The differential diagnosis of macroscopic hematuria includes not only conditions such as malignancy, urolithiasis, and infections but also other rare but nevertheless important causes. These include rupture of a pseudo-aneurysm of the iliac artery into the ureter, a uretero-arterial fistula, and an aneurysm of the internal iliac artery [1-3]. We report a case of macroscopic hematuria secondary to an aneurysm of the internal iliac artery without evidence of rupture.
CASE REPORT
An 84-year-old man presented to our department with a 12-hour history of painless gross hematuria. This was his first ever episode. His past medical history included anemia, benign prostatic hyperplasia, appendicectomy, duodenal ulcer (treated surgically 40 years ago), and an abdominal aortic aneurysm. He was taking tamsulosin, finasteride, levocarnitine, and ferrous sulphate. The physical examination revealed a soft, nontender abdomen and isolated left leg edema. His blood pressure was 140/85 mmHg and his pulse was 75 beats/min. The per rectum examination revealed a smooth, slightly enlarged prostate. Laboratory investigations on admission showed the following: hemoglobin 10 g/dl, hematocrit 31.5%, platelets 162×109/l, urea 77 mg/dl, and creatinine 1.5 mg/dl. Midstream urine (MSU) sample investigations revealed the following: specific weight 1,030, pH 5.5, white cells 2-4, and red cells >200 per optic field. Culture showed mixed growth of 104-105 cfu. Bladder irrigation was instigated, and urine samples for cytological examination were also taken. Cystoscopy showed decreased expansion suggesting compression from outside the bladder. At the point of compression, increased vascularization was noted in the bladder mucosa with no evidence of active bleeding. No trace of blood was identified coming from the ureteric orifices, the bladder neck, or the prostate. There was no evidence of intra-vesicular masses or other inflammatory changes. The kidney-ureter-bladder X-ray revealed no abnormalities.
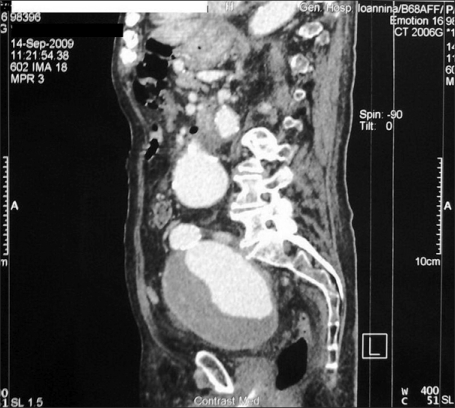
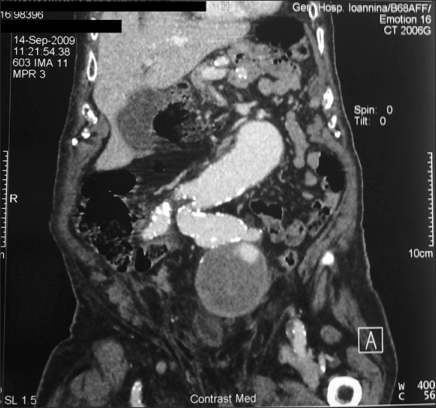
The abdominal computed tomography (CT) scan with intravenous contrast revealed left-sided hydronephrosis and dilation of the upper third of the left ureter with no evidence of stones or related peri-ureteric mass. There was an abdominal aortic aneurysm starting 3 cm below the origin of the renal vessels and involving the aortic bifurcation and both internal iliac arteries (Fig. 1, 2). The greatest diameter of the aortic aneurysm was 8.0 cm, and the left internal iliac artery's diameter was 11.5 cm (Fig. 3). The iliac artery aneurysm contained a peripheral thrombus, whereas the aortic aneurysm was partly calcified (Fig. 4). Inflammatory changes were present in the lower right peri-renal area. The right iliopsoas muscle was enlarged and of a heterogeneous texture. There was adjacent soft tissue swelling.
The cytological examination was negative for malignant cells. The hematuria was controlled by the fourth day of admission. The patient was discharged awaiting review by the vascular surgical team.
DISCUSSION
Aneurysm of the iliac artery usually coexists with aortic aneurysm and occurs more frequently in men. The diagnosis is difficult not only because of its rare occurrence but also because of its atypical presentation and the deep anatomical position of the artery in the pelvis [4]. For these reasons, an aneurysm of the iliac artery is often not considered in the differential diagnosis of macroscopic hematuria [5]. When an aneurysm of the iliac artery increases in size, symptoms appear as the result of compression or rupture into adjacent organs causing urological, gastroenterological, and neurological symptoms. The urological symptoms include hematuria, bladder outlet obstruction, and flank pain [2,5]. Direct compression by the aneurysm and the desmoplastic reaction that surrounds and fixes the bladder and the ureter can result in obstructive urological symptoms [4].
Direct rupture of an iliac aneurysm into the bladder associated with hematuria is rare, and only few cases have been reported [2,6]. It is important to note that hematuria secondary to a large aneurysm of the internal iliac artery does not necessarily suggest an arterio-vesical or arterio-ureteral fistula. The hematuria may be due to bladder mucosal bleeding as a result of congested peri-vesical vessels resulting from aneurysm compression [6]. This explains the hematuria in our patient, because no other cause of bleeding was identified by the series of investigations. The cystoscopic findings excluded a diagnosis of congenital arteriovenous malformation, because no trace of blood was found coming from the ureteric orifices.
The physical examination in this case also revealed edema of the left leg. This finding was also reported by Bhasin et al, who reported two cases of lower limb edema due to venous and lymphatic compression with subsequent cellulitis in one case and deep venous thrombosis in the other [7].
The mortality rate due to rupture of an iliac artery aneurysm is over 50%, with survival rates following treatment of over 90% [8]. Surgical intervention is indicated in patients in reasonable clinical condition and whose aneurysms are greater than 3 cm in diameter. Our patient was referred for vascular surgical review.
Two methods of treatment are currently available: open surgery and endovascular aneurysm repair (EVAR). Surgical resection and reconstruction remains the gold standard for definitive management. Other open surgical techniques include exclusion, aneurysmorrhaphy, and resection. However, surgery for aneurysms of the internal iliac artery is technically challenging because of the depth of the operative field. Aneurysm exclusion is the simplest procedure but carries a risk of long-term complications because the aneurysm is still supplied by collaterals and thus continues to expand and may even rupture. For a unilateral aneurysm of the internal iliac artery with the contralateral internal iliac artery free of disease, aneurysmorrhaphy with over-sawing of the proximal neck and distal branches offers the best result [6].
For patients unfit for open surgery, different minimally invasive techniques for the exclusion of the internal iliac artery aneurysm from the flow can be used. A combination of embolization of the distal branches of the internal iliac artery and stent-graft placement at the orifice of the internal iliac artery is usually advocated as the primary endovascular treatment option. However, this method is associated with potentially serious early and late complications. These include thrombosis of the graft, endoleaks, kinking, rupture or distal migration of the graft, or even rupture of the aneurysm due to endotension [9]. Small coil or glue embolization of the distal branches of the internal iliac artery, packing of the aneurysmal sac with wires or coils of various sizes, and percutaneous CT-guided embolization of the aneurysmal sac can also be preformed, but the long-term outcomes of these techniques have not been studied [10]. In our case, the patient was reviewed by vascular surgeons, who offered surgery, but the patient declined surgery because of his age.
An aneurysm of the internal iliac artery is a rare cause of macroscopic hematuria that can be fatal. Awareness of this as a possible cause of hematuria can assist in immediate diagnosis and appropriate treatment.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download