaded by tumor cells. Even if the gross findings are normal, there may be some microscopic invasion of Paget's cells, indicating that the surgical margin from the gross lesion should be 1 to 5 cm. Incomplete excision has been reported to occur in 36% of patients in whom an intraoperative frozen biopsy of the surgical margin was not performed, with a recurrence rate of 38%. This was higher than the recurrence rate of 25% when intraoperative frozen biopsy was performed [8]. If lymph node metastasis is clinically suspected, the ilioinguinal region and pelvic lymph nodes should be dissected. For patients with no suspected clinical findings, however, prophylactic lymph node dissection is not recommended [9]. Factors affecting patient prognosis include the depth of dermal invasion, surgical margin status, underlying carcinoma, lymph node status, and staging [8].
Our patient had a good prognosis, and there have been no signs of recurrence or metastasis up to 34 months postoperatively. However, the EMPD recurrence rate is 32% to 61% with distant metastases to internal organs requiring about 16 to 20 months [10]. In contrast, EMPD in the umbilicus is extremely rare, and clinical progression and prognosis in such a case is unknown. Moreover, in our patient, EMPD of the umbilicus accompanied the scrotal lesion. Periodic and close follow-up are therefore necessary to assess recurrence and distant metastases to other organs.
Figures and Tables
Fig. 1
Preoperative photograph showing extramammary Paget's disease manifesting as scaly, dark red-brown plaques with well-defined borders on the umbilicus (about 1×1 cm sized).

Fig. 2
Photomicrography showing proliferation of abundant pale Paget's cells with scattered atypical nuclei in the epidermis (H&E, reduced from ×100).
References
1. Chanda JJ. Extramammary Paget's disease: prognosis and relationship to internal malignancy. J Am Acad Dermatol. 1985. 13:1009–1014.
2. Crocker HR. Paget's disease affecting the scrotum and penis. Trans Pathol Soc Lond. 1889. 10:187–191.
3. Remond B, Aractingi S, Blanc F, Verola O, Vignon D, Dubertret L. Umbilical Paget's disease and prostatic carcinoma. Br J Dermatol. 1993. 128:448–450.
4. Yang WJ, Kim DS, Im YJ, Cho KS, Rha KH, Cho NH, et al. Extramammary Paget's disease of penis and scrotum: diagnosis, treatment and prognosis. Korean J Urol. 2005. 46:159–162.
5. Gumurdula D, Sung CJ, Lawrence WD. Pathologic quiz case: a 63-year-old woman with a pigmented perineal lesion. Extramammary Paget disease. Arch Pathol Lab Med. 2004. 128:e23–e24.
6. Kanitakis J. Mammary and extramammary Paget's disease. J Eur Acad Dermatol Venereol. 2007. 21:581–590.
7. Park S, Grossfeld GD, McAninch JW, Santucci R. Extramammary Paget's disease of the penis and scrotum: excision, reconstruction and evaluation of occult malignancy. J Urol. 2001. 166:2112–2116.
8. Chiu TW, Wong PS, Ahmed K, Lam SC, Ying SY, Burd A. Extramammary Paget's disease in Chinese males: a 21-year experience. World J Surg. 2007. 31:1941–1946.
9. Perez MA, LaRossa DD, Tomaszewski JE. Paget's disease primarily involving the scrotum. Cancer. 1989. 63:970–975.
10. Balducci L, Crawford ED, Smith GF, Lambuth B, McGehee R, Hardy C. Extramammary Paget's disease: an annotated review. Cancer Invest. 1988. 6:293–303.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download