Abstract
Purpose
To compare the variable inflammatory parameters of acute pyelonephritis patients treated with inpatient therapy at 13 hospitals, according to the age and gender distributions.
Materials and Methods
A total of 3,544 medical records of patients with confirmed acute pyelonephritis, and admitted to hospital between January 2000 and December 2005, were retrospectively analyzed.
Results
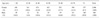
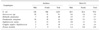
The mean age of the patients was 43.2±16.2 years old, with a male:female ratio of 1 : 5.1. The average duration of hospital admission was 7.9±5.3 days. Underlying diseases were found in 23.0% (749/3,252 patient), largely due to diabetes (35.1%). Radiological abnormal findings were found in 13.7%. The leukocyte count, ratio of segmented form, erythrocyte sedimentation rate (ESR), c-reactive protein, pyuria, positive blood culture, positive urine culture were 11,014±5,778/mm3, 74.8± 14.5%, 44.0±32.0 mm/hr, 12.4±9.3mg/dl, 83.9%, 10.5% and 46.7%, respectively. E. coli grow in 79% of the urine culture positive patients. In a comparison of 3 age groups (<40 years, 40-60 years, >61 years), the elderly patients had a greater number of underlying diseases and more pathogens in cultured blood. When divided into males and females, the elderly male patients had more pathogen in cultured urine, but contrary to the male patients, the elderly female patients had elevated leukocyte count and erythrocyte sedimentation rate. Also, the old patient group had more resistance to ampicillin when they had E. coli as the uropathogen (p=0.021). Patients with higher ESR required longer hospital admission periods.
Figures and Tables
References
1. Foxman B, Klemstine KL, Brown PD. Acute pyelonephritis in US hospitals in 1997: hospitalization and in-hospital mortality. Ann Epidemiol. 2003. 13:144–150.
2. Ki M, Park T, Choi BY, Foxman B. The epidemiology of acute pyelonephritis in South Korea. 1997-1999. Am J Epidemiol. 2004. 160:985–993.
3. Hooton TM, Stamm WE. Diagnosis and treatment of uncomplicated urinary tract infection. Infect Dis Clin North Am. 1997. 11:551–581.
4. Lee JH, Huh JS, Kim YJ. Clinical characteristics of acute pyelonephritis in adult men. Korean J Urol. 2005. 46:295–298.
5. Do SH, Kim JH, Choi YD. Vesicoureteral reflux in the adult uncomplicated acute pyelonephritis. Korean J Urol. 2001. 42:1049–1052.
6. Lie SW, Ng KC. Retrospective analysis of inflammatory parameters in acute pyelonephritis. Scand J Urol Nephrol. 2003. 37:250–252.
7. Chung KS, Ko SS, Yoon YJ, Park YH, Son HS, Lee KY. A clinical study on acute pyelonephritis. Korean J Med. 1984. 27:597–602.
8. Son HS, Ahn JH, Lee TY, Lim CK, Kim MJ. Clinical study on 740 cases of acute pyelonephritis (1980-1989). Korean J Nephrol. 1990. 9:380–387.
9. Min HJ. Acute pyelonephritis; clinical study and consideration about inpatient therapy. Korean J Med. 1998. 55:232–244.
10. Lee JS, Rho SH, Kim SE, Nam TM, Kim JS, Kim SK, et al. A study on the clinical and microbiologic features of community acquired acute pyelonephritis for the recent 5 years in a university hospital. Korean J Nephrol. 2002. 21:905–913.
11. Song HJ, Kim SJ. A study of antimicrobial sensitivity to the causative organism of urinary tract infection. Korean J Urol. 2005. 46:68–73.
12. Ko YH, Oh JS, Cho DY, Bae JH, Koh SK. Changes of causative organisms and antimicrobial sensitivity of urinary tract infection between 1979 and 2001. Korean J Urol. 2003. 44:342–350.
13. Kim SW, Lee JY, Park WJ, Cho YH, Yoon MS. Antibiotic sensitivity to the causative organism of acute simple urinary tract infection. Korean J Urol. 2000. 41:1117–1124.
14. Ko HS, Choi DY, Han YT. A study of the changes of antibiotic sensitivity to the causative organisms of urinary tract infection for recent 5 years. Korean J Urol. 1999. 40:809–816.
15. Finkelstein R, Kassis E, Reinhertz G, Gorenstein S, Herman P. Community-acquired urinary tract infection in adults: a hospital viewpoint. J Hosp Infect. 1998. 38:193–202.




 PDF
PDF ePub
ePub Citation
Citation Print
Print







 XML Download
XML Download