Abstract
Background
Insulin resistance is a key factor in the pathogenesis of polycystic ovary syndrome (PCOS), and several candidate genes involved in insulin action such as insulin receptor or insulin recpetor substrate (IRS) have been investigated. In this study, we examined the genetic effects of the IRS-1 and IRS-2 genes on the metabolic and reproductive features in women with PCOS.
Methods
125 patients with PCOS and 344 regular cycling controls were enrolled. Analysis of the polymorphisms of Gly972Arg in the IRS-1 gene and Gly1057Asp in the IRS-2 gene was performed and oral glucose tolerance tests and hyperinsulinemic euglycemic clamp tests were done.
Results
The genotype frequencies of the Gly972Arg polymorphism in the IRS-1 gene and the Gly1057Asp polymorphism in the IRS-2 gene were not significantly different between the women with PCOS and the controls. Gly972Arg polymorphism of the IRS-1 gene was extremely rare in both groups. PCOS women with the IRS-2 Asp1057Asp genotype showed significantly higher hirsutism scores, higher levels of free testosterone and higher post-load 60, 90, and 120 min plasma glucose levels compared to those women with the Gly1057Gly or Gly1057Asp genotype. In contrast, the control women with the Asp1057Asp genotype showed significantly lower post-load 60, 90, and 120 min plasma glucose levels compared with those women with the Gly1057Gly or Gly1057Asp genotype.
Conclusion
Gly972Arg polymorphism of the IRS-1 gene was extremely rare in Korean women. Gly1057Asp polymorphism of the IRS-2 gene was associated with the phenotypic features of PCOS such as hirsutism, hyperandrogenemia and hyperglycemia, but it was not associated with the insulin sensitivity index. In conclusion, Gly1057Asp polymorphism of the IRS-2 gene may not have a significant impact on insulin resistance in Korean women with PCOS.
Polycystic ovary syndrome (PCOS) is a common and heterogeneous endocrine disorder of premenopausal women characterized by menstrual irregularity, clinical or biochemical hyperandrogenism, and insulin resistance[1,2]. Familial aggregation of PCOS suggests evidence of genetic factors in the pathogenesis of this disorder, however, the exact mechanism remains unknown[3,4].
Associations of PCOS with mutations in a variety of candidate genes involved in steroid hormone biosynthesis [5,6], gonadotropic hormone action[7], insulin action or secretion[8~10], or body weight control and energy homeostasis pathway[11] have been studied. The majority of PCOS women show insulin resistance and compensatory hyperinsulinemia, which in turn aggravates hyperandrogenism. Impairment of insulin action is a key factor in the pathogenesis of PCOS and the predisposition to type 2 diabetes or metabolic syndrome. Therefore, genes involved in insulin action such as insulin genes, insulin receptor genes, insulin receptor substrate (IRS) genes have been investigated as candidate genes in the pathogenesis of PCOS.
Since IRS proteins are critical to signal transduction in insulin target tissues[12], genetic abnormalities of IRS-1 or IRS-2 may affect the susceptibility of type 2 diabetes or hyperandrogenism in premature pubarche[13,14]. There has been some controversy whether or not IRS-1 or IRS-2 polymorphism is associated with PCOS[10,15~17].
The present study was designed to evaluate the effects of the polymorphisms in the IRS-1 and IRS-2 genes on the metabolic and reproductive features in Korean women with PCOS.
One-hundred twenty-five women with PCOS and 344 age-matched healthy women with regular menstrual cycles were enrolled in this study. Diagnosis of PCOS was based on the Rotterdam PCOS consensus criteria by the European Society of Human Reproduction and Embryology (ESHRE)[18]. All medications known to affect the sex hormone metabolism or insulin action or kinetics were discontinued for at least 3 months before study enrollment. The institutional review board of Ewha Womans University Mokdong Hospital approved the study. Informed consent was obtained from all participants.
Studies were performed on the second to the 5th day of the menstrual cycle in controls and PCOS women with spontaneous menses and the arbitrary date in PCOS women with amenorrhea. Weight and height were measured in subjects wearing light clothing and without shoes; BMI was also calculated (kg/m2). Waist circumference was measured on bare skin during midrespiration at the narrowest indentation between the 10th rib and the iliac crest to the nearest 0.1 cm. The degree of hirsutism was determined by a modified Ferriman-Gallwey (FG) score[18]. Visceral and subcutaneous fat areas were measured by using a computed tomography at the level of umbilicus in PCOS women only.
A standard 75-g oral glucose tolerance test (OGTT) was performed to assess glucose metabolism status. Hyperinsulinemic euglycemic clamp tests were also performed to assess insulin sensitivity using protocol described by DeFronzo et al[19]. After a 10 min priming with insulin, constant infusion of insulin was performed at a rate of 3 µU/kg/min. During the lamp period, the plasma glucose concentration was maintained at 90 mg/dL by monitoring the glucose level at 5-min intervals. A quantitative estimate of insulin sensitivity, glucose disposal rate, insulin mediated glucose uptake (IMGU), was provided by mean glucose infusion rate (mg/kg.min) in the last 15 min of the 2 h of hyperinsulinemic euglycemic clamp study.
Plasma glucose was measured by the glucose oxidase method (Beckman Model Glucose Analyzer 2) and plasma insulin was by radioimmunoassay using a kit from Diagnostic Products Corporation (Los Angeles, CA). Plasma levels of LH, FSH, and SHBG were measured with specific immunoradiometric assays, and total testosterone with RIA using commercial kits (Diagnostic Products Co., Los Angeles, CA). Free testosterone was calculated with total testosterone, SHBG, and albumin using Kaufman's formula http://www.issam.ch/freetesto.htm
[20].
Genomic DNA was extracted from leukocytes in peripheral blood samples according to the manufacturer's instruction (QIAGEN K.K., Tokyo, Japan). A total of 200 µL of peripheral blood leukocytes were extracted from each subjects, and genomic DNA (4~8 µg) was eluted in a total volume of 200 µL.
The sequences of the primers for IRS-1 polymorphism were as follows; 5'-CTT CTG TCA GGT GTC CAT CC-3' and 5'-TGG CGA GGT GTC CAC GTA GC-3'. The PCR product was digested with BstNI (New England Biolab), which cleaves the Arg allele to generate two DNA fragments of 108- and 51-bp, respectively; otherwise 159-bp only in Gly972Gly wild type.
The sequences of the primers for IRS-2 polymorphism were as follows; 5'-TCC TTG GAC GGC CTC CTG T-3' and 5'-AAG GCC TCG ACT CCC GAC A-3'. The PCR product was digested with SmaI (New England Biolab), which cleaves the Gly allele to generate two DNA fragments of 192- and 54-bp, respectively in wild type; otherwise 246-bp in Asp1057 allele.
PCR was carried out under the following conditions: 94℃ for 2 min, followed by 30 cycles of 94℃ for 1min, 60℃ for 1 min, 72℃ for 1 min, and 72℃ for 7 min for IRS-1; and 94℃ for 2 min, followed by 30 cycles of 94℃ for 1min, 58℃ for 1 min, 72℃ for 2 min, and 72℃ for 7 min for IRS-2.
Data were analyzed using SAS version 8.0 (SAS institute, Cary, NC). Since fasting and postload insulin levels, HOMA-IR, and SHBG showed slightly skewed distributions, analyses were performed using log-transformed data. Although mean values are shown for untransformed data, all P values were based on log-transformed data. Students' t-tests in two groups and two-way analysis of variance (ANOVA) with Post Hoc multiple comparison test in three groups were used for continuous variables, including PCOS vs. controls and IRS-2 genotypes as independent variables. Repeated measures two-way ANOVA was used to considerate the between-subject or within-subject interaction effects. All P values were two-tailed, and statistical significance was defined as P < 0.05.
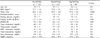
PCOS women had significantly higher levels of waist circumference (73.7 ± 11.4 vs. 67.7 ± 5.6 cm, P < 0.001), fasting plasma glucose (85 ± 8 vs. 76 ± 8 mg/dL, P < 0.001) and insulin (6.7 ± 7.9 vs. 2.5 ± 3.2 µU/mL, P < 0.001), total testosterone (56 ± 26 vs. 36 ± 14 ng/dL, P < 0.001), free testosterone (0.9 ± 0.5 vs. 0.5 ± 0.2 ng/dL, P < 0.001), LH (12.7 ± 10.1 vs. 5.3 ± 5.9 IU/L, P < 0.05), and FSH (5.4 ± 1.8 vs. 4.0 ± 1.8 IU/L, P < 0.05) compared to control women. Mean age (25 yrs old), systolic and diastolic blood pressures, and lipid profiles were not significantly different between the two groups (Table 1).
Genotype frequencies of IRS-1 and IRS-2 polymorphisms did not differ in women with PCOS and controls (Table 2). Because the frequency of IRS-1 polymorphism was extremely low in both groups (0.8 % in PCOS and 1.7% in controls), comparison of metabolic or hormonal parameters was impossible.
PCOS women with IRS-2 Asp1057Asp genotype showed significantly higher levels of FG score (4.7 ± 5.3 vs. 2.3 ± 3.1, 3.0 ± 3.2, P < 0.05) and free testosterone (1.1 ± 0.8 vs. 0.8 ± 0.5, 0.8 ± 0.4 ng/dL, P < 0.05, Table 3) compared to those with Gly1057Gly or Gly1057Asp genotypes. During 75 g OGTT, post-load 60, 90, and 120 min plasma glucose levels were significantly higher in women with Asp1057Asp genotype than those with Gly1057Gly or Gly1057Asp genotype (Fig. 1A). In contrast, post-load plasma glucose levels in control women with Asp1057Asp genotype were significantly lower than those with Gly1057Gly or Gly1057Asp genotypes (Fig. 1C). Post-load plasma insulin levels during OGTT did not differ significantly according to the genotypes of IRS-2 polymorphism in both PCOS and control women (Fig. 1B, D). Other biochemical or reproductive hormone values except waist circumference were not significantly different in control women according to IRS-2 polymorphism. Due to the small number of control subjects (n = 7) with measured LH, FSH, and visceral and subcutaneous fat areas, we could not compare these data among controls (Table 4).
In the present study, we examined the frequencies of IRS-1 Gly972Arg and IRS-2 Gly1057Asp polymorphisms and relationship of these polymorphisms to phenotypic features of PCOS in young Korean women with PCOS. Insulin sensitivity and insulin secretion capacity in Korean women with PCOS and controls were comparable to our previous report[21]. We found that the genotype frequency of IRS-1 polymorphism in PCOS women was extremely rare (0.8%) and not different compared to control women (1.7%). IRS-1 is a major protein that needs to become phosphorylated to activate the enzyme phosphatidyl-inositol 3-kinase (PI3K), a necessary step for the initiation of several effects of insulin such as glucose transport. IRS-1 gene consists of several amino acids substitutions[22]. The most common genetic variant of IRS-1 is a glycine to arginine change at codon 972, which is more prevalent among persons with insulin resistance or type 2 diabetes[23,24]. It also has been related to obesity or weight change in non-diabetic population[25,26] or hyperandrogenism in premature pubertal pubarche and adolescent girls[14]. However, many controversial studies have been reported on the relationship between this genetic variant of IRS-1 and insulin resistance status such as PCOS or type 2 diabetes in various ethnic groups. The genotype frequency of Gly972Arg was significantly higher in PCOS women than controls in Chileans[27] or European Caucasians[15], however, a Spanish study showed no difference[28] The frequency of IRS-1 Gly972Arg polymorphism was 26% in diabetic Caucasians, 11% in nondiabetic controls[29], but 3.6% and 4.5% in Japanese diabetic patients and controls, respectively[30]. Recently, Lin et al did not find Gly972Arg genotype of this polymorphism in Taiwanese women with PCOS and controls[17], suggesting that this polymorphism is rare in Asian ethnicities. Unfortunately, since this polymorphism has never been reported in the Korean population, we cannot conclude whether this rarity was unique for Koreans or just for our study population.
We observed no significant difference of the genotype frequency of Gly1057Asp of IRS-2 polymorphism in women with PCOS and controls. PCOS women with Asp1057Asp genotype showed more hirsute and hyperandrogenemic tendencies compared to those with Gly1057Asp or Gly1057Gly genotype. They also had significantly higher post-load 60, 90, and 120 min glucose levels. However, plasma insulin levels during OGTT or insulin sensitivity indices assessed by HOMA-IR, or euglycemic hyperinsulinemic clamp were not significantly different. El Mkadem et al[10] observed higher levels of post-load 2 h plasma glucose levels and HOMA-IR in PCOS women with Gly1057Asp genotype, suggesting that IRS-2 had an important role for the maintenance of normoglycemia against the insulin resistance via compensatory hyperinsulinemic response. Inactivation of IRS-2 in mice results both in peripheral insulin resistance and in reduced development or survival of beta cells in animal models[31,32]. As a consequence, failure of beta cells to compensate for the increased insulin demand leads to the development of diabetes. However, we did not find any differences in insulin resistance or changes of insulin levels during OGTT.
In contrast to our study, Ehrmann et al[15] reported significantly lower levels of 2-h glucose in nondiabetic white PCOS women with Asp1057Asp or Gly1057Asp and in nondiabetic African-American PCOS with Gly1057Asp compared to those with Gly1057Gly. However, they did not analyze the genetic effects in control subjects. Other studies also reported the risk of type 2 diabetes decreasing in relation to the dosage of the Gly allele[33,34]. The possible causes of this discrepancy might be due to the differences in criteria for definition of PCOS, ethnic variations, or different efficiencies in the detection of this mutation. Furthermore, genotype-phenotype interaction could be expressed differently and dependent on ethnicity or environment. We found opposite results in control subjects; these healthy women with Asp1057Asp had significantly lower levels of post-load glucose during OGTT (60, 90, and 120 min). This suggests that the genetic effect of Asp1057Asp on the sustained post-load hyperglycemia might be a characteristic in this study group, and possibly protective in normal cycling healthy women. To our knowledge, there has been no data observing the effect of this polymorphism in healthy reproductive aged women.
There are some limitations in this study. Firstly, the numbers of sample size was quite small, and had little power in association studies examining the effects of genetic variants on risk of PCOS. Only seven women with PCOS had a family history of PCOS or diabetes, therefore we cannot observe any impact of this polymorphism on the development of PCOS or type 2 diabetes. Secondly, we cannot reveal the exact mechanism for the difference in OGTT profile as a function of IRS-2 genotype especially as they go in different directions in the PCOS and control subjects. Finally, we cannot rule out the possibility of any other existing mutations in the insulin receptor itself, because we only had the data of single nucleotide polymorphism.
In summary, genotype frequency of Gly972Arg of IRS-1 polymorphism was extremely rare in the Korean population. Asp1057Asp genotype of IRS-2 polymorphism was related to mild hyperandrogenemia and hyperglycemia in young Korean women with PCOS, and these relationships were not consistent in healthy counterparts.
We thus conclude that the Gly1057Asp polymorphism in IRS-2 gene may not have a significant impact on the insulin resistance in Korean women with PCOS.
Figures and Tables
Fig. 1
Plasma glucose and insulin concentrations in PCOS (A and B), and controls (C and D) during 75 g oral glucose tolerance test according to IRS-2 genotypes. *P < 0.05 vs. Gly1057Gly and Gly1057Asp. †P < 0.05 vs. Gly1057Asp.

Table 1
Clinical and biochemical characteristics in PCOS in women with polycystic ovary syndrome (PCOS) and control

References
1. Carmina E, Lobo RA. Polycystic ovary syndrome (PCOS): arguably the most common endocrinopathy is associated with significant morbidity in women. J Clin Endocrinol Metab. 1999. 84:1897–1899.
2. Dunaif A, Givens JR, Haseltine FP, Merriam GR. Current issues in endocrinology and metabolism: polycystic ovary syndrome. 1992. Boston: Blackwell Scientific.
3. Escobar-Morreale HF, Luque-Ramirez M, San Millan JL. The molecular-genetic basis of functional hyperandrogemism and the polycystic ovary syndrome. Endocr Rev. 2005. 26:251–282.
4. Givens JR. Fam ilial polycystic ovarian disease. Endocrinol Metab Clin North Am. 1988. 17:771–783.
5. Gharani N, Waterworth DM, Batty S, White D, Gilling-Smith C, Conway GS, McCarthy M, Franks S, Williamson R. Association of the steroid synthesis gene CYP11a with polycystic ovary syndrome and hyperandrogenism. Hum Mol Genet. 1997. 6:397–402.
6. Carey AH, Waterworth D, Patel K, White D, Little J, Novelli P, Franks S, Williamson R. Polycystic ovaries and premature male pattern baldness are associated with one allele of the steroid metabolism gene CYP17. Hum Mol Genet. 1994. 3:1873–1876.
7. Ehrmann DA. Polycystic ovary syndrome. N Engl J Med. 2005. 352:1223–1236.
8. Eaves IA, Bennett ST, Forster P, Ferber KM, Ehrmann D, Wilson AJ, Bhattacharyya S, Ziegler AG, Brinkmann B, Todd JA. Transmission ratio distortion at the INS-IGF2 VNTR. Nat Genet. 1999. 22:324–325.
9. Urbanek M, Woodroffe A, Ewens KG, Diamanti-Kandarakis E, Legro RS, Strauss JF 3rd, Dunaif A, Spielman RS. Candidate gene region for polycystic ovary syndrome on chromosome 19p13.2. J Clin Endocrinol Metab. 2005. 90:6623–6629.
10. El Mkadem SA, Lautier C, Macari F, Molinari N, Lèfebvre P, Renard E, Gris JC, Cros G, Daurès JP, Bringer J, White MF, Grigorescu F. Role of allelic variant Gly972 Arg of IRS-1 and Gly1057Asp of IRS-2 in moderate-to-severe insulin resistance of women with polycystic ovary syndrome. Diabetes. 2001. 50:2164–2168.
11. Kiddy DS, Hamilton-Fairley D, Bush A, Short F, Anyaoku V, Reed MJ, Franks S. Improvement in endocrine and ovarian function during dietary treatment of obese women with polycystic ovary syndrome. Clin Endocrinol (Oxf). 1992. 36:105–111.
12. Sesti G, Federici M, Hribal ML, Lauro D, Sbraccia P, Lauro R. Defects of the insulin receptor substrate (IRS) system in human metabolic disorders. FASEB J. 2001. 15:2099–2111.
13. Burks DJ, White MF. IRS proteins and β-cell function. Diabetes. 2001. 50:S140–S145.
14. Witchel SF, Smith R, Tomboc M, Aston CE. Candidate gene analysis in premature pubarche and adolescent hyperandrogenism. Fertil Steril. 2001. 75:724–730.
15. Ehrmann DA, Tang X, Yoshiuchi I, Cox NJ, Bell GI. Relationship of insulin receptor substrate-1 and -2 genotypes to phenotypic features of polycystic ovary syndrome. J Clin Endocrinol Metab. 2002. 87:4297–4300.
16. Baba T, Endo T, Sata F, Honnma H, Kitajima Y, Hayashi T, Manase K, Kanaya M, Yamada H, Minakami H, Kishi R, Saito T. Polycystic ovary syndrome is associated with genetic polymorphism in the insulin signaling gene IRS-1 but not ENPP1 in a Japanese population. Life Sci. 2007. 81:850–854.
17. Lin TC, Yen JM, Gong KB, Kuo TC, Ku DC, Liang SF, Wu MJ. Abnormal glucose tolerance and insulin resistance in polycystic ovary syndrome amongst the Taiwanese population- not correlated with insulin receptor substrate-1 Gly972Arg/Ala513Pro polymorphism. BMC Med Genet. 2006. 7:36–43.
18. Zawadzki JK, Dunaif A. Dunaif A, Givens JR, Haseltine FP, Merriam GR, editors. Diagnostic criteria for polycystic ovary syndrome: towards a more rational approach. Polycystic ovary syndrome. 1992. Boston: Blackwell Scientific Publications;377–384.
19. DeFronzo RA, Tobin JD, Andres R. Glucose clamp technique: a method for quantifying insulin secretion and resistance. Am J Physiol. 1979. 237:E214–E223.
20. Vermeulen A, Verdonck L, Kaufman JM. A critical evaluation of simple methods for the estimation of free testosterone in serum. J Clin Endocrinol Metab. 1999. 84:3666–3672.
21. Park HR, Oh JY, Hong YS, Sung Y-A, Lee H, Cheong HW. The clinical characteristics of Korean women with polycystic ovary syndrome. Kor J Med. 2007. 73:169–175.
22. Ura S, Araki E, Kishikawa H, Shirotani T, Todaka M, Isami S, Shimoda S, Yoshimura R, Matsuda K, Motoyoshi S, Miyamura N, Kahn CR, Shichiri M. Molecular scanning of the insulin receptor substrate-1 (IRS-1) gene in Japanese patients with NIDDM: identification of five novel polymorphisms. Diabetologia. 1996. 39:600–608.
23. Clausen JO, Hansen T, Bjorbaek C, Echwald SM, Urhammer SA, Rasmussen SB, Andersen CB, Hansen L, Almind K, Winther K, Pedersen O, Clausen JO, Borch-Johnsen K, Winther K, Haraldsdottir J. Insulin resistance: interactions between obesity and a common variant of insulin receptor substrate-1. Lancet. 1995. 346:397–402.
24. Jellema A, Zeegers MP, Feskens EJ, Dagnelie PC, Mensink RP. Gly972Arg variant in the insulin receptor substrate-1 gene and association with Type 2 diabetes: a meta-analysis of 27 studies. Diabetologia. 2003. 46:990–995.
25. Baroni MG, Arca M, Sentinelli F, Buzzetti R, Capici F, Lovari S, Vitale M, Romeo S, Di Mario U. The G972R variant of the insulin receptor substrate-1 (IRS-1) gene, body fat distribution and insulin-resistance. Diabetologia. 2001. 44:367–372.
26. Laukkanen O, Pihlajamäki J, Lindström J, Eriksson J, Valle TT, Hämäläinen H, Ilanne-Parikka P, Keinänen-Kiukaanniemi S, Tuomilehto J, Uusitupa M, Laakso M. Finnish Diabetes Prevention Study Group. Common polymorphisms in the genes regulating the early insulin signalling pathway: effects on weight change and the conversion from impaired glucose tolerance to Type 2 diabetes. The Finnish Diabetes Prevention Study. Diabetologia. 2004. 47:871–877.
27. Sir-Petermann T, Perez-Bravo F, Angel B, Maliqueo M, Calvillan M, Palomino A. G972R polymorphism of IRS-1 in women with polycystic ovary syndrome. Diabetologia. 2001. 44:1200–1201.
28. Villuendas G, Botella-Carretero JI, Roldan B, Sancho J, Escobar-Morreale HF, San Millan JL. Polymorphisms in the insulin receptor substrate-1 (IRS-1) gene and the insulin receptor substrate-2 (IRS-2) gene influence glucose homeostasis and body mass index in women with polycystic ovary syndrome and non-hyperandrogenic controls. Hum Reprod. 2005. 20:3184–3191.
29. Zhang Y, Wat N, Stratton IM, Warren-Perry MG, Orho M, Groop L, Turner RC. UKPDS 19:heterogeneity in NIDDM: separate contributions of IRS-1 and beta 3-adrenergic-receptor mutations to insulin resistance and obesity respectively with no evidence for glycogen synthase gene mutations. UK Prospective Diabetes Study. Diabetologia. 1996. 39:1505–1511.
30. Shimokawa K, Kadowaki H, Sakura H, Otabe S, Hagura R, Kosaka K, Yazaki Y, Akanuma Y, Kadowaki T. Molecular scanning of the glycogen synthase and insulin receptor substrate-1 genes in Japanese subjects with non-insulin-dependent diabetes mellitus. Biochem Biophys Res Commun. 1994. 202:463–469.
31. Withers DJ, Gutierrez JS, Towery H, Burks DJ, Ren JM, Previs S, Zhang Y, Bernal D, Pons S, Shulman GI, Bonner-Weir S, White MF. Disruption of IRS-2 causes type 2 diabetes in mice. Nature. 1998. 391:900–904.
32. Withers DJ, Burks DJ, Towery HH, Altamuro SL, Flint CL, White MF. Irs-2 coordinates Igf-1 receptor-mediated β-cell development and peripheral insulin signalling. Nat Genet. 1999. 23:32–40.
33. Mammarella S, Ramano F, Di Valerio A, Creati B, Esposio DL, Palmirotta R, Capani F, Vitullo P, Volpe G, Battista P, Della Loggia F, Mariani-Costantini R, Cam A. Interaction between the G1057D variant of IRS-2 and overweight in the pathogenesis of type 2 diabetes. Hum Mol Genet. 2000. 9:2517–2521.
34. Almind K, Frederiksen SK, Bernal D, Hansen T, Ambye L, Urhammer S, Ekstrom CT, Berglund L, Reneland R, Lithell H, White MF, Van Obberghen E, Pedersen O. Search for variants of the gene-promoter and the potential phosphotyrosine encoding sequence of the insulin receptor substrate-2 gene: evaluation of their relation with alterations in insulin secretion and insulin sensitivity. Diabetologia. 1999. 42:1244–1249.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download