Abstract
Purpose
Ileus is the most common complication following radical cystectomy. Ileus causes prolonged fasting, significant patient discomfort and prolongation of the hospital stay. We retrospectively examined the risk factors for ileus following radical cystectomy.
Materials and Methods
Between January, 2000 and June, 2007, 59 patients underwent radical cystectomy with urinary diversion at our institution. 30 patients underwent creation of an ileal conduit and 29 patients underwent orthotopic bladder substitution with using ileum. Ileus was defined as the persistent absence of flatus on postoperative day 7 or the generalized findings of ileus on simple abdominal film. The potential risk factors were analyzed between the ileus and non ileus groups, including the patient's age and gender, the American Society of Anesthesiologists score, the preoperative serum albumin level, prior abdominal surgery, the operative time, combined operation, the estimated blood loss, the type of urinary diversion, use of N2O, use of intestinal stapler, complications, the ICU stay and the pathologic stage and grade.
Results
24% (14/59) of patients had postoperative ileus. The difference of the ASA score between the two groups was statistically significant (p=0.03). Patients with ileus (67.5±7.2) were older than the non-ileus patients (63.0±9.4) (p=0.103). Ileus was more frequent in men (29.5%, 13/44) than in women (6.6%, 1/15) (p=0.09).
Figures and Tables
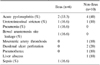
Table 2
Comparison of the patients' gender between the ileus and non-ileus groups according to the ASA score

References
1. Messing EM, Young TB, Hunt VB, Gilchrist KW, Newton MA, Bram LL, et al. Comparison of bladder cancer outcome in men undergoing hematuria home screening versus those with standard clinical presentations. Urology. 1995. 45:387–396.
2. Chang SS, Baumgartner RG, Wells N, Cookson MS, Smith JA Jr. Causes of increased hospital stay after radical cystectomy in a clinical pathway setting. J Urol. 2002. 167:208–211.
3. Hollenbeck BK, Miller DC, Taub D, Dunn RL, Khuri SF, Henderson WG, et al. Identifying risk factors for potentially avoidable complications following radical cystectomy. J Urol. 2005. 174:1231–1237.
4. Chang SS, Cookson MS, Baumgartner RG, Wells N, Smith JA Jr. Analysis of early complications after radical cystectomy: results of a collaborative care pathway. J Urol. 2002. 167:2012–2016.
5. Park HK, Lee SW, Yeo WG, Kwak C, Byeon SS, Kim HH, et al. Analysis of risk factors for ileus following radical cystectomy: is the prolonged use of a nasogastric tube necessary? Korean J Urol. 2004. 45:1215–1218.
6. Inman BA, Harel F, Tiguert R, Lacombe L, Fradet Y. Routine nasogastric tubes are not required following cystectomy with urinary diversion: a comparative analysis of 430 patients. J Urol. 2003. 170:1888–1891.
7. Donat SM, Slaton JW, Pisters LL, Swanson DA. Early nasogastric tube removal combined with metoclopramide after radical cystectomy and urinary diversion. J Urol. 1999. 162:1599–1602.
8. Person B, Wexner SD. The management of postoperative ileus. Curr Probl Surg. 2006. 43:6–65.
9. Jeon HG, Ku JH, Jeong H, Kwak C, Lee E, Lee C, et al. The impact of pelvic lymphadenectomy on the survival of patients who underwent radical cystectomy for transitional cell carcinoma of the bladder. Korean J Urol. 2004. 45:103–107.
10. Lang M, Niskanen M, Miettinen P, Alhava E, Takala J. Outcome and resource utilization in gastroenterological surgery. Br J Surg. 2001. 88:1006–1014.
11. El-Galley R, Hammontree L, Urban D, Pierce A, Sakawi Y. Anesthesia for laparoscopic donor nephrectomy: is nitrous oxide contraindicated? J Urol. 2007. 178:225–227.
12. Pruthi RS, Chun J, Richman M. Reducing time to oral diet and hospital discharge in patients undergoing radical cystectomy using a perioperative care plan. Urology. 2003. 62:661–666.
13. Shafii M, Murphy DM, Donovan MG, Hickey DP. Is mechanical bowel preparation necessary in patients undergoing cystectomy and urinary diversion? BJU Int. 2002. 89:879–881.
14. Irving AD, Scrimgeour D. Mechanical bowel preparation for colonic resection and anastomosis. Br J Surg. 1987. 74:580–581.
15. Santos JC, Batista J, Sirimarco MT, Guimaraes AS, Levy CE. Prospective randomized trial of mechanical bowel preparation in patients undergoing elective colorectal surgery. Br J Surg. 1994. 81:1673–1676.
16. Burke P, Mealy K, Gillen P, Joyce W, Traynor O, Hyland J. Requirement of bowel preparation in colorectal surgery. Br J Surg. 1994. 81:907–910.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download