Abstract
Purpose
This study was a systematic review and meta-analysis designed to investigate effects of psychoeducational intervention for cancer survivors.
Methods
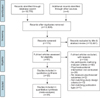
Ten databases were searched. Two reviewers independently performed the selection of the studies, data extraction and assessment. The risk of bias was assessed using Cochrane Collaboration's tool. To estimate the effect size, meta-analysis of the studies was performed using Comprehensive Meta-Analysis and RevMan programs.
Results
Of 18,781 publications identified, 35 met inclusion criteria, and 25 studies were used to estimate effect size of psychoeducational intervention. Effect sizes (standardized mean difference [SMD]) were heterogeneous and random effects models were used in the analyses. Psychoeducational intervention was effective for quality of life (n=2,410, ES=0.23; 95% CI: 0.09~0.37), coping and self-efficacy (n=179, ES=0.68; 95% CI: 0.26~1.11), anxiety (n=1,786, ES=-0.26; 95% CI: -0.37~-0.15), depression (n=1,910, ES=-0.28; 95% CI: -0.37~-0.18), and psychological distress (n=2,242, ES=-0.31; 95% CI: -0.46~-0.17). Subgroup analysis showed that counseling was the most effective intervention for quality of life, and behavioral therapy was an effective intervention for all positive and negative outcomes. Publication bias was not detected except for psychological distress.
Conclusion
Psychoeducational intervention appears to be effective in improving quality of life and coping and self-efficacy, and it is effective in reducing psychological symptoms in cancer survivors. Behavioral therapy, especially, is commonly effective in improving psychosocial outcomes. However, low-quality evidence, variability in the designs of existing studies, and publication bias suggest that additional high-quality trials should be conducted in the future.
Figures and Tables
Table 1
Descriptive Summary of Included Studies

References
1. Ministry of Health & Welfare, Korea Central Cancer Registry, National Cancer Center. Annual report of cancer statistics in Korea in 2014 [Internet]. Seoul: Ministry of Health & Welfare;2015. cited 2017 February 9. Available from: http://ncc.re.kr/cancerStatsView.ncc?bbsnum=397&searchKey=total&searchValue=&pageNum=1.
2. American Cancer Society. Cancer facts & figures 2016 [Internet]. Atlanta, GA: Author;2016. cited 2016 November 29. Available from: http://www.cancer.org/acs/groups/content/@research/documents/document/acspc-047079.pdf.
3. Cappiello M, Cunningham RS, Knobf MT, Erdos D. Breast cancer survivors: Information and support after treatment. Clin Nurs Res. 2007; 16(4):278–294. DOI: 10.1177/1054773807306553.
4. Antoni MH. Psychosocial intervention effects on adaptation, disease course and biobehavioral processes in cancer. Brain Behav Immun. 2013; 30:Suppl. S88–S98. DOI: 10.1016/j.bbi.2012.05.009.
5. Houlihan NG. Transitioning to cancer survivorship: Plans of care. Oncology (Williston Park). 2009; 23:8 Suppl. 42–48.
6. Li Q, Lin Y, Liu X, Xu Y. A systematic review on patient-reported outcomes in cancer survivors of randomised clinical trials: Direction for future research. Psychooncology. 2014; 23(7):721–730. DOI: 10.1002/pon.3504.
7. Zhang H, Zhou Y, Cui Y, Yang J. The effectiveness of a rehabilitation programme for Chinese cancer survivors: A pilot study. Int J Nurs Pract. 2016; 22(1):79–88. DOI: 10.1111/ijn.12370.
8. Hoon LS, Chi Sal CW, Hong-Gu H. Effect of psychosocial interventions on outcomes of patients with colorectal cancer: A review of the literature. Eur J Oncol Nurs. 2013; 17(6):883–891. DOI: 10.1016/j.ejon.2013.05.001.
9. Tursi MF, Baes C, Camacho FR, Tofoli SM, Juruena MF. Effectiveness of psychoeducation for depression: A systematic review. Aust N Z J Psychiatry. 2013; 47(11):1019–1031. DOI: 10.1177/0004867413491154.
10. Matsuda A, Yamaoka K, Tango T, Matsuda T, Nishimoto H. Effectiveness of psychoeducational support on quality of life in early-stage breast cancer patients: A systematic review and meta-analysis of randomized controlled trials. Qual Life Res. 2014; 23(1):21–30. DOI: 10.1007/s11136-013-0460-3.
11. Xiao W, Chow KM, So WK, Leung DY, Chan CW. The effectiveness of psychoeducational intervention on managing symptom clusters in patients with cancer: A systematic review of randomized controlled trials. Cancer Nurs. 2016; 39(4):279–291. DOI: 10.1097/ncc.0000000000000313.
12. Barsevick AM, Sweeney C, Haney E, Chung E. A systematic qualitative analysis of psychoeducational interventions for depression in patients with cancer. Oncol Nurs Forum. 2002; 29(1):73–84. DOI: 10.1188/02.onf.73-87.
13. Smedslund G, Ringdal GI. Meta-analysis of the effects of psychosocial interventions on survival time in cancer patients. J Psychosom Res. 2004; 57(2):123–131. DOI: 10.1016/s0022-3999(03)00575-0.
14. Oh PJ, Han SJ. Meta-analysis of psychosocial interventions to reduce pain in patients with cancer. J Korean Acad Nurs. 2013; 43(5):658–668. DOI: 10.4040/jkan.2013.43.5.658.
15. Mustafa M, Carson-Stevens A, Gillespie D, Edwards AG. Psychological interventions for women with metastatic breast cancer. Cochrane Database Syst Rev. 2013; (6):CD004253. DOI: 10.1002/14651858.CD004253.pub4.
16. Parahoo K, McDonough S, McCaughan E, Noyes J, Semple C, Halstead EJ, et al. Psychosocial interventions for men with prostate cancer: A Cochrane systematic review. BJU Int. 2015; 116(2):174–183. DOI: 10.1111/bju.12989.
17. Chow KM, Chan JC, Choi KK, Chan CW. A review of psychoeducational interventions to improve sexual functioning, quality of life, and psychological outcomes in gynecological cancer patients. Cancer Nurs. 2016; 39(1):20–31. DOI: 10.1097/ncc.0000000000000234.
18. McLoone J, Menzies S, Meiser B, Mann GJ, Kasparian NA. Psycho-educational interventions for melanoma survivors: A systematic review. Psychooncology. 2013; 22(7):1444–1456. DOI: 10.1002/pon.3165.
19. Macmillan Cancer Support. Two million reasons: The cancer survivorship agenda: Why we need to support people with or beyond cancer. London, UK: Author;2008.
20. Higgins JPT, Green S, editors. Cochrane handbook for systematic reviews of interventions version 5.1.0 [Internet]. London, UK: The Cochrane Collaboration;2011. cited 2016 November 29. Available from: http://handbook.cochrane.org.
21. Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. BMJ. 2009; 339:b2535. DOI: 10.1136/bmj.b2535.
22. Mullan F. Seasons of survival: Reflections of a physician with cancer. N Engl J Med. 1985; 313(4):270–273. DOI: 10.1056/nejm198507253130421.
23. Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003; 327(7414):557–560. DOI: 10.1136/bmj.327.7414.557.
24. Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997; 315(7109):629–634. DOI: 10.1136/bmj.315.7109.629.
25. Rosenthal R. Meta-analytic procedures for social research. Thousand Oaks, CA: Sage Publications;1991.
26. Schou Bredal I, Kåresen R, Smeby NA, Espe R, Sørensen EM, Amundsen M, et al. Effects of a psychoeducational versus a support group intervention in patients with early-stage breast cancer: Results of a randomized controlled trial. Cancer Nurs. 2014; 37(3):198–207. DOI: 10.1097/NCC.0b013e31829879a3.
27. Mitchell AJ, Chan M, Bhatti H, Halton M, Grassi L, Johansen C, et al. Prevalence of depression, anxiety, and adjustment disorder in oncological, haematological, and palliative-care settings: A meta-analysis of 94 interview-based studies. Lancet Oncol. 2011; 12(2):160–174. DOI: 10.1016/s1470-2045(11)70002-x.
28. Costanzo ES, Lutgendorf SK, Mattes ML, Trehan S, Robinson CB, Tewfik F, et al. Adjusting to life after treatment: Distress and quality of life following treatment for breast cancer. Br J Cancer. 2007; 97(12):1625–1631. DOI: 10.1038/sj.bjc.6604091.
29. Liu JE, Wang HY, Wang ML, Su YL, Wang PL. Posttraumatic growth and psychological distress in Chinese early-stage breast cancer survivors: A longitudinal study. Psychooncology. 2014; 23(4):437–443. DOI: 10.1002/pon.3436.
30. Park JH, Bae SH, Chun M, Jung YS, Jung YM. Factors influencing elevated distress scores at the end of primary treatment of breast cancer. Asian Oncol Nurs. 2015; 15(3):132–139. DOI: 10.5388/aon.2015.15.3.132.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download