Abstract
Purpose
The aims of this study were to construct a hypothetical structural model which explains premenstrual coping in university students and to test the fitness with collected data.
Methods
Participants were 206 unmarried women university students from 3 universities in A and B cities. Data were collected from March 29 until April 30, 2016 using self-report structured questionnaires and were analyzed using IBM SPSS 23.0 and AMOS 18.0.
Results
Physiological factor was identified as a significant predictor of premenstrual syndrome (t=6.45, p<.001). This model explained 22.1% of the variance in premenstrual syndrome. Psychological factors (t=-2.49, p=.013) and premenstrual syndrome (t=8.17, p<.001) were identified as significant predictors of premenstrual coping. Also this model explained 30.9% of the variance in premenstrual coping in university students. A physiological factors directly influenced premenstrual syndrome (β=.41, p=.012). Premenstrual syndrome (β=.55, p=.005) and physiological factor (β=.23, p=.015) had significant total effects on premenstrual coping. Physiological factor did not have a direct influence on premenstrual coping, but indirectly affected it (β=.22, p=.007). Psychological factors did not have an indirect or total effect on premenstrual coping, but directly affected it (β=-.17, p=.036).
Conclusion
These findings suggest that strategies to control physiological factors such as menstrual pain should be helpful to improve premenstrual syndrome symptoms. When developing a program to improve premenstrual coping ability and quality of menstrual related health, it is important to consider psychological factors including perceived stress and menstrual attitude and premenstrual syndrome.
Figures and Tables
Table 1
Descriptive Statistics of Observed Variables and Correlations among the Observed Variables (N=206)
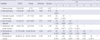
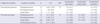
Table 2
Model Fit Indices for the Hypothetical Model (N=206)

Table 3
Standardized Direct, Indirect, and Total Effects of the Hypothetical Model (N=206)
References
1. Indusekhar R, Usman SB, O'Brien S. Psychological aspects of premenstrual syndrome. Best Pract Res Clin Obstet Gynaecol. 2007; 21(2):207–220. DOI: 10.1016/j.bpobgyn.2006.10.002.
2. National Health Insurance Service. Once a month, exhausting an intruder on a woman: Premenstrual syndrome (PMS). Health Insur. 2015; 201(7):22–23.
3. Kim BM, Jung JI, Song YM, Lee JK, Yoo JH. Association of premenstrual syndrome with quality of life in young Korean women. J Korean Acad Fam Med. 2008; 29(2):108–113.
4. Halbreich U, Borenstein J, Pearlstein T, Kahn LS. The prevalence, impairment, impact, and burden of premenstrual dysphoric disorder (PMS/PMDD). Psychoneuroendocrinology. 2003; 28:Suppl 3. 1–23. DOI: 10.1016/S0306-4530(03)00098-2.
5. Winer SA, Rapkin AJ. Premenstrual disorders: Prevalence, etiology and impact. J Reprod Med. 2006; 51:4 Suppl. 339–347.
6. Shin MA. A structural model of premenstrual symptom in female college students [dissertation]. Seoul: Hanyang University;2005. 1–95.
7. Ahn S, Lee SO. A study on premenstrual discomfort and related factors in female college students. J Korean Data Anal Soc. 2006; 8(6):2221–2235.
8. Jung GS, Oh HM, Choi IR. The influential factors on premenstrual syndrome college female students. J Korea Acad Ind Coop Soc. 2014; 15(5):3025–3036. DOI: 10.5762/KAIS.2014.15.5.3025.
9. Park KE, Lee SE. A study on premenstrual syndrome and menstrual attitude. Korean J Women Health Nurs. 2001; 7(3):359–372.
10. Kim MJ, Nam YS, Oh KS, Lee CM. Some important factors associated with premenstrual syndrome influence of excercise, menarche, and age on PMS. J Phys Growth Motor Dev. 2003; 11(2):13–26.
11. Ekin GU, Ekin M, Savan K. Prevalence of premenstrual symptoms among college students. Turkiye Klinikleri J Med Sci. 2013; 33(2):301–305. DOI: 10.5336/medsci.2011-25764.
12. Hong KJ, Park YS, Kim JE, Kim HW. Transcultural differences on perimenstrual discomforts, menstrual attitudes and sex role acceptance between Korean and American college students. J Korean Acad Nurs. 1998; 28(2):233–243.
13. Jeon JH, Hwang SK. A structural equation modeling on premenstrual syndrome in adolescent girls. J Korean Acad Nurs. 2014; 44(6):660–671. DOI: 10.4040/jkan.2014.44.6.660.
14. Read JR, Perz J, Ussher JM. Ways of coping with premenstrual change: Development and validation of a premenstrual coping measure. BMC Womens Health. 2014; 14:1. DOI: 10.1186/1472-6874-14-1.
15. Kim YI, Lee EH, Jeon GE, Choi SJ. A study on coping styles for dysmenorrhea and affecting factors in middle school students. J Korean Acad Community Health Nurs. 2013; 24(3):264–272. DOI: 10.12799/jkachn.2013.24.3.264.
16. Engel GL. The clinical application of the biopsychosocial model. Am J Psychiatry. 1980; 137(5):535–544. DOI: 10.1176/ajp.137.5.535.
17. Yamamoto K, Okazaki A, Sakamoto Y, Funatsu M. The relationship between premenstrual symptoms, menstrual pain, irregular menstrual cycles, and psychosocial stress among Japanese college students. J Physiol Anthropol. 2009; 28(3):129–136. DOI: 10.2114/jpa2.28.129.
18. Hamaideh SH, Al-Ashram SA, Al-Modallal H. Premenstrual syndrome and premenstrual dysphoric disorder among Jordanian women. J Psychiatr Ment Health Nurs. 2014; 21(1):60–68. DOI: 10.1111/jpm.12047.
19. Lee Y, Im EO. A path analysis of stress and premenstrual symptoms in Korean international and Korean domestic students. J Adv Nurs. 2016; 72(12):3045–3059. DOI: 10.1111/jan.13061.
20. Kline RB. Principles and practice of structural equation modeling. 2nd ed. New York, NY: Guilford Press;2005. p. 20–208.
21. Bourdel N, Alves J, Pickering G, Ramilo I, Roman H, Canis M. Systematic review of endometriosis pain assessment: How to choose a scale? Hum Reprod Update. 2015; 21(1):136–152. DOI: 10.1093/humupd/dmu046.
22. Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983; 24(4):385–396. DOI: 10.2307/2136404.
23. Park JO, Seo YS. Validation of the perceived stress scale (PSS) on samples of Korean university students. Korean J Psychol Gen. 2010; 29(3):611–629.
24. Yang DO, Youn GH. Attitudes toward menstruation according to the increased years after menarche. Korean J Woman Psychol. 2001; 6(3):37–48.
25. Sarason IG, Sarason BR, Shearin EN, Pierce GR. A brief measure of social support: Practical and theoretical implications. J Soc Pers Relat. 1987; 4(4):497–510. DOI: 10.1177/0265407587044007.
26. Hong OK. Antecedents and health-related consequences of loneliness in older Korean immigrants [dissertation]. Omaha, NE: University of Nebraska;1996. 1–190.
27. Allen SS, McBride CM, Pirie PL. The shortened premenstrual assessment form. J Reprod Med. 1991; 36(11):769–772.
28. Lee MH, Kim JW, Lee JH, Kim DM. The standardization of the shortened premenstrual assessment form and applicability on the internet. J Korean Neuropsychiatr Assoc. 2002; 41(1):159–167.
29. Kim HO, Lim SW, Woo HY, Kim KH. Premenstrual syndrome and dysmenorrhea in Korean adolescent girls. Korean J Obstet Gynecol. 2008; 51(11):1322–1329.
30. Eissa M. Personality and psychosocial factors affecting premenstrual syndrome. Curr Psychiatr. 2010; 17(1):55–62.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download