Abstract
Purpose
Bacillus Calmette-Guérin (BCG) intravesical therapy is the standard treatment in high-risk patients with non-muscle-invasive bladder cancer, but a significant number of patients experience recurrence after BCG therapy. Although several treatment options are available for recurrence after BCG therapy, the optimal treatment strategy is still controversial. We reviewed current and promising treatment options after BCG failure.
Materials and Methods
search of published literature using PubMed and meeting abstracts was performed.
Results
BCG failures are further subdefined as BCG refractory, BCG resistant, BCG relapsing, and BCG intolerance. Several predictors for BCG response have been studied, but prediction or stratification before therapy seems to be difficult in clinical practice. Novel biomarkers associated with immunologic mechanisms appear to be promising to predict BCG failure. Radical cystectomy is the standard treatment for BCG-refractory disease, but the timing of cystectomy is controversial. BCG maintenance or combination with interferon-α is a promising therapy for BCG resistance or relapse. Some salvage therapies or device-assisted instillations have been also promising, but the efficacy and safety of these novel therapies should be confirmed by large prospective studies before their clinical use in BCG failure.
Conclusions
Patients with BCG failure are not a homogeneous group and need to be stratified. Radical cystectomy should be performed without delay in patients with BCG-refractory status, but salvage intravesical therapies may be an alternative in cases without true refractory status. Although BCG and interferon intravesical therapy is promising, more efficient salvage therapy after BCG failure is required.
Since bacillus Calmette-Guérin (BCG) was first used in humans in 1921, its main use has been for vaccination against tuberculosis [1]. However, BCG has also been used in the immunotherapy of cancer or chronic inflammation. Until now, BCG was the most frequently used immunotherapeutic treatment. Morales et al. investigated a new form of application for BCG in 1976 [2]. They developed a schedule for the effective adjuvant intravesical treatment of non-muscle-invasive bladder cancer (NMIBC) after transurethral resection (TUR) with BCG. Since the late 1980s, evidence has become available that instillation of BCG into the bladder is an effective form of immunotherapy in NMIBC.
Recent meta-analyses have confirmed that BCG after TUR is superior to TUR alone or to TUR and chemotherapy in preventing recurrence [3-5]. To date, BCG intravesical therapy is the standard treatment in high-risk patients with NMIBC and in patients with carcinoma in situ (CIS) [6-8]. However, although BCG is the most effective therapy for preventing recurrence and progression in NMIBC, a significant number of patients do experience recurrence and progression after BCG therapy. The treatment fails in 30-40% of patients, and 30-40% of those who initially responded relapse. This status has been generally called "BCG failure" [9].
Several treatment options for recurrence after BCG therapy are available. Radical cystectomy or salvage intravesical therapy can be selectively chosen as the treatment of BCG failure according to disease status. Currently, several agents or treatment protocols are now being investigated for overcoming BCG failure. However, the optimal treatment strategy of BCG failure is still controversial. Therefore, in this article, we review current and promising treatment options after BCG failure.
Although BCG failure is a generally used term for recurrence after BCG therapy in bladder cancer, its definition is not clear. Clear definitions of BCG failure are needed in both the clinical and the research setting. By strict definition, any recurrence of tumor after BCG therapy can be termed a BCG failure, but not all failures under this definition have a similar prognosis [10]. Some series have defined BCG failure after a single induction course of BCG, and others after two courses [11-13]. In addition, most studies have included all patients who received one or more courses of BCG. Investigators have often combined patients with persistent disease and patients with recurrent disease after an initial response, and a few studies have combined patients who were nonresponders to BCG and patients who could not complete BCG therapy because of toxicity [14]. These differences in definition might affect the results of the studies of BCG failure and account for the wide disparity in response rates. In clinical practice, vague definitions make it more difficult for clinicians to decide when to abandon BCG and to start other treatment options.
Recently, efforts have been made to clarify the definition of BCG failure. Herr and Dalbagni suggested definitions to clarify refractory and resistant disease [15]. They reported that the presence of a tumor at the 6-month evaluation after initial BCG was predictive of subsequent tumor recurrence, whereas tumor presence at 3 months was not predictive. These concepts were further stratified into BCG-refractory, BCG-resistant, BCG-relapsing, and BCG-intolerance at the First International Consensus Meeting in 2005 (Table 1) [16]. This subclassification allows clinicians to understand current disease status after adjuvant BCG therapy and can aid clinical decisions about when to abandon BCG and what to choose as the proper treatment option after BCG. The International Bladder Cancer Group emphasized the importance of distinguishing recurrences from treatment failures and also acknowledged that defining the type of BCG failure may be helpful in deciding whether conservative management or cystectomy is required [17]. However, currently updated guidelines of NMIBC still have no consensus about the definition of BCG failure. Much more evidence clinically supporting the subclassifications of the definition will be needed for general consensus.
Several studies have investigated the factors predictive of the BCG response in NMIBC. Although some studies have reported the potential prediction of recurrence or progression after BCG, after more than two decades of study, no independent prognostic factor for remission or relapse after BCG therapy appears to have been identified [18]. However, recent studies have reported novel predictive factors.
Recent multivariate analyses based on large, multicenter bladder cancer patient cohorts of greater than 1,000 patients have suggested some independent predictors for recurrence and progression after BCG induction and short-term maintenance treatment [19]. Analysis from a Spanish group with 1,062 patients with NMIBC suggested that female gender, history of recurrence, multiplicity, and presence of CIS are predictors for recurrence, and age, history of recurrence, high grade, T1 stage, and recurrence at initial cystoscopy are predictors for progression [19].
Microstaging of T1 tumors may help to select tumors with a higher risk of progression. Several reports in the past 10 years have demonstrated a worse prognosis for T1 tumors with deep lamina propria invasion, with progression rates ranging from 29% to 55% [20-22]. Subgrouping of T1 tumors uses the muscularis mucosa as a landmark of microstaging. According to the muscularis mucosa, T1 tumors are classified into T1a when the tumor involves the subepithelial connective tissue superficial to the muscularis mucosa, T1b when it goes into the level of the muscularis mucosa, and T1c when it goes beyond the muscularis mucosa [21]. In a study of 49 patients with T1 bladder cancer, Kondylis et al showed that substaging of T1 tumors did not affect response to BCG regarding recurrence or progression [20]. In contrast, Orsola et al reported that patients with high-grade T1 bladder cancer invading the muscularis mucosa (T1b) had a seven times higher risk of a positive repeat TUR at 3 months after the initial TUR and BCG therapy if the initial tumor was greater than 3 cm and a five-fold increased risk if associated with CIS [21,22]. However, this result has not been confirmed in a prospective study.
Tumor marker expression has been investigated as a predictive factor for recurrence or progression in several cancers with various stages and has also been investigated in bladder cancer treated with BCG, but the results have been inconsistent. Some investigators reported that P53 and Ki-67 protein overexpression are independent predictors for recurrence in NMIBC treated with BCG [23,24], but others have reported no significant associations [25-28]. The results for ezrin protein expression were similarly inconsistent [24,27,29]. Recently, pRb was proposed as a predictive factor of nonresponse and recurrence after BCG plus IFN-α [28]. However, because these markers have not been confirmed by a prospective study, debate about these issues remains.
Various cytokines or cytokine-related parameters have been investigated as a predictive or prognostic factor in NMIBC treated with BCG. These include cytokine gene polymorphisms, tumor necrosis factor-alpha gene, antigen-presenting molecules and chemokines, T helper 1 and 2 lymphocyte urinary cytokine profiles, and urinary interleukin-8 [30-35]. Some reports have shown promising results for cytokines as the predictive factor of BCG response or prognosis, but despite decades of investigation, there are still no molecular markers that predict response to BCG.
Tumor cells are surrounded by infiltrating inflammatory cells, which communicate via a complex network of intercellular signaling pathways. Tumor-associated macrophages (TAMs) can regulate the growth of various cancers either positively or negatively. Takayama et al investigated the prognostic role of TAMs in CIS after BCG by measuring the cancer cell-to-lamina propria TAM ratio [36]. In that study, higher cancer cell TAM counts and higher cancer cell-to-lamina propria TAM ratio were independent prognostic factors for recurrence after BCG. Ayari et al performed a similar study with TAMs and tumor-infiltrating dendritic cells (TIDCs) [37]. They demonstrated that a high level of infiltration by CD83 (+) TIDCs or CD68 (+) TAMs does not respond as well to BCG immunotherapy. These two studies emphasize the prognostic significance of tumor-infiltrating immune cells for the response to BCG, but large, prospective studies are required to confirm these findings.
Patients with T1G3 bladder cancer have a markedly varied potential for tumor progression, whereas more than a third do not experience recurrence or progression. Radical cystectomy may be the best treatment in high-risk patients but is an overtreatment in patients who will have no recurrence or progression. Therefore, patient selection might be important to manage patients who fail BCG therapy. Several salvage therapies after failure of BCG have been studied, and some therapies have shown promising results as second-line intravesical therapy after BCG.
Currently, radical cystectomy with pelvic lymph node dissection is the standard treatment for patients who have failed BCG. This treatment provides a good 5-year survival rate of 70-90%, and orthotopic neobladder reconstruction has been established as the standard procedure that provides good quality of life [10,38]. However, cystectomy yields a 2-3% mortality rate and 20-30% complication rates. Some patients who undergo cystectomy may suffer when adjusting to postoperative changes in their quality of life. Early cystectomy would be an overtreatment, even in high-risk patients, because more than one third of T1G3 bladder cancer patients do not experience recurrence or progression.
The most debatable issue is when cystectomy should be performed [38]. No prospective randomized trial has evaluated the optimal timing of cystectomy in these patients. The timing of cystectomy is an important prognostic factor. Several studies have emphasized the risk of delayed cystectomy in high-risk NMIBC. One study of BCG plus interferon-α (IFN-α) in 1,106 NMIBC patients suggested that the timing of BCG failure is a significant predictor for subsequent recurrence [39]. In that study, patients with disease recurrence more than 1 year after BCG treatment and who were treated with low-dose BCG plus interferon-alpha had response rates similar to those of BCG-naïve patients treated with regular-dose BCG plus interferon (Fig. 1) [39]. From this result, the authors suggested that patients with BCG failure more than 1 year after BCG might benefit from another trial with intravesical immunotherapy, whereas patients with recurrence within 1 year of BCG should be considered for either cystectomy or alternative intravesical therapies. In addition, a recent historical comparative study suggested that a paradigm shift has occurred because patients are increasingly offered radical cystectomy before disease progression to muscle invasion [40]. As a result, the disease-specific death of the contemporary cohort in which preemptive radical cystectomy was performed was less than that of the historical cohort in which the bladder was preserved until progression to muscle invasion [40]. Another study demonstrated that patients who underwent surgery less than 2 years after initial transurethral resection of bladder tumor (TURBT) for high-risk NMIBC had a significantly improved survival compared with similar patients who had surgery after 2 years [41-43]. Herr et al have suggested that tumor response at 6 months was the most important factor for predicting ultimate failure and progression [42]. Therefore, it is recommended that cystectomy should not be delayed in high-risk patients beyond 6 months (two courses of BCG) [38].
Radical cystectomy allows us to overcome the clinical limitation of under-staging and thus can help to direct appropriate therapy for more advanced tumors earlier in the time course. Proponents of early cystectomy point out that a significant proportion of patients who undergo delayed cystectomy subsequently die of the disease, and a significant proportion of patients who progress during conservative management had resectable disease at the time of cystectomy, which dramatically increased the risk of death [38]. The proponents of early cystectomy also note that conservative management mandates life-long surveillance that includes routine cystoscopy, as well as radiographic evaluation and adjuvant therapies, as dictated by recurrences [38]. However, no reliable data have been published regarding the cost savings of early cystectomy versus conservative management at this time. Furthermore, the issue of the quality of life of patients undergoing long-term surveillance, in particular the effects of the anxiety associated with this option, compared with the postoperative quality of life challenges associated with cystectomy, has not been adequately studied to date.
Although each additional course of BCG carries a 7% actuarial risk of progression after BCG failure, as many as 40-80% of patients who appear to have failed the initial BCG therapy show a durable response after a second course of BCG [44,45]. Therefore, patients should not be considered a true failure if they have received only one course of BCG. Another course of BCG can be applied to these patients, whereas patients who have evidence of disease after two courses are unlikely to respond to additional BCG therapy and are at risk for progression of disease [10]. These patients, who were classified as BCG refractory, are "true BCG failures" and treatment options other than BCG should be considered. Patients who delay definitive therapy by receiving two doses of initiation therapy or an alternative treatment for BCG-refractory disease may be at increased risk for progression with a proportionate decrease in long-term survival and, therefore, early cystectomy is the best choice of treatment in these patients [10,17,38,41].
Although the merits of a maintenance course have been debated in the past, BCG maintenance is highly recommended as the standard adjuvant treatment in high-risk NMIBC [10]. With increasing data showing its benefits, a maintenance course of BCG at 3 months is currently accepted. Meta-analyses showed that induction BCG followed by maintenance BCG decreases recurrence in high-risk patients, although most patients did not complete the entire course to 36 months [46,47]. However, Herr pointed to the bias included in these meta-analyses, which exaggerated the efficacy of BCG maintenance, and insisted that critical analysis of the evidence does not support the liberal use of maintenance BCG as currently practiced and recommended [48]. Herr suggested that maintenance BCG does not appear superior to initial BCG treatment in preventing or delaying tumor progression and that prolonged BCG treatment adds toxicity [48]. However, the decision for maintenance of BCG after BCG failure must depend on disease status. BCG maintenance is not optimal in patients with BCG-refractory status, but is recommended as the adjuvant treatment after an additional BCG induction course in patients with BCG resistance or relapse, or even in patients with BCG-intolerance.
Interest in interferon as an intravesical agent against bladder cancer developed in the 1980s [41]. Results of early prospective series with interferon were disappointing. The long-term success rate of IFN-α monotherapy of BCG failures is generally less than 15% [49]. Furthermore, one study of IFN-α found it to be no better than water placebo at 43 months of follow-up, which suggests that it has no role in recurrent stage T1 disease [50]. However, over the subsequent decade, sufficient experience with both agents accumulated to suggest using them together as salvage therapy in patients with recurrence after intravesical BCG.
A large, national, multicenter phase II trial assessed the efficacy of the combination of BCG and interferon [51]. This trial showed that this combination therapy is well tolerated and appears to prolong the disease-free interval in previous BCG-failure patients. With a median follow-up of 24 months, 45% of BCG failures remained recurrence-free compared with 59% in the BCG-naïve group treated with a normal dose of BCG (Fig. 2). Although the definition of BCG failure was quite liberal and included some BCG-intolerant patients, this trial showed that the combination of BCG and IFN seems a promising second-line immunotherapy regimen after BCG failures, but the results of this phase II trial should be confirmed [10].
Several intravesical drugs have been investigated in high-risk patients who failed BCG. Conventional intravesical chemotherapeutic agents have been investigated in a few studies but did not show satisfactory efficacy. Platinum derivatives have been tried but were generally too irritating and associated with occasional fatal anaphylaxis [52]. Recently, two newer cytotoxic chemotherapeutic drugs, gemcitabine and docetaxel, with known systemic activity against advanced bladder cancer have been tried in the intravesical route.
Only a few attempts have been made to treat BCG failures with conventional intravesical chemotherapy. The Swedish-Norwegian Bladder Cancer Group compared mitomycin C (MMC) and BCG in NMIBC patients, and treatment failures were allowed to cross over to the other treatment [53]. Twenty-one patients with BCG failure changed to MMC therapy, but only four remained recurrence free with a median follow-up period of 64 months. Conventional intravesical chemotherapy generally appears to not be effective in BCG tolerance.
Valrubicin, a new anthracycline derivative, is the only drug approved by the US Federal Drug Administration (FDA) for patients with CIS failing BCG therapy [54]. The FDA approval of this agent was based on a small phase II trial with 90 patients. After a 1-year follow-up, only 21% showed a complete response and only 8% were disease free at the 2-year follow-up [55]. A marker lesion study in refractory patients confirmed some potential of valrubicin, with 18 of 39 (46%) patients free of disease after 3 months. However, valrubicin was withdrawn from the market in 2002 because of impurities in its original formulation and is therefore not currently used.
Gemcitabine is a novel deoxycytidine analogue with a broad spectrum of antitumor activity [41]. To date, gemcitabine is one of the standard chemotherapeutical agents in systemic therapy for advanced bladder cancer and also has been studied for its potential for intravesical use for NMIBC. Intravesical gemcitabine has been generally well tolerated with minimal induction of cystitis and little systemic absorption. The exception has been in patients who received previous multiple treatments, where gemcitabine intolerance was seen in 8 of 64 (13%) patients, necessitating withdrawal [56].
The first phase I study in 18 patients refractory to BCG and treated with gemcitabine on refusing cystectomy reported that intravesical gemcitabine therapy given twice weekly was associated with minimal bladder irritation and tolerable myelosuppression [57]. Activity against marker lesions and primary and previous refractory tumors has been demonstrated in multiple phase I and phase II trials with gemcitabine, and the marker lesion response varies, with the highest response rate reported of 56% [57-61]. In a phase II trial of gemcitabine for BCG refractory patients, Bartoletti et al. reported that when 2,000 mg gemcitabine in 50 ml was used, 18 of 24 (75%) intermediate-risk and 7 of 16 (43.7%) high-risk BCG-refractory patients remained recurrence free [59]. Also, Dalbagni et al conducted a phase II study using a more intensive, twice-weekly administration in 30 BCG-refractory patients and reported that with a median follow-up of 19 months, 15 of 30 (50%) had an initial complete response [62]. These studies have confirmed the potential of gemcitabine in these patients. However, in the largest most dose-intensive regimen with the longest follow-up, the 1-year complete response rate was only 21%, suggesting that single-agent gemcitabine will not likely meet its role as a universal salvage drug [14].
Docetaxel is a chemotherapeutic agent that has recently been investigated for intravesical therapy. A phase I trial showed that docetaxel is safe for intravesical therapy in patients with BCG-refractory NMIBC, with no systemic absorption and limited toxicity. Of the 18 patients, 56% had no evidence of disease at the cystoscopy and biopsy after treatment, and 22% remained disease free during the median 32.5 months of follow-up [63]. There has been no phase II trial, but recently, an extended report for intravesical docetaxel was made by the same group [64]. In that study, monthly maintenance therapy with intravesical docetaxel was performed in 13 patients with BCG refractory Ta, T1, or CIS to overcome the low durability in the previous study. With a median 13 months of follow-up, 10 of 13 patients had a complete response after induction, and 6 have remained disease-free. All 10 responders completed at least three instillations of maintenance, of whom 6 have remained recurrence-free. In summary, intravesical docetaxel is tolerable and has shown promising results in patients with BCG failures, but a phase II study should be performed to confirm its efficacy.
Although multi-agent chemotherapy has become universal for almost all cases of systemic chemotherapy, previous attempts to use combined or alternating older chemotherapy drugs, such as adriamycin and mitomycin, intravesically were frustrated by severe cystitis despite some evidence of enhanced activity [14]. However, combinations of drugs in which one or both are non-vesicants may be better received [14]. One such combination of immediate sequential gemcitabine followed by mitomycin reported a near 50% recurrence-free rate in 27 BCG refractory patients at 18 months compared with 20% for gemcitabine alone in 12 similar patients [65]. Further prospective studies with combinations of other intravesical chemotherapeutic agents including gemcitabine and docetaxel deserve to be carried out.
Although intravesical chemotherapy is not a standard treatment option in BCG failures, intravesical chemotherapy combined with an energy source might be better. Combining intravesical chemotherapy with an energy source can improve drug delivery. Device-assisted instillations using novel devices such as electromotive drug administration (EDMA), thermotherapy, and photodynamic therapy have also been investigated and have shown favorable results but are still in phase I trials.
The feasibility and safety of both techniques were compared and tested as four weekly ablative sessions before TUR in 15 patients [66]. Di Stasi et al and colleagues conducted a randomized controlled trial of sequential electromotive MMC in high-risk patients [67]. In that study, 212 patients with pT1 bladder cancer were randomly assigned to conventional BCG induction cycle or to BCG followed by electromotive MMC once per week for three cycles followed by maintenance treatment. Patients assigned sequential BCG and electromotive MMC had a higher disease-free interval and lower recurrence than did patients assigned BCG alone [67]. This combination of chemotherapy and EMDA appears to be promising in high-risk patients but has not been investigated in BCG failure yet. The BCG failure group would be the next reasonable study population for this combination therapy.
The combination of intravesical hyperthermia and MMC has also been studied recently. This treatment combines heating of the bladder wall to a temperature of around 42℃ with a cooled solution of MMC. Several studies have shown that thermochemotherapy and MMC is superior to MMC alone and can be used both to prevent recurrences and as ablative treatment [54,68]. Thermochemotherapy has also been reported to be successful in BCG failures [69,70]. In a study of CIS patients, most of whom had failed BCG, treated with MMC combined with hyperthermia, Alfred et al reported a response rate of 92% at the initial cystoscopy with biopsies 3 months after treatment, and 51% of patients remained recurrence-free at a median follow-up of 27 months. However, longer follow-up and more results are required to indicate the value of thermochemotherapy in patients with BCG failures [70].
Photodynamic therapy (PDT) is a minimally invasive therapeutic modality approved for the treatment of several cancers [71]. PDT involves the administration of a tumor-localizing photosensitizer followed by its activation with light of a specific wavelength. In the presence of tissue oxygen, the photoactive sensitizer triggers a series of photochemical and photobiological processes that may lead to direct cancer cell damage, tumor microvascular occlusion, and host immune response [72]. Waidelich et al performed PDT after the oral administration of 5-aminolevulinic acid (5-ALA) in 24 patients with BCG-refractory bladder cancer [73]. In that study, at a median follow-up of 36 months, 3 of 5 patients with CIS and 4 of 19 with papillary tumors were recurrence free. Tumor progression was stopped in 20 of 24 cases. Hypotension and tachycardia occurred in 19 and 10 patients, respectively, immediately after the oral administration of 5-ALA. Berger et al reported the results of PDT in 31 patients including 10 BCG failure patients [74]. In the 10 BCG failure patients treated by PDT, 40% were free of recurrence after a mean follow-up of 11.8 months. These initial clinical results suggest that PDT with oral 5-ALA may be effective in BCG failure. However, systemic side effects such as hemodynamic instability after oral ALA, particularly in patients with cardiovascular co-morbidity, should be overcome.
Recently, the Harvard Radiation Oncology Group reported their experiences of bladder-sparing trimodality therapy in high-risk NMIBC patients who have progressed to muscle-invasive disease [75]. The bladder-intact survival rate at 3, 5, and 7 years was 61%, 54%, and 54%, respectively. Although this was a small retrospective study, their favorable results suggest that concurrent chemoradiation therapy can be used in the management of high-risk T1 bladder cancer. However, there has been no study of chemoradiation therapy in BCG failure patients.
Patients with BCG failures are not a homogeneous group and need to be stratified through the assessment of a potential response for further BCG and future progression risk. Novel biomarkers or cells associated with immunologic mechanisms appear to be promising to predict BCG failure, but there is still a long way to go. Radical cystectomy should be performed without delay in patients with BCG-refractory status, but salvage intravesical therapies may be an alternative option in patients without true refractory status. Although some salvage intravesical therapies including BCG plus IFN-α are promising and are being investigated, more efficient and powerful treatments appear to be required in the management of BCG failures.
Figures and Tables
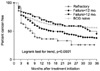 | Fig. 1Cancer-free survival rates for bacillus Calmette-Guérin (BCG)-naïve and BCG-failure patients with different failure patterns ([39] Gallagher, et al. Urology 2008;71:297-301. reproduced with permission of the publisher, Elsevier). |
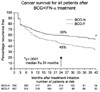 | Fig. 2Kaplan-Meier recurrence rates in patients receiving intravesical bacillus Calmette-Guérin (BCG) and interferon (IFN) characterized by whether they had never received BCG (BCG-N) or had tumor recurrence after prior BCG (BCG-F). ([51] Joudi, et al. Urol Oncol 2006;24:344-8. reproduced with permission of the publisher, Elsevier). |
References
1. Brandau S, Suttmann H. Thirty years of BCG immunotherapy for non-muscle invasive bladder cancer: a success story with room for improvement. Biomed Pharmacother. 2007. 61:299–305.
2. Morales A, Eidinger D, Bruce AW. Intracavitary bacillus Calmette-Guérin in the treatment of superficial bladder tumors. J Urol. 1976. 116:180–183.
3. Shelley MD, Kynaston H, Court J, Wilt TJ, Coles B, Burgon K, et al. A systematic review of intravesical bacillus Calmette-Guérin plus transurethral resection vs transurethral resection alone in Ta and T1 bladder cancer. BJU Int. 2001. 88:209–216.
4. Han RF, Pan JG. Can intravesical bacillus Calmette-Guérin reduce recurrence in patients with superficial bladder cancer? A meta-analysis of randomized trials. Urology. 2006. 67:1216–1223.
5. Böhle A, Jocham D, Bock PR. Intravesical bacillus Calmette-Guerin versus mitomycin C for superficial bladder cancer: a formal meta-analysis of comparative studies on recurrence and toxicity. J Urol. 2003. 169:90–95.
6. Hong SJ, Choi HY, Ahn HJ, Kim CS, Yang WJ. Effect of intravesical high dose epirubicin versus bacillus Calmette-Guerin instillation on the recurrence and progression of superficial bladder cancer: a prospective, multicenter study. Korean J Urol. 2005. 46:677–682.
7. Park JW, Park CH, Kim CI. Superficial bladder carcinoma treated with Bacillus Calmette-Guerin: minimum 5-year follow up results. Korean J Urol. 2003. 44:573–578.
8. Park JO, Kim DS, Yoon DK, Cho JH. A long term effects of single 6-week intravesical bcg therapy for the recurrence and progression of stage T1 bladder cancer. Korean J Urol. 2000. 41:1–7.
9. Palou Redorta J. Management of BCG "Failures". Eur Urol. 2006. 49:779–780.
10. Martin FM, Kamat AM. Definition and management of patients with bladder cancer who fail BCG therapy. Expert Rev Anticancer Ther. 2009. 9:815–820.
11. Klein EA, Rogatko A, Herr HW. Management of local bacillus Calmette-Guerin failures in superficial bladder cancer. J Urol. 1992. 147:601–605.
12. Glashan RW. A randomized controlled study of intravesical alpha-2b-interferon in carcinoma in situ of the bladder. J Urol. 1990. 144:658–661.
13. Sarosdy MF, Manyak MJ, Sagalowsky AI, Belldegrun A, Benson MC, Bihrle W, et al. Oral bropirimine immunotherapy of bladder carcinoma in situ after prior intravesical bacille Calmette-Guerin. Urology. 1998. 51:226–231.
14. O'Donnell MA, Boehle A. Treatment options for BCG failures. World J Urol. 2006. 24:481–487.
15. Herr HW, Dalbagni G. Defining bacillus Calmette-Guerin refractory superficial bladder tumors. J Urol. 2003. 169:1706–1708.
16. Sengupta S, Blute ML. The management of superficial transitional cell carcinoma of the bladder. Urology. 2006. 67:3 Suppl 1. 48–54.
17. Lamma D, Colombel M, Persad R, Soloway M, Böhle A, Palou J, et al. Clinical practice recommendations for the management of non-muscle invasive bladder cancer. Eur Urol. 2008. 7:Suppl. 651–666.
18. Saint F, Salomon L, Quintela R, Cicco A, Hoznek A, Abbou CC, et al. Do prognostic parameters of remission versus relapse after Bacillus Calmette-Géurin (BCG) immunotherapy exist?. analysis of a quarter century of literature. Eur Urol. 2003. 43:351–360.
19. Fernandez-Gomez J, Solsona E, Unda M, Martinez-Piñeiro L, Gonzalez M, Hernandez R, et al. Prognostic factors in patients with non-muscle-invasive bladder cancer treated with bacillus Calmette-Guérin: multivariate analysis of data from four randomized CUETO trials. Eur Urol. 2008. 53:992–1001.
20. Kondylis FI, Demirci S, Ladaga L, Kolm P, Schellhammer PF. Outcomes after intravesical bacillus Calmette-Guerin are not affected by substaging of high grade T1 transitional cell carcinoma. J Urol. 2000. 163:1120–1123.
21. Orsola A, Trias I, Raventós CX, Español I, Cecchini L, Búcar S, et al. Initial high-grade T1 urothelial cell carcinoma: feasibility and prognostic significance of lamina propria invasion microstaging (T1a/b/c) in BCG-treated and BCG-non-treated patients. Eur Urol. 2005. 48:231–238.
22. Orsola A, Cecchini L, Raventós CX, Trilla E, Planas J, Landolfi S, et al. Risk factors for positive findings in patients with high-grade T1 bladder cancer treated with transurethral resection of bladder tumour (TUR) and bacille Calmette-Guérin therapy and the decision for a repeat TUR. BJU Int. 2009. Epub ahead of print.
23. Saint F, Le Frere Belda MA, Quintela R, Hoznek A, Patard JJ, Bellot J, et al. Pretreatment p53 nuclear overexpression as a prognostic marker in superficial bladder cancer treated with Bacillus Calmette-Guérin (BCG). Eur Urol. 2004. 45:475–482.
24. Lebret T, Becette V, Hervé JM, Molinié V, Barré P, Lugagne PM, et al. Prognostic value of MIB-1 antibody labeling index to predict response to Bacillus Calmette-Guérin therapy in a high-risk selected population of patients with stage T1 grade G3 bladder cancer. Eur Urol. 2000. 37:654–659.
25. Lacombe L, Dalbagni G, Zhang ZF, Cordon-Cardo C, Fair WR, Herr HW, et al. Overexpression of p53 protein in a high-risk population of patients with superficial bladder cancer before and after bacillus Calmette-Guérin therapy: correlation to clinical outcome. J Clin Oncol. 1996. 14:2646–2652.
26. Lebret T, Becette V, Barbagelatta M, Hervé JM, Gaudez F, Barré P, et al. Correlation between p53 over expression and response to bacillus Calmette-Guerin therapy in a high risk select population of patients with T1G3 bladder cancer. J Urol. 1998. 159:788–791.
27. Zlotta AR, Noel JC, Fayt I, Drowart A, Van Vooren JP, Huygen K, et al. Correlation and prognostic significance of p53, p21WAF1/CIP1 and Ki-67 expression in patients with superficial bladder tumors treated with bacillus Calmette-Guerin intravesical therapy. J Urol. 1999. 161:792–798.
28. Esuvaranathan K, Chiong E, Thamboo TP, Chan YH, Kamaraj R, Mahendran R, et al. Predictive value of p53 and pRb expression in superficial bladder cancer patients treated with BCG and interferon-alpha. Cancer. 2007. 109:1097–1105.
29. Palou J, Algaba F, Vera I, Rodriguez O, Villavicencio H, Sanchez-Carbayo M. Protein expression patterns of ezrin are predictors of progression in T1G3 bladder tumours treated with nonmaintenance Bacillus Calmette-Guérin. Eur Urol. 2008. Epub ahead of print.
30. Thalmann GN, Dewald B, Baggiolini M, Studer UE. Interleukin-8 expression in the urine after bacillus Calmette-Guerin therapy: a potential prognostic factor of tumor recurrence and progression. J Urol. 1997. 158:1340–1344.
31. Thalmann GN, Sermier A, Rentsch C, Möhrle K, Cecchini MG, Studer UE. Urinary interleukin-8 and 18 predict the response of superficial bladder cancer to intravesical therapy with bacillus Calmette-Guerin. J Urol. 2000. 164:2129–2133.
32. Saint F, Kurth N, Maille P, Vordos D, Hoznek A, Soyeux P, et al. Urinary IL-2 assay for monitoring intravesical bacillus Calmette-Guérin response of superficial bladder cancer during induction course and maintenance therapy. Int J Cancer. 2003. 107:434–440.
33. Saint F, Patard JJ, Maille P, Soyeux P, Hoznek A, Salomon L, et al. Prognostic value of a T helper 1 urinary cytokine response after intravesical bacillus Calmette-Guerin treatment for superficial bladder cancer. J Urol. 2002. 167:364–367.
34. Saint F, Patard JJ, Maille P, Soyeux P, Hoznek A, Salomon L, et al. T helper 1/2 lymphocyte urinary cytokine profiles in responding and nonresponding patients after 1 and 2 courses of bacillus Calmette-Guerin for superficial bladder cancer. J Urol. 2001. 166:2142–2147.
35. Kumar A, Dubey D, Bansal P, Mandhani A, Naik S. Urinary interleukin-8 predicts the response of standard and low dose intravesical bacillus Calmette-Guerin (modified Danish 1331 strain) for superficial bladder cancer. J Urol. 2002. 168:2232–2235.
36. Takayama H, Nishimura K, Tsujimura A, Nakai Y, Nakayama M, Aozasa K, et al. Increased infiltration of tumor associated macrophages is associated with poor prognosis of bladder carcinoma in situ after intravesical bacillus Calmette-Guerin instillation. J Urol. 2009. 181:1894–1900.
37. Ayari C, LaRue H, Hovington H, Decobert M, Harel F, Bergeron A, et al. Bladder tumor infiltrating mature dendritic cells and macrophages as predictors of response to bacillus Calmette-Guérin immunotherapy. Eur Urol. 2009. 55:1386–1395.
38. Metwalli AR, Kamat AM. Controversial issues and optimal management of stage T1G3 bladder cancer. Expert Rev Anticancer Ther. 2006. 6:1283–1294.
39. Gallagher BL, Joudi FN, Maymí JL, O'Donnell MA. Impact of previous bacille Calmette-Guérin failure pattern on subsequent response to bacille Calmette-Guérin plus interferon intravesical therapy. Urology. 2008. 71:297–301.
40. Raj GV, Herr H, Serio AM, Donat SM, Bochner BH, Vickers AJ, et al. Treatment paradigm shift may improve survival of patients with high risk superficial bladder cancer. J Urol. 2007. 177:1283–1286.
41. Grossman HB, O'Donnell MA, Cookson MS, Greenberg RE, Keane TE. Bacillus Calmette-Guérin failures and beyond: contemporary management of non-muscle-invasive bladder cancer. Rev Urol. 2008. 10:281–289.
42. Herr HW, Sogani PC. Does early cystectomy improve the survival of patients with high risk superficial bladder tumors? J Urol. 2001. 166:1296–1299.
43. Mahmud SM, Fong B, Fahmy N, Tanguay S, Aprikian AG. Effect of preoperative delay on survival in patients with bladder cancer undergoing cystectomy in Quebec: a population based study. J Urol. 2006. 175:78–83.
44. Lamm D. Improving patient outcomes: optimal BCG treatment regimen to prevent progression in superficial bladder cancer. Eur Urol. 2006. 5:Suppl. 654–659.
45. Bui TT, Schellhammer PF. Additional bacillus Calmette-Guérin therapy for recurrent transitional cell carcinoma after an initial complete response. Urology. 1997. 49:687–690.
46. Sylvester RJ, van der Meijden AP, Lamm DL. Intravesical bacillus Calmette-Guerin reduces the risk of progression in patients with superficial bladder cancer: a meta-analysis of the published results of randomized clinical trials. J Urol. 2002. 168:1964–1970.
47. Böhle A, Bock PR. Intravesical bacille Calmette-Guérin versus mitomycin C in superficial bladder cancer: formal meta-analysis of comparative studies on tumor progression. Urology. 2004. 63:682–686.
48. Herr HW. Is maintenance bacillus Calmette-Guérin really necessary? Eur Urol. 2008. 54:971–973.
49. Belldegrun AS, Franklin JR, O'Donnell MA, Gomella LG, Klein E, Neri R, et al. Superficial bladder cancer: the role of interferon-alpha. J Urol. 1998. 159:1793–1801.
50. Portillo J, Martin B, Hernandez R, Correas M, Gutierrez J, Del Valle J, et al. 2: Results at 43 months' follow-up of a double-blind, randomized, prospective clinical trial using intravesical interferon alpha-2b in the prophylaxis of stage pT1 transitional cell carcinoma of the bladder. Urology. 1997. 49:187–190.
51. Joudi FN, Smith BJ, O'Donnell MA. Final results from a national multicenter phase II trial of combination bacillus Calmette-Guérin plus interferon alpha-2B for reducing recurrence of superficial bladder cancer. Urol Oncol. 2006. 24:344–348.
52. Bouffioux C, Denis L, Oosterlinck W, Viggiano G, Vergison B, Keuppens F, et al. The European Organization for Research on Treatment of Cancer Genitourinary Group. Adjuvant chemotherapy of recurrent superficial transitional cell carcinoma: results of a European organization for research on treatment of cancer randomized trial comparing intravesical instillation of thiotepa, doxorubicin and cisplatin. J Urol. 1992. 148:297–301.
53. Malmström PU, Wijkström H, Lundholm C, Wester K, Busch C, Norlén BJ. Swedish-Norwegian Bladder Cancer Study Group. 5-year followup of a randomized prospective study comparing mitomycin C and bacillus Calmette-Guerin in patients with superficial bladder carcinoma. J Urol. 1999. 161:1124–1127.
54. Witjes JA. Management of BCG failures in superficial bladder cancer: a review. Eur Urol. 2006. 49:790–797.
55. Steinberg G, Bahnson R, Brosman S, Middleton R, Wajsman Z, Wehle M. The Valrubicin Study Group. Efficacy and safety of valrubicin for the treatment of Bacillus Calmette-Guerin refractory carcinoma in situ of the bladder. J Urol. 2000. 163:761–767.
56. Morabito F, Rossi R, Graziano ME, Ferrando U, Lancini V, Cretarola E, et al. Multicenter study on the use of gemcitabine to prevent recurrence of multiple-recurring superficial bladder tumors following intravesical antiblastic agents and/or BCG: evaluation of tolerance. Arch Ital Urol Androl. 2006. 78:1–4.
57. Dalbagni G, Russo P, Sheinfeld J, Mazumdar M, Tong W, Rabbani F, et al. Phase I trial of intravesical gemcitabine in bacillus Calmette-Guérin-refractory transitional-cell carcinoma of the bladder. J Clin Oncol. 2002. 20:3193–3198.
58. Gontero P, Casetta G, Maso G, Sogni F, Pretti G, Zitella A, et al. Phase II study to investigate the ablative efficacy of intravesical administration of gemcitabine in intermediate-risk superficial bladder cancer (SBC). Eur Urol. 2004. 46:339–343.
59. Bartoletti R, Cai T, Gacci M, Giubilei G, Viggiani F, Santelli G, et al. Intravesical gemcitabine therapy for superficial transitional cell carcinoma: results of a Phase II prospective multicenter study. Urology. 2005. 66:726–731.
60. Bassi P, De Marco V, Tavolini IM, Longo F, Pinto F, Zucchetti M, et al. Pharmacokinetic study of intravesical gemcitabine in carcinoma in situ of the bladder refractory to bacillus Calmette-Guérin therapy. Urol Int. 2005. 75:309–313.
61. Gacci M, Bartoletti R, Cai T, Nerozzi S, Pinzi N, Repetti F, et al. Intravesical gemcitabine in BCG-refractory T1G3 transitional cell carcinoma of the bladder: a pilot study. Urol Int. 2006. 76:106–111.
62. Dalbagni G, Russo P, Bochner B, Ben-Porat L, Sheinfeld J, Sogani P, et al. Phase II trial of intravesical gemcitabine in bacille Calmette-Guérin-refractory transitional cell carcinoma of the bladder. J Clin Oncol. 2006. 24:2729–2734.
63. McKiernan JM, Masson P, Murphy AM, Goetzl M, Olsson CA, Petrylak DP, et al. Phase I trial of intravesical docetaxel in the management of superficial bladder cancer refractory to standard intravesical therapy. J Clin Oncol. 2006. 24:3075–3080.
64. Barlow L, McKiernan J, Sawczuk I, Benson M. A single-institution experience with induction and maintenance intravesical docetaxel in the management of non-muscle-invasive bladder cancer refractory to bacille Calmette-Guérin therapy. BJU Int. 2009. 104:1098–1102.
65. Maymi JL, Saltsgaver N, O'Donell MA. Intravesical sequential gemcitabine-mitomycin chemotherapy as salvage treatment for patients with refractory superficial bladder cancer. J Urol. 2006. 175:271. abstract 840.
66. Colombo R, Brausi M, Da Pozzo L, Salonia A, Montorsi F, Scattoni V, et al. Thermo-chemotherapy and electromotive drug administration of mitomycin C in superficial bladder cancer eradication. a pilot study on marker lesion. Eur Urol. 2001. 39:95–100.
67. Di Stasi SM, Giannantoni A, Giurioli A, Valenti M, Zampa G, Storti L, et al. Sequential BCG and electromotive mitomycin versus BCG alone for high-risk superficial bladder cancer: a randomised controlled trial. Lancet Oncol. 2006. 7:43–51.
68. Gofrit ON, Shapiro A, Pode D, Sidi A, Nativ O, Leib Z, et al. Combined local bladder hyperthermia and intravesical chemotherapy for the treatment of high-grade superficial bladder cancer. Urology. 2004. 63:466–471.
69. van der Heijden AG, Kiemeney LA, Gofrit ON, Nativ O, Sidi A, Leib Z, et al. Preliminary European results of local microwave hyperthermia and chemotherapy treatment in intermediate or high risk superficial transitional cell carcinoma of the bladder. Eur Urol. 2004. 46:65–71.
70. Alfred Witjes J, Hendricksen K, Gofrit O, Risi O, Nativ O. Intravesical hyperthermia and mitomycin-C for carcinoma in situ of the urinary bladder: experience of the European Synergo working party. World J Urol. 2009. 27:319–324.
71. Juarranz A, Jaén P, Sanz-Rodríguez F, Cuevas J, González S. Photodynamic therapy of cancer. Basic principles and applications. Clin Transl Oncol. 2008. 10:148–154.
72. Zuluaga MF, Lange N. Combination of photodynamic therapy with anti-cancer agents. Curr Med Chem. 2008. 15:1655–1673.
73. Waidelich R, Stepp H, Baumgartner R, Weninger E, Hofstetter A, Kriegmair M. Clinical experience with 5-aminolevulinic acid and photodynamic therapy for refractory superficial bladder cancer. J Urol. 2001. 165:1904–1907.
74. Berger AP, Steiner H, Stenzl A, Akkad T, Bartsch G, Holtl L. Photodynamic therapy with intravesical instillation of 5-aminolevulinic acid for patients with recurrent superficial bladder cancer: a single-center study. Urology. 2003. 61:338–341.
75. Wo JY, Shipley WU, Dahl DM, Coen JJ, Heney NM, Kaufman DS, et al. The results of concurrent chemoradiotherapy for recurrence after treatment with bacillus Calmette-Guérin for non-muscle-invasive bladder cancer: is immediate cystectomy always necessary? BJU Int. 2009. 104:179–183.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download