Abstract
Purpose
Patients in the intensive care unit (ICU) are usually at greater risk for acquiring urinary tract infection (UTI). Few studies have focused on UTI specifically acquired within the ICU. We retrospectively studied and compared the microbiology and antibiotic sensitivity of UTI in ICU-admitted patients between 2001 and 2008.
Materials and Methods
We reviewed the medical records of a total of 1,818 ICU patients who had undergone a urine culture exam in 2001 and 2008 in a single hospital. Changes in causative organisms and their antibiotic sensitivity between 2001 and 2008 were analyzed.
Results
The common pathogens in 2008 were Escherichia coli (20.3%), Pseudomonas (19.5%), Enterococcus (18.0%), Klebsiella (7.8%), coagulase-negative Staphylococcus (CNS) (4.3%), and Staphylococcus (4.3%). Pseudomonas species significantly increased in 2008 compared with 2001 (p=0.002). Gram-negative organisms showed relatively higher sensitivities to amikacin, imipenem, and Tazocin (72.1%, 76.2%, and 74.6%, respectively), whereas they showed relatively lower sensitivities to third-generation cephalosporins and ciprofloxacin (43% to 59%). Gram-positive organisms showed high sensitivities to teicoplanin and vancomycin (91.2% and 86.8%, respectively), whereas they showed low sensitivities to ampicillin and ciprofloxacin (25% and 26.5%, respectively). The antibiotic resistance of Pseudomonas species was nearly double that of E. coli.
Conclusions
E. coli, Pseudomonas, and Enterococcus were the three most common organisms in ICU-acquired UTI in our study. In particular, Pseudomonas species were found to have increased significantly in recent years. Pseudomonas species had a significantly lower susceptibility to antibiotic sensitivity than did the other organisms.
Figures and Tables
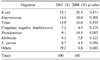
Table 1
Species distribution of the isolates from patients with urinary tract infections in 2001 versus 2008
References
1. Foxman B. Epidemiology of urinary tract infections: incidence, morbidity, and economic costs. Am J Med. 2002. 113:Suppl 1A. 5S–13S.
2. Lizioli A, Privitera G, Alliata E, Antonietta Banfi EM, Boselli L, Panceri ML, et al. Prevalence of nosocomial infections in Italy: result from the Lombardy survey in 2000. J Hosp Infect. 2003. 54:141–148.
3. Eriksen HM, Iversen BG, Aavitsland P. Prevalence of nosocomial infections in hospitals in Norway, 2002 and 2003. J Hosp Infect. 2005. 60:40–45.
4. Vincent JL, Bihari DJ, Suter PM, Bruining HA, White J, Nicolas-Chanoin MH, et al. EPIC International Advisory Committee. The prevalence of nosocomial infection in intensive care units in Europe. Results of the European Prevalence of Infection in Intensive Care (EPIC) Study. JAMA. 1995. 274:639–644.
5. Platt R, Polk BF, Murdock B, Rosner B. Mortality associated with nosocomial urinary-tract infection. N Engl J Med. 1982. 307:637–642.
6. Garner JS, Jarvis WR, Emori TG, Horan TC, Hughes JM. CDC definitions for nosocomial infections, 1988. Am J Infect Control. 1988. 16:128–140.
7. Richards C, Emori TG, Edwards J, Fridkin S, Tolson J, Gaynes R. Characteristics of hospitals and infection control professionals participating in the National Nosocomial Infections Surveillance System 1999. Am J Infect Control. 2001. 29:400–403.
8. Laupland KB, Zygun DA, Davies HD, Church DL, Louie TJ, Doig CJ. Incidence and risk factors for acquiring nosocomial urinary tract infection in the critically ill. J Crit Care. 2002. 17:50–57.
9. Kim SD, Sohn DW, Kim SW, Cho YH. The present status and counterplans of nosocomial infection. Korean J UTII. 2007. 2:1–11.
10. Kim JM, Park ES, Jeong JS, Kim KM, Kim JM, Oh HS, et al. Multicenter surveillance study for nosocomial infections in major hospitals in Korea. Nosocomial Infection Surveillance Committee of the Korean Society for Nosocomial Infection Control. Am J Infect Control. 2000. 28:454–458.
11. Naber KG, Bishop MC, Bjerklund-Johansen TE, Botto H, Cek M, Grabe M, et al. . The management of urinary and genital tract infections. European Association of Urology Guidelines. 2006. Arnhem: Drukkerij Gelderland;1–126.
12. Tissot E, Limat S, Cornette C, Capellier G. Risk factors for catheter-associated bacteriuria in a medical intensive care unit. Eur J Clin Microbiol Infect Dis. 2001. 20:260–262.
13. Laupland KB, Bagshaw SM, Gregson DB, Kirkpatrick AW, Ross T, Church DL. Intensive care unit-acquired urinary tract infections in a regional critical care system. Crit Care. 2005. 9:R60–R65.
14. Gaynes R, Edwards JR. Overview of nosocomial infections caused by gram-negative bacilli. Clin Infect Dis. 2005. 41:848–854.
15. Alvarez-Lerma F, Nolla-Salas J, Leon C, Palomar M, Jorda R, Carrasco N, et al. Candiduria in critically ill patients admitted to intensive care medical units. Intensive Care Med. 2003. 29:1069–1076.
16. Ko HS, Choi DY, Han YT. A study of the changes of antibiotic sensitivity to the causative organisms of urinary tract infection for recent 5 years. Korean J Urol. 1999. 40:809–816.
17. Ko YH, Oh JS, Cho DY, Bea JH, Koh SK. Changes of causative organisms and antimicrobial sensitivity of urinary tract infection between 1979 and 2001. Korean J Urol. 2003. 44:342–350.
18. Ryu KH, Kim MK, Jeong YB. A recent study on the antimicrobial sensitivity of the organisms that cause urinary tract infection. Korean J Urol. 2007. 48:638–645.
19. Kumon H, Ono N, Iida M, Nickel JC. Combination effect of fosfomycin and ofloxacin against Pseudomonas aeruginosa growing in a biofilm. Antimicrob Agents Chemother. 1995. 39:1038–1044.
20. Richards MJ, Edwards JR, Culver DH, Gaynes RP. Nosocomial infections in combined medical-surgical intensive care units in the United States. Infect Control Hosp Epidemiol. 2000. 21:510–515.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download