Abstract
Purpose
The purpose of this study was to examine the mediation of psychological distress in the relationship between disturbance in ADL from chemotherapy induced peripheral neuropathy and quality of life in order to provide a basis for planning nursing interventions to improve the quality of life in cancer patients.
Methods
A purposive sample of 130 patients treated with chemotherapy were recruited in the cross-sectional survey design. Data were collected using self-report questionnaires. The instruments were the Chemotherapy Induced Peripheral Neuropathy Assessment Tool (CIPNAT), Hospital Anxiety Depression Scale (HADS), and Functional Assessment of Cancer Therapy-General (FACT-G).
Results
The mean score for disturbance in ADL from chemotherapy induced peripheral neuropathy was 3.30. Overall quality of life was 2.48. The mean score was 1.04 for psychological distress. The prevalence was 35.4% for anxiety and 47.7% for depression. There were significant correlations among the three variables, disturbance in ADL from chemotherapy induced peripheral neuropathy, psychosocial distress, and quality of life. Psychosocial distress had a complete mediating effect (β= -.74, p <.001) in the relationship between disturbance in ADL from chemotherapy induced peripheral neuropathy and quality of life (Sobel test: Z= -6.11, p <.001).
Figures and Tables
Figure 1
Mediating effect of psychological distress in the relationship between disturbance in ADL from chemotherapy induced peripheral neuropathy and quality of life.

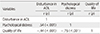
Table 1
Disturbance in ADL, Psychological Distress, and Quality of Life according to General Characteristics of the Participants (N=130)

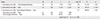
Table 2
Level of Disturbance in ADL from Chemotherapy induced Peripheral Neuropathy, Depression, Anxiety, and Quality of Life (N=130)

References
1. National Cancer Information Center. Cancer facts & figure 2014. Seoul: Ministry of Health & Welfare, National Cancer Center;2014.
2. Tofthagen CS, McMillan SC, Kip KE. Development and psychometric evaluation of the chemotherapy-induced peripheral neuropathy assessment tool. Cancer Nurs. 2011; 34(4):E10–E20. DOI: 10.1097/NCC.0b013e31820251de.
3. Tofthagen C. Patient perceptions associated with chemotherapy-induced peripheral neuropathy. Clin J Oncol Nurs. 2010; 14(3):E22–E28. DOI: 10.1188/10.CJON.E22-E28.
4. Argyriou AA, Bruna J, Marmiroli P, Cavaletti G. Chemotherapy-induced peripheral neurotoxicity (CIPN): An update. Crit Rev Oncol Hematol. 2012; 82(1):51–77. DOI: 10.1016/j.critrevonc.2011.04.012.
5. Kwak MK, Kim EJ, Lee ER, Kwon IG, Hwang MS. Characteristics and quality of life in patients with chemotherapy-induced peripheral neuropathy. J Korean Oncol Nurs. 2010; 10(2):231–239. DOI: 10.5388/jkon.2010.10.2.231.
6. Yang GS, Choe MA. Effet of anorexia and neuropathic pain induced by cisplatin on hindlimb muscles of rat. J Korean Acad Nurs. 2013; 43(3):361–369. DOI: 10.4040/jkan.2013.43.3.361.
7. Windebank AJ, Grisold W. Chemotherapy-induced neuropathy. J Peripher Nerv Syst. 2008; 13(1):27–46. DOI: 10.1111/j.1529-8027.2008.00156.x.
8. Rosson GD. Chemotherapy-induced neuropathy. Clin Podiatr Med Surg. 2006; 23(3):637–649. DOI: 10.1016/j.cpm.2006.04.009.
9. Choe MA, An GJ. Effect of nitric oxide synthase inhibitor on hindlimb muscle in rats with neuropathic pain induced by unilateral peripheral nerve injury. J Korean Acad Nurs. 2011; 41(4):520–527. DOI: 10.4040/jkan.2011.41.4.520.
10. Oh PJ, Lee YJ. Predictors of fighting spirit or helplessness/hopelessness in people with cancer. J Korean Acad Nurs. 2008; 38(2):270–277. DOI: 10.4040/jkan.2008.38.2.270.
11. Wickham R. Chemotherapy-induced peripheral neuropathy: A review and implications for oncology nursing practice. Clin J Oncol Nurs. 2007; 11(3):361–376. DOI: 10.1188/07.CJON.361-376.
12. Kim JH, Lee KM, Jeon MJ, Seol ME, Lee SH, Park JY. Symptom and interference of activities of daily living of chemotherapy-induced peripheral neuropathy in patients receiving taxanes and platinums. Asian Oncol Nurs. 2013; 13(3):145–151. DOI: 10.5388/aon.2013.13.3.145.
13. Kim HY, Kang JH, Song JE, Youn HJ. Chemotherapy-induced peripheral neuropathy and quality of life in breast cancer patients. Asian Oncol Nurs. 2013; 13(4):222–230. DOI: 10.5388/aon.2013.13.4.222.
14. Hwang WH. Assessment using CIPNAT for peripheral neuropathy in cancer patients undergoing chemotherapy[master's thesis]. Busan: Kosin University;2013. 1–57.
15. Huang TW, Lin CC. The mediating effects of depression on sleep disturbance and fatigue: Symptom clusters in patients with hepatocellular carcinoma. Cancer Nurs. 2009; 32(5):398–403. DOI: 10.1097/NCC.0b013e3181ac6248.
16. Kim JN, Lee R. A review of research on the psychosocial interventions for the cancer patients. Korean J Health Psychol. 2008; 13:329–357.
17. Lee SY, Ham YH, Ok ON, Kim EJ, Kwon IG, Hwang MS, et al. The effects of foot reflexology on peripheral neuropathy, symptom distress, anxiety and depression in cancer patients treated with oxaliplatin. Asian Oncol Nurs. 2012; 12(4):305–313. DOI: 10.5388/aon.2012.12.4.305.
18. Raingruber B. The effectiveness of psychosocial interventions with cancer patients: An integrative review of the literature (2006-2011). ISRN Nurs. 2011; 2011. DOI: 10.5402/2011/638218.
19. Shrock D, Palmer RF, Taylor B. Effects of a psychosocial intervention on survival among patients with stage I breast and prostate cancer: A matched case-control study. Altern Ther Health Med. 1999; 5(3):49–55.
20. Faul F, Erdfelder E, Lang AG, Buchner A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007; 39(2):175–191. DOI: 10.3758/BF03193146.
21. Oh SM, Min KJ, Park DB. A comparison of normal, depressed and anxious groups: A study on the standardization of the hospital anxiety and depressed scale for Koreans. J Korean Neuropsychiatr Assoc. 1999; 38(2):289–296.
22. Kim H, Yoo HJ, Kim YJ, Han OS, Lee KH, Lee JH. Development and validation of Korean functional assessment cancer therapy-general (FACT-G). Korean J Clin Psychol. 2003; 22:215–229.
23. Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986; 51(6):1173–1182.
24. Lee IH. Easy flow regression analysis. Seoul: Hannarae;2014. p. 313–316.
25. Yoo YS, Cho OK. Relationship between quality of life and nurseled bedside symptom evaluations in patients with chemotherapy-induced peripheral neuropathy. Asian Nurs Res. 2014; 8(1):36–41. DOI: 10.1016/j.anr.2013.11.002.
26. Baek YA. The correlation among symptoms, anxiety, depression and quality of life in patients with colorectal cancer undergoing chemotherapy[master's thesis]. Seoul: Seoul University;2013. 1–80.
27. Choi KS, Park JA, Lee JH. The effect of symptom experience and resilience on quality of life in patients with colorectal cancers. Asian Oncol Nurs. 2012; 12(1):61–68. DOI: 10.5388/aon.2012.12.1.61.
28. Jeong JY, So HS, Hong JE, Chae MJ, Han GH. Related factors to quality of life among hospitalized cancer patients undergoing chemotherapy. Asian Oncol Nurs. 2012; 12(1):84–91. DOI: 10.5388/aon.2012.12.1.84.
29. Tsunoda A, Nakao K, Hiratsuka K, Yasuda N, Shibusawa M, Kusano M. Anxiety, depression and quality of life in colorectal cancer patients. Int J Clin Oncol. 2006; 10(6):411–417. DOI: 10.1007/s10147-005-0524-7.
30. So WK, Marsh G, Ling WM, Leung FY, Lo JC, Yeung M, et al. The symptom cluster of fatigue, pain, anxiety, and depression and the effect on the quality of life of women receiving treatment for breast cancer: A multicenter study. Oncol Nurs Forum. 2009; 36(4):E205–E214. DOI: 10.1188/09.ONF.E205-E214.
31. Avis NE, Crawford S, Manuel J. Quality of life among younger women with breast cancer. J Clin Oncol. 2005; 23(15):3322–3330.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download