Abstract
Purpose
This study was done to identify frequency, intensity of urinary dysfunction and daily life distress in women after a radical hysterectomy for cervical cancer.
Methods
One hundred and fifty seven women who had undergone a radical hysterectomy and one hundred and sixty five women as healthy controls completed questionnaires on intensity of urinary dysfunction and daily life distress caused by urinary dysfunction.
Results
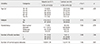
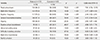
Women with cervical cancer showed higher frequency of urinary dysfunction than healthy controls. Major urinary dysfunction for women with cervical cancer in order of frequency were night-time incontinence (odds ratio=10.39, p<.001), difficulty in starting urination, weak urine stream and sense of incomplete emptying of bladder. The highest score on intensity was difficulty in starting urination, followed by urgency, weak urine stream, daytime frequency and sense of incomplete emptying. Night-time incontinence was the urinary symptom causing the most daily life distress for cervical cancer women followed by difficulty in starting urination, urgency, sense of incomplete emptying, and night-time frequency.
Figures and Tables
References
1. Ministry of Health & Welfare, Korea Central Cancer Registry, National Cancer Center. Annual report of cancer statistics in Korea in 2011. Seoul: Ministry of Health & Welfare;2013.
2. Berek JS. Berek and Novak's gynecology. 15th ed. Philadelphia, PA: Lippincott Williams and Wilkins;2011. p. 1304–1345.
3. Kashima K, Yahata T, Fujita K, Tanaka K. Analysis of the complications after radical hysterectomy for stage IB, IIA and IIB uterine cervical cancer patients. J Obstet Gynaecol Res. 2010; 36(3):555–559. DOI: 10.1111/j.1447-0756.2010.01174.x.
4. Likic IS, Kadija S, Ladjevic NG, Stefanovic A, Jeremic K, Petkovic S, et al. Analysis of urologic complications after radical hysterectomy. Am J Obstet Gynecol. 2008; 199(6):644.e1–644.e3. DOI: 10.1016/j.ajog.2008.06.034.
5. Charoenkwan K, Pranpanas S. Prevalence and characteristics of late postoperative voiding dysfunction in early-stage cervical cancer patients treated with radical hysterectomy. Asian Pac J Cancer Prev. 2007; 8(3):387–389.
6. Bergmark K, Avall-Lundqvist E, Dickman PW, Henningsohn L, Steineck G. Lymphedema and bladder-emptying difficulties after radical hysterectomy for early cervical cancer and among population controls. Int J Gynecol Cancer. 2006; 16(3):1130–1139. DOI: 10.1111/j.1525-1438.2006.00601.x.
7. Todo Y, Kuwabara M, Watari H, Ebina Y, Takeda M, Kudo M, et al. Urodynamic study on postsurgical bladder function in cervical cancer treated with systematic nerve-sparing radical hysterectomy. Int J Gynecol Cancer. 2006; 16(1):369–375. DOI: 10.1111/j.1525-1438.2006.00345.x.
8. Hwang JH. Urologic complication in laparoscopic radical hysterectomy: Meta-analysis of 20 studies. Eur J Cancer. 2012; 48(17):3177–3185. DOI: 10.1016/j.ejca.2012.06.006.
9. Chuang FC, Kuo HC. Management of lower urinary tract dysfunction after radical hysterectomy with or without radiotherapy for uterine cervical cancer. J Formos Med Assoc. 2009; 108(8):619–626. DOI: 10.1016/S0929-6646(09)60382-X.
10. Behtash N, Ghaemmaghami F, Ayatollahi H, Khaledi H, Hanjani P. A case-control study to evaluate urinary tract complications in radical hysterectomy. World J Surg Oncol. 2005; 3(1):12. DOI: 10.1186/1477-7819-3-12.
11. Manchana T, Prasartsakulchai C, Santingamkun A. Long-term lower urinary tract dysfunction after radical hysterectomy in patients with early postoperative voiding dysfunction. Int Urogynecol J. 2010; 21(1):95–101. DOI: 10.1007/s00192-009-0996-5.
12. Laterza RM, Sievert KD, de Ridder D, Vierhout ME, Haab F, Cardozo L, et al. Bladder function after radical hysterectomy for cervical cancer. Neurourol Urodyn. 2015; 34(4):309–315. DOI: 10.1002/nau.22570.
13. Song HJ. Effect of a bladder training program using internet self catheterization on voiding dysfunction of patients who have received a radical abdominal hysterectomy [master's thesis]. Seoul: Yonsei University;1999. 1–54.
14. Faul F, Erdfelder E, Buchner A, Lang AG. Statistical power analyses using G*Power 3.1: Tests for correlation and regression analyses. Behav Res Methods. 2009; 41(4):1149–1160. DOI: 10.3758/brm.41.4.1149.
15. Korean Continence Society. Textbook of female urology and urogynecology. 2nd ed. Seoul: Ilchokak;2009. p. 101–132.
16. Kim SH. The association between expectations regarding aging and health-promoting behaviors among Korean older adults. J Korean Acad Nurs. 2007; 37(6):932–940.
17. Suh DH, Cho HY, Kim K, No JH, Kim YB. Matched-case comparisons in a single institution to determine critical points for inexperienced surgeons' successful performances of laparoscopic radical hysterectomy versus abdominal radical hysterectomy in stage IA2-IIA cervical cancer. PLoS One. 2015; 10(6):e0131170. DOI: 10.1371/journal.pone.0131170.
18. Lee EJ, Kang H, Kim DH. A comparative study of laparoscopic radical hysterectomy with radical abdominal hysterectomy for early-stage cervical cancer: A long-term follow-up study. Eur J Obstet Gynecol Reprod Biol. 2011; 156(1):83–86. DOI: 10.1016/j.ejogrb.2010.12.016.
19. Park JY, Kim DY, Kim JH, Kim YM, Kim YT, Nam JH. Laparoscopic versus open radical hysterectomy for elderly patients with early-stage cervical cancer. Am J Obstet Gynecol. 2012; 207(3):195.e1–195.e8. DOI: 10.1016/j.ajog.2012.06.081.
20. Rob L, Halaska M, Robova H. Nerve-sparing and individually tailored surgery for cervical cancer. Lancet Oncol. 2010; 11(3):292–301. DOI: 10.1016/s1470-2045(09)70191-3.
21. Tseng CJ, Shen HP, Lin YH, Lee CY, Wei-Cheng Chiu W. A prospective study of nerve-sparing radical hysterectomy for uterine cervical carcinoma in Taiwan. Taiwan J Obstet Gynecol. 2012; 51(1):55–59. DOI: 10.1016/j.tjog.2012.01.011.
22. Gil-Ibáñez B, Díaz-Feijoo B, Perez-Benavente A, Puig-Puig O, Franco-Camps S, Centeno C, et al. Nerve sparing technique in robotic-assisted radical hysterectomy: Results. Int J Med Robot. 2013; 9(3):339–344. DOI: 10.1002/rcs.1480.
23. Maneschi F. Urodynamic study of bladder function following nerve sparing radical hysterectomy. J Gynecol Oncol. 2014; 25(3):159–161. DOI: 10.3802/jgo.2014.25.3.159.
24. Heo KO. A study of women's life-distress by voiding dysfunction [dissertation]. Seoul: Hanyang University;2009. 1–84.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download