Abstract
Purpose
Dysfunctional voiding is closely related to constipation, and accurate evaluation of constipation is important. We investigated the accuracy and reliability of several methods that are used to evaluate constipation.
Materials and Methods
We collected data from the parents of 168 dysfunctional voiders, and the data was collected using the Bristol stool form scale and the Leech method. We then analyzed the results of the questionnaire and compared them with the Paris Consensus on Childhood Constipation Terminology (PACCT).
Results
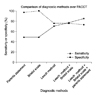
Among the 168 dysfunctional voiders, 71 (42%) were diagnosed with constipation according to PACCT. Of the 39 children who were considered constipated, none were constipated according to PACCT. However, 35 of the 129 children whose parents denied they were constipation were in fact diagnosed with constipation. When the Leech method and the Bristol stool form scale were both used, the sensitivity of diagnosis rose to as high as 75%, and when the statement of the guardian was added, the sensitivity rose to as high as 85%.
Conclusions
Since constipation can be a rather subjective condition, it would be appropriate to respect and incorporate the parents' statement into the diagnosis. However, for making a more accurate diagnosis, comprehensive evaluation based on specific symptoms and the Bristol stool form scale and the Leech method may be helpful.
Figures and Tables
References
1. Chase JW, Homsy Y, Siggaard C, Sit F, Bower WF. Functional constipation in children. J Urol. 2004. 171:2641–2643.
2. Neumann PZ, DeDomenico IJ, Nogrady MB. Constipation and urinary tract infection. Pediatrics. 1973. 52:241–245.
3. Loening-Baucke V. Urinary incontinence and urinary tract infection and their resolution with treatment of chronic constipation of childhood. Pediatrics. 1997. 100:228–232.
4. Benninga M, Candy DC, Catto-Smith AG, Clayden G, Loening-Baucke V, Di Lorenzo C, et al. The Paris consensus on childhood constipation terminology (PACCT) group. J Pediatr Gastroenterol Nutr. 2005. 40:273–275.
5. Riegler G, Esposito I. Bristol scale stool form. A still valid help in medical practice and clinical research. Tech Coloproctol. 2001. 5:163–164.
6. Leech SC, McHugh K, Sullivan PB. Evaluation of a method of assessing faecal loading on plain abdominal radiographs in children. Pediatr Radiol. 1999. 29:255–258.
7. van den Bosch M, Graafmans D, Nievelstein R, Beek E. Systematic assessment of constipation on plain abdominal radiographs in children. Pediatr Radiol. 2006. 36:224–226.
8. Kim HJ, Lee JG. The effect of distension of distal colon and rectum on micturition reflex in rats. Korean J Urol. 2001. 42:1004–1007.
9. Biggs WS, Dery WH. Evaluation and treatment of constipation in infants and children. Am Fam Physician. 2006. 73:469–477.
10. Dohil R, Roberts E, Jones KV, Jenkins HR. Constipation and reversible urinary tract abnormalities. Arch Dis Child. 1994. 70:56–57.
11. Loening-Baucke V. Prevalence rates for constipation and faecal and urinary incontinence. Arch Dis Child. 2007. 92:486–489.
12. Loening-Baucke V. Chronic constipation in children. Gastroenterology. 1993. 105:1557–1564.
13. Voskuijl WP, Heijmans J, Heijmans HS, Taminiau JA, Benninga MA. Use of Rome II criteria in childhood defecation disorders: applicability in clinical and research practice. J Pediatr. 2004. 145:213–217.
14. Constipation Guideline Committee of the North American Society for Pediatric Gastroenterology, Hepatology and Nutrition. Evaluation and treatment of constipation in infants and children: recommendations of the North American Society for Pediatric Gastroenterology, Hepatology and Nutrition. J Pediatr Gastroenterol Nutr. 2006. 43:e1–e13.
15. Singh SJ, Gibbons NJ, Vincent MV, Sithole J, Nwokoma NJ, Alagarswami KV. Use of pelvic ultrasound in the diagnosis of megarectum in children with constipation. J Pediatr Surg. 2005. 40:1941–1944.
16. Bijos A, Czerwionka-Szaflarska M, Mazur A, Romanczuk W. The usefulness of ultrasound examination of the bowel as a method of assessment of functional chronic constipation in children. Pediatr Radiol. 2007. 37:1247–1252.
17. Klijn AJ, Asselman M, Vijverberg MA, Dik P, de Jong TP. The diameter of the rectum on ultrasonography as a diagnostic tool for constipation in children with dysfunctional voiding. J Urol. 2004. 172:1986–1988.
18. O'Regan S, Yazbeck S, Hamberger B, Schick E. Constipation a commonly unrecognized cause of enuresis. Am J Dis Child. 1986. 140:260–261.
19. Akyol I, Adayener C, Senkul T, Baykal K, Iseri C. An important issue in the management of elimination dysfunction in children: parental awareness of constipation. Clin Pediatr (Phila). 2007. 46:601–603.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download