Abstract
Purpose
Thrombocytosis has been reported in many types of malignancies and it has been studied as a prognostic factor. To better define the relationship between the platelet count and survival, we performed a retrospective analysis of patients with thrombocytosis and renal cell carcinoma, and some of whom had a lower survival rate than those with a normal platelet count.
Materials and Methods
We reviewed the medical records of patients with renal cell carcinoma and who had undergone radical nephrectomy between January, 1995 and December, 2004. A total of 112 patients were treated by radical nephrectomy for renal cell carcinoma. Among them, 67 patients without primary thrombocytosis, no familial history of renal cell carcinoma and no history of adjuvant therapy were enrolled in this study. The patients were divided into a normal platelet count group and a thrombocytosis group (greater than 400,000/µl) according to the perioperative platelet count. The two groups were compared pathologically and clinically, including comparing the prognosis.
Results
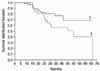
The mean follow-up was 55.8 months (range: 21 to 80). Thrombocytosis was present in 19 patients. The mean survival for the normal platelet count group was 67.8±39.36 months, compared with 41.4±30.65 months for the thrombocytosis group (p<0.05). The difference of survival between the 2 groups remained significant when controlling for the established prognostic indicators like the pathological stage, nuclear grade and cell types.
Figures and Tables
References
1. Kim SW, Park WJ, Ha JS, Lee SJ, Lee JY, Lee CB, et al. Prognostic factors in renal cell carcinoma. Korean J Urol. 2002. 43:98–105.
2. Aso Y, Homma Y. A survey on incidental adrenal tumors in Japan. J Urol. 1992. 147:1478–1481.
3. Skinner DG, Colvin RB, Vermillion CD, Pfister RC, Leadbetter WF. Diagnosis and management of renal cell carcinoma. A clinical and pathologic study of 309 cases. Cancer. 1971. 28:1165–1177.
4. Griesshammer M, Bangerter M, Sauer T, Wennauer R, Bergmann L, Heimpel H. Aetiology and clinical significance of thrombocytosis: analysis of 732 patients with an elevated platelet count. J Intern Med. 1999. 245:295–300.
5. Pedersen LM, Milman N. Prognostic significance of thrombocytosis in patients with primary lung cancer. Eur Respir J. 1996. 9:1826–1830.
6. Hernandez E, Lavine M, Dunton CJ, Gracely E, Parker J. Poor prognosis associated with thrombocytosis in patients with cervical cancer. Cancer. 1992. 69:2975–2977.
7. Van Brussel JP, Mickisch GH. Prognostic factors in renal cell and bladder cancer. BJU Int. 1999. 83:902–908.
8. Ficarra V, Righetti R, Pilloni S, D'Amico A, Maffei N, Novella G, et al. Prognostic factors in patients with renal cell carcinoma: retrospective analysis of 675 cases. Eur Urol. 2002. 41:190–198.
9. Kim WJ, Chung JI, Hong JH, Kim CS, Jung SI, Yoon DK. Epidemiological study for urologic cancer in Korea (1998-2002). Korean J Urol. 2004. 45:1081–1088.
10. Symbas NP, Townsend MF, El-Galley R, Keane TE, Graham SD, Petros JA. Poor prognosis associated with thrombocytosis in patients with renal cell carcinoma. BJU Int. 2000. 86:203–207.
11. O'Keefe SC, Marshall FF, Issa MM, Harmon MP, Petros JA. Thrombocytosis is associated with a significant increase in cancer specific death rate after radical nephrectomy. J Urol. 2002. 168:1378–1380.
12. Katsuki I, Kei K, Shunichi S, Makoto S, Hideki Y. Prognostic significance of thrombocytosis in renal cell carcinoma patients. Int J Urol. 2004. 11:364–367.
13. Oh BS, Park SH, Park YI. Significance of thrombocytosis as a prognostic factor after radical nephrectomy in patients with renal cell carcinoma. Korean J Urol. 2004. 45:1095–1099.
14. Metcalf D, Nicola NA, Gearing DP. Effects of injected leukemia inhibitory factor on hematopoietic and other tissues in mice. Blood. 1990. 76:50–56.
15. Gastl G, Plante M, Finstad CL, Wong GY, Federici MG, Bander NH, et al. High IL-6 levels in ascitic fluid correlate with reactive thrombocytosis in patients with epithelial ovarian cancer. Br J Haematol. 1993. 83:433–441.
16. Ljungberg B, Grankvist K, Rasmuson T. Serum interleukin-6 in relation to acute-phase reactants and survival in patients with renal cell carcinoma. Eur J Cancer. 1997. 33:1794–1798.
17. Takenawa J, Kaneko Y, Fukumoto M, Fukatsu A, Hirano T, Fukuyama H, et al. Enhanced expression of interleukin-6 in primary human renal cell carcinomas. J Natl Cancer Inst. 1991. 83:1668–1672.
18. Blay JY, Negrier S, Combaret V, Attali S, Goillot E, Merrouche Y, et al. Serum level of interleukin 6 as a prognosis factor in metastatic renal cell carcinoma. Cancer Res. 1992. 52:3317–3322.
19. Hollen CW, Henthorn J, Koziol JA, Burstein SA. Elevated serum interleukin-6 levels in patients with reactive thrombocytosis. Br J Haematol. 1991. 79:286–290.
20. Karpatkin S, Pearlstein E. Role of platelets in tumor cell metastases. Ann Intern Med. 1981. 95:636–641.
21. Gasic GJ, Gasic TB, Stewart CC. Antimetastatic effects associated with platelet reduction. Proc Natl Acad Sci U S A. 1968. 612:46–52.
22. Dirix LY, Verheulen PB, Hubens G. Serum basic fibroblast growth factor and vascular endothelial growth factor and tumor growth kinetics in advanced colorectal cancer. Ann Oncol. 1996. 7:843–848.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download