Abstract
Purpose
This study aimed to examine the effects of cognitive behavior therapy for insomnia (CBT-I) based on the mobile social networking service (SNS) on dysfunctional beliefs and attitudes about sleep, sleep quality, daytime sleepiness, depression, and quality of life among rotating-shift nurses in a hospital in Korea.
Methods
A nonequivalent control group pre-post test design was used. The participants included 55 nurses with rotating three-shift work (25 in the experimental group and 30 in the control group). For the experimental group, CBT-I using mobile SNS was provided once a week for 60 minutes over six weeks. Data were analyzed using descriptive statistics, χ2-test, independent samples t-test, and Mann-whitney U test with the SPSS 21.0 program.
Results
In the homogeneity test of the general characteristics and study variables, there were no significant differences between the two groups. Nurses in the experimental group had significantly lower scores on dysfunctional beliefs and attitudes regarding sleep and sleepiness than nurses in the control group. Nurses in the experimental group had significantly higher scores on sleep quality and quality of life than nurses in the control group.
Conclusion
These findings indicate that using the mobile SNS-based CBT-I is feasible and has significant and positive treatment-related effects on rotating-shift nurses' irrational thoughts and beliefs in association with sleep, sleep quality, daytime sleepiness, and quality of life. These contribute to expanding our knowledge of rotating-shift nurses' sleep issues and their preferences for intervention.
Figures and Tables
Table 1
CBT-I Intervention Program

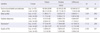
Table 2
Homogeneity Test of General, Health-related Characteristics between the Two Groups (N=55)

Table 3
Homogeneity Test for Outcome Variables between the Two Groups (N=55)
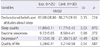
Table 4
Comparison of Outcome Variables between the Two Groups (N=55)
Notes
This manuscript is a condensed form of the first author's master's thesis from Ewha Womans University.
References
1. Suh S, Yang HC, Fairholme CP, Kim H, Manber R, Shin C. Who is at risk for having persistent insomnia symptoms? A longitudinal study in the general population in Korea. Sleep Med. 2014; 15(2):180–186. DOI: 10.1016/j.sleep.2013.09.024.
2. Ministry of Health and Welfare. Sleep disorder [Internet]. Seoul: National Health Insurance Service;Ministry of Health and Welfare;c2013. cited 2016 Aug 19. Available from: http://www.mohw.go.kr/front_new/al/sal0301vw.jsp?PAR_MENU_ID=04&MENU_ID=0403&CONT_SEQ=289376.
3. Halter MJ. Sleep-wake disorders. In : Halter MJ, Varcarolis EM, editors. Varcarolis' foundations of psychiatric mental health nursing: a clinical approach. 7th ed. St. Louis, Missouri: Elsevier Health Sciences;2014. p. 364–379.
4. Choi HY, Lim WJ. Current clinical practice of insomnia. Ewha Med J. 2013; 36(2):84–92. DOI: 10.12771/emj.2013.36.2.84.
5. Morin CM, Hauri PJ, Espie CA, Spielman AJ, Buysse DJ, Bootzin RR. Nonpharmacologic treatment of chronic insomnia. An American Academy of Sleep Medicine review. Sleep. 1999; 22(8):1134–1156.
6. Arnedt JT, Cuddihy L, Swanson LM, Pickett S, Aikens J, Chervin RD. Randomized controlled trial of telephone-delivered cognitive behavioral therapy for chronic insomnia. Sleep. 2013; 36(3):353–362. DOI: 10.5665/sleep.2448.
7. Johnson JA, Rash JA, Campbell TS, Savard J, Gehrman PR, Perlis M, et al. A systematic review and meta-analysis of randomized controlled trials of cognitive behavior therapy for insomnia (CBT-I) in cancer survivors. Sleep Med Rev. 2016; 27:20–28. DOI: 10.1016/j.smrv.2015.07.001.
8. Richter K, Acker J, Adam S, Niklewski G. Prevention of fatigue and insomnia in shift workers-a review of non-pharmacological measures. EPMA J. 2016; 7:16. DOI: 10.1186/s13167-016-0064-4.
9. Järnefelt H, Lagerstedt R, Kajaste S, Sallinen M, Savolainen A, Hublin C. Cognitive behavioral therapy for shift workers with chronic insomnia. Sleep Med. 2012; 13(10):1238–1246. DOI: 10.1016/j.sleep.2012.10.003.
10. Lee JT, Lee KJ, Park JB, Lee KW, Jang KY. The relations between shiftwork and sleep disturbance in a university hospital nurses. Korean J Occup Environ Med. 2007; 19(3):223–230.
11. Im SB, Yu SY, Seo EB, Lee SJ, Yun BR, Seo EJ, et al. The effects of shift work on the nurses' negative affectivity and sleep disorder. J Korean Acad Psychiatr Ment Health Nurs. 2006; 15(1):40–47.
12. Kim MS, Kim JR, Park KS, Kang YS, Choe MS. Associations between sleep quality, daytime sleepiness, with perceived errors during nursing work among hospital nurses. J Agric Med Community Health. 2013; 38(4):229–242. DOI: 10.5393/JAMCH.2013.38.4.229.
13. van Straten A, Emmelkamp J, de Wit J, Lancee J, Andersson G, van Someren EJ, et al. Guided internet-delivered cognitive behavioural treatment for insomnia: a randomized trial. Psychol Med. 2014; 44(7):1521–1532. DOI: 10.1017/S0033291713002249.
14. Espie CA, Kyle SD, Williams C, Ong JC, Douglas NJ, Hames P, et al. A randomized, placebo-controlled trial of online cognitive behavioral therapy for chronic insomnia disorder delivered via an automated media-rich web application. Sleep. 2012; 35(6):769–781. DOI: 10.5665/sleep.1872.
15. Espie CA, MacMahon KM, Kelly HL, Broomfield NM, Douglas NJ, Engleman HM, et al. Randomized clinical effectiveness trial of nurse-administered small-group cognitive behavior therapy for persistent insomnia in general practice. Sleep. 2007; 30(5):574–584. DOI: 10.1093/sleep/30.5.574.
16. Brown JS, Sellwood K, Beecham JK, Slade M, Andiappan M, Landau S, et al. Outcome, costs and patient engagement for group and individual CBT for depression: a naturalistic clinical study. Behav Cogn Psychother. 2011; 39(3):355–358. DOI: 10.1017/S135246581000072X.
17. Morin CM, Stone J, Trinkle D, Mercer J, Remsberg S. Dysfunctional beliefs and attitudes about sleep among older adults with and without insomnia complaints. Psychol Aging. 1993; 8(3):463–467. DOI: 10.1037/0882-7974.8.3.463.
18. Yu ES, Ko YG, Sung GH, Kwon JH. Validation of the Korean version of dysfunctional beliefs and attitudes about sleep (K-DBAS-16). Korean J Clin Psychol. 2009; 28(1):309–320.
19. Buysse DJ, Reynolds CF 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989; 28(2):193–213. DOI: 10.1016/0165-1781(89)90047-4.
20. Sohn SI, Kim DH, Lee MY, Cho YW. The reliability and validity of the Korean version of the Pittsburgh Sleep Quality Index. Sleep Breath. 2012; 16(3):803–812. DOI: 10.1007/s11325-011-0579-9.
21. Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. 1991; 14(6):540–545. DOI: 10.1093/sleep/14.6.540.
22. Cho YW, Lee JH, Son HK, Lee SH, Shin C, Johns MW. The reliability and validity of the Korean version of the Epworth sleepiness scale. Sleep Breath. 2011; 15(3):377–384. DOI: 10.1007/s11325-010-0343-6.
23. Radloff LS. The CES-D scale. A self-report depression scale for research in the general population. Appl Psychol Meas. 1977; 1(3):385–401. DOI: 10.1177/014662167700100306.
24. Chon KK, Rhee MK. Preliminary development of Korean version of CES-D. Korean J Clin Psychol. 1992; 11(1):65–76.
25. The WHOQOL group. Development of the World Health Organization WHOQOL-BREF quality of life assessment. Psychol Med. 1998; 28(3):551–558. DOI: 10.1017/S0033291798006667.
26. Min SK, Lee CI, Kim KI, Suh SY, Kim DK. Development of Korean version of WHO Quality of Life Scale Abbreviated Version (WHOQOL-BREF). J Korean Neuropsychiatr Assoc. 2000; 39(3):571–579.
27. Perlis ML, Jungquist C, Smith MT, Posner D.
JH Kim
SY Seo
CH Yoon
. Cognitive behavioral treatment of insomnia: a session-by-session guide. 1st Engl. Ed. Seoul: Koonja;c2013. p. 185.
28. Lancee J, Eisma MC, van Straten A, Kamphuis JH. Sleeprelated safety behaviors and dysfunctional beliefs mediate the efficacy of online CBT for insomnia: a randomized controlled trial. Cogn Behav Ther. 2015; 44(5):406–422. DOI: 10.1080/16506073.2015.1026386.
29. Lee JJ, Shin HC. Effects of cognitive-behavioral therapy of insomnia on Korean college students. Korean J Couns. 2011; 12(2):693–707.
30. Shimodera S, Watanabe N, Furukawa TA, Katsuki F, Fujita H, Sasaki M, et al. Change in quality of life after brief behavioral therapy for insomnia in concurrent depression: analysis of the effects of a randomized controlled trial. J Clin Sleep Med. 2014; 10(4):433–439. DOI: 10.5664/jcsm.3624.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download