Abstract
Purpose
This study was an experimental study to compare the inhalation effects of aroma essential oil on the quality of sleep (QOS) for shift nurses after working nights.
Methods
The participants were 60 healthy adults who didn't have any disease. As an experimental treatment, the participants in the experimental group were asked to inhale essential oil for 3 minutes at a distance of approximately 10 cm fromt heir nose and then they were asked to sleep with the aroma stone beside their head (within a 30 cm distance). QOS were measured four times on Pretest, Day 1, Day 2, and Day 3 after they slept. To measure QOS, Perceived QOS (Numeric Rating Scale), the Verran & Synder-Halpern (VSH) Sleep Scale were used, and number of awakenings (NoA) was measured by Actigraph.
Results
There were no significant differences in the homogeneity tests for general characteristics and dependent variables prior to the experiments, except for VSH of subjective sleep quality. Also, there was no significant interaction between group and time. The VSH of the experimental group was higher than the control group (F=6.39, p=.002). The NoA between the experimental group and the control group was significantly different after experimental treatment 3rd day (F=13.35, p=.001).
Figures and Tables
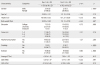
Table 2
Comparison of QOS (NRS), QOS (VSH) and NoA between Two Groups (N=60)

Exp. G=Experimental group; Cont. G=Control group; D0=Pretest day; D1=Post-test 1st day; D2=Post-test 2nd day; D3=Post-test 3rd day; QOS=Quality of Sleep; NRS=Numeric Rating Scale; VSH=Verran & Synder-Halpern sleep scale; NoA=Numbers of Awakenings; F (p)*=Repeated measures of ANCOVA (Covariates: NRS D0=5.27, VSH D0=44.2); G*t=Group*Time; T1~T14=30 min interval for 7 hours (1st day); TT1~TT14=30 min interval for 7 hours (2nd day); TTT1~TTT14=30 min interval for 7 hours (3rd day).
References
1. Im SB, Yu SY, Seo EB, Lee SJ, Yun BR, Seo EJ, et al. The effects of shift work on the nurses’ negative affectivity and sleep disorder. J Korean Acad Psychiatr Ment Health Nurs. 2006; 15(1):40–47.
2. Lee KJ, Kim MR, Lee AS, Lee JH, Chang YH, Chung MS. Development of duty form for improvement of nurses working conditions. Seoul: Hospital Nurses Association;2006.
3. Son YJ, Park YR. Relationships between sleep quality, fatigue and depression on health promoting behavior by shift-work patterns in university hospital nurses. J Korean Biol Nurs Sci. 2011; 13(3):229–237.
4. Akerstedt T, Wright KP Jr. Sleep loss and fatigue in shift work and shift work disorder. Sleep Med Clin. 2009; 4(2):257–271. DOI: 10.1016/j.jsmc.2009.03.001.
5. Shin MR. The relationship between the change in number of endothelial progenitor cells and the lack of sleep in medical students [master's thesis]. Seoul: Korea University;2013. 1–14.
6. Trendall J. Concept analysis: Chronic fatigue. J Adv Nurs. 2000; 32(5):1126–1131. DOI: 10.1046/j.1365-2648.2000.01583.x.
7. Lee HY, Kim SY. The trends of nursing research on aromatherapy in Korea. J East West Nurs Res. 2010; 16(2):85–95.
8. Nasel C, Nasel B, Samec P, Schindler E, Buchbauer G. Functional imaging of effects of fragrances on the human brain after prolonged inhalation. Chem Senses. 1994; 19(4):359–364. DOI: 10.1093/chemse/19.4.359.
9. Cho SJ. The miracle of aromatherapy. Seoul: SKbooks;2006. p. 1–236.
10. Oh HK. Aromatherapy handbook. Seoul: Yangmoon;2002. p. 1–191.
11. Oh HK. Naturopathic medicine. Seoul: Garambooks;1996. p. 1–474.
12. Choi JY, Oh HK, Chun KK, Lee JS, Park DK, Choi SD, et al. A study for antistress effects of two aromatic synergic blending oils. J Korean Soc Clin Neurophysiol. 2000; 2(2):70–80.
13. Chang SB, Chu SH, Kim YI, Yun SH. The effects of aroma inhalation on sleep and fatigue in night shift nurses. J Korean Acad Adult Nurs. 2008; 20(6):941–949.
14. Kim SJ, Gu MO. A study on the relationship among circadian types, sleep quality and adaptation to night shifts among nurses working on two or three day night duties. J Korean Clin Nurs Res. 2013; 19(3):309–320.
15. Lee HS, Hwang HS, Kim YA. Effects of hand massage with aroma oil on stress responses and serum immunity of registered nurse during the night duty. J Korean Acad Soc Nurs Educ. 2007; 13(2):169–176.
16. Buckle J. The role of aromatherapy in nursing care. Nurs Clin North Am. 2001; 36(1):57–72.
17. Battaglia S. The complete guide to aromatherapy. Queensland, AU: International Centre of Holistic Aromatherapy;2003. p. 1–602.
18. Pilcher JJ, Ginter DR, Sadowsky B. Sleep quality versus sleep quantity: Relationships between sleep and measures of health, well-being and sleepiness in college students. J Psychosom Res. 1997; 42(6):583–596. DOI: 10.1016/S0022-3999(97)00004-4.
19. Kim KS. The effect of preparatory audiovisual information with videotape influencing on sleep and anxiety of abdominal surgical patients. J Korean Acad Fundam Nurs. 1994; 1(1):19–36.
20. Lee EO, Lim NY, Park HA, Lee IS, Kim JI, Bae J, et al. Nursing research and statistics. Paju: Soomoonsa;2009. p. 1–789.
21. Lichstein KL, Stone KC, Donaldson J, Nau SD, Soeffing JP, Murray D. Actigraphy validation with insomnia. Sleep. 2006; 29(2):232–239.
22. Bae JM, Park GH. An illustrated guide to medical statistics using SPSS. Seoul: Hannarae Publishing Co.;2012. p. 1–367. .
23. Kim L. Jet lag and circadian rhythms. Sleep Med Psychophysiol. 1997; 4(1):57–65.
24. Cho MY, Min ES, Hur MH, Lee MS. Effects of aromatherapy on the anxiety, vital signs, and sleep quality of percutaneous coronary intervention patients in intensive care units. Evid Based Complement Alternat Med. 2013; 2013:381381. DOI: 10.1155/2013/381381.
25. Ju MS, Lee S, Bae I, Hur MH, Seong K, Lee MS. Effects of aroma massage on home blood pressure, ambulatory blood pressure, and sleep quality in middle-aged women with hypertension. Evid Based Complement Alternat Med. 2013; 2013:403251. http://dx.doi.org/10.1155/2013/403251.
26. Chien LW, Cheng SL, Liu CF. The effect of lavender aromatherapy on autonomic nervous system in midlife women with insomnia. Evid Based Complement Alternat Med. 2012; 2012:740813. DOI: 10.1155/2012/740813.
27. Ko YJ. Effects of lavender fragrance inhalation method on sleep, depression and stress of institutionalized elderly. J East West Nurs Res. 2012; 18(2):74–80.
28. Seo SY, Chang SY. Effects of aroma hand massage on sleep, depression and quality of life in the institutionalized elderly women. Korean J Women Health Nurs. 2009; 15(4):372–380. DOI: 10.4069/kjwhn.2009.15.4.372.
29. Lillehei AS, Halcón LL, Savik K, Reis R. Effect of inhaled lavender and sleep hygiene on self-reported sleep issues: A randomized controlled trial. J Altern Complement Med. 2015; 21(7):430–438. DOI: 10.1089/acm.2014.0327.
30. Fismer KL, Pilkington K. Lavender and sleep: A systematic review of the evidence. Eur J Integr Med. 2012; 4(4):e436–e447. DOI: 10.1016/j.eujim.2012.08.001.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download