Abstract
Purpose
This study was done to develop an evidence-based incontinence care protocol through an adaptation process and to evaluate the effects of the protocol.
Methods
The protocol was developed according to the guideline of adaptation. A non-randomized controlled trial was used for testing the effects of the new Incontinence Care Protocol. A total of 120 patients having bowel incontinence with Bristol stool type 5, 6, and 7 and admitted to intensive care units were recruited to this study. The newly developed incontinence care protocol was used with patients in the experimental group and conventional skin care was given to patients in the control group. Outcome variables were incontinence-associated dermatitis (IAD) severity, pressure ulcer occurrence and severity.
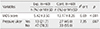
Figures and Tables
References
1. Kneedler JA, Pfister JI, Purcell SK. Incontinence associated dermatitis: An online continuing education activity [Internet]. Aurora, IL: Pfiedler Enterprises;2013. cited 2014 February 10. Available from: http://www.pfiedler.com/ce/1205/index.html.
2. Gray M. Incontinence-related skin damage: Essential knowledge. Ostomy Wound Manage. 2007; 53(12):28–32.
3. Junkin J, Selekof JL. Prevalence of incontinence and associated skin injury in the acute care inpatient. J Wound Ostomy Continence Nurs. 2007; 34(3):260–269. DOI: 10.1097/01.WON.0000270820.91694.1f.
4. Maklebust J, Magnan MA. Risk factors associated with having a pressure ulcer: A secondary data analysis. Adv Wound Care. 1994; 7(6):2527–28. 31–34.
5. Shin CW, Kim SD, Cho WY. The prevalence and management of urinary incontinence in elderly patients at sanatorium in Busan area. Korean J Urol. 2009; 50(5):450–456. DOI: 10.4111/kju.2009.50.5.450.
6. Thompson P, Langemo D, Anderson J, Hanson D, Hunter S. Skin care protocols for pressure ulcers and incontinence in long-term care: A quasi-experimental study. Adv Skin Wound Care. 2005; 18(8):422–429.
7. European Pressure Ulcer Advisory Panel. National Pressure Ulcer Advisory Panel. Prevention and treatment of pressure ulcers: Quick reference guide. Washington, DC: National Pressure Ulcer Advisory Panel;2009.
8. Armstrong DG, Ayello EA, Capitulo KL, Fowler E, Krasner DL, Levine JM, et al. New opportunities to improve pressure ulcer prevention and treatment: Implications of the CMS inpatient hospital care present on admission indicators/hospital-acquired conditions policy: A consensus paper from the international expert wound care advisory panel. Adv Skin Wound Care. 2008; 21(10):469–478. DOI: 10.1097/01.asw.0000323562.52261.40.
9. Keller BP, Wille J, van Ramshorst B, van der Werken C. Pressure ulcers in intensive care patients: A review of risks and prevention. Intensive Care Med. 2002; 28(10):1379–1388. DOI: 10.1007/s00134-002-1487-z.
10. Bliss DZ, Johnson S, Savik K, Clabots CR, Gerding DN. Fecal incontinence in hospitalized patients who are acutely ill. Nurs Res. 2000; 49(2):101–108.
11. Tariq SH. Geriatric fecal incontinence. Clin Geriatr Med. 2004; 20(3):571–587. DOI: 10.1016/j.cger.2004.04.010.
12. Shannon ML, Lehman CA. Protecting the skin of the elderly patient in the intensive care unit. Crit Care Nurs Clin North Am. 1996; 8(1):17–28.
13. Driver DS. Perineal dermatitis in critical care patients. Crit Care Nurse. 2007; 27(4):42–47.
14. Kim SY, Kim NS, Sheen SS, Ji SM, Lee SJ, Kim SH, et al. Manual for guideline adaptation [Internet]. Seoul: National Evidencebased Health Care Collaborating Agency;2011. cited 2011 March 31. Available from: http://www.cpg.or.kr/image/MANUAL.pdf.
15. Lawshe CH. A quantitative approach to content validity. Pers Psychol. 1975; 28(4):563–575. DOI: 10.1111/j.1744-6570.1975.tb01393.x.
16. Park KH, Kim KS. Effect of a structured skin care regimen on patients with fecal incontinence: A comparison cohort study. J Wound Ostomy Continence Nurs. 2014; 41(2):161–167. DOI: 10.1097/won.0000000000000005.
17. Borchert K, Bliss DZ, Savik K, Radosevich DM. The incontinence-associated dermatitis and its severity instrument: Development and validation. J Wound Ostomy Continence Nurs. 2010; 37(5):527–535. DOI: 10.1097/WON.0b013e3181edac3e.
18. Harris C, Bates-Jensen B, Parslow N, Raizman R, Singh M, Ketchen R. Bates-Jensen wound assessment tool: Pictorial guide validation project. J Wound Ostomy Continence Nurs. 2010; 37(3):253–259. DOI: 10.1097/WON.0b013e3181d73aab.
19. Bates-Jensen BM, Sussman C. Tools to measure wound healing for health professionals. In : Sussman C, Bates-Jensen BM, editors. Wound care: A collaborative practice manual. 3rd ed. Baltimore, MD: Lippincott Williams & Wilkins;2007. p. 144–179.
20. Brindle C. Outliers to the braden scale: Identifying high-risk ICU patients and the results of prophylactic dressing use. World Counc Enteros Ther J. 2010; 30(1):11–18.
21. Wound Ostomy and Continence Nurses Society. Guideline for management of pressure ulcers. WOCN clinical practice guideline series #2. Glenview, IL: Author;2010.
22. Association for the Advancement of Wound Care. Guideline of pressure ulcer guidelines [Internet]. Malvern, PA: Author;2010. cited 2011 October 1. Available from: http://aawconline.org/wp-content/uploads/2011/08/AAWCPressureUlcerGuidelineof-GuidelinesAug11.pdf.
23. Registered Nurses' Association of Ontario. Risk assessment & prevention of pressure ulcers [Internet]. Toronto, CA: Author;2005. cited 2011 March 1. Available from: http://rnao.ca/sites/rnao-ca/files/Risk_Assessment_and_Prevention_of_Pressure_Ulcers.pdf.
24. Institute for Clinical Systems Improvement. Health care protocol: Pressure ulcer prevention and treatment protocol [Internet]. Bloomington, MN: Author;2010. cited 2010 March 1. Available from: https://www.icsi.org/_asset/6t7kxy/PressureUlcer.pdf.
25. Institute for Healthcare Improvement. How-to guide: Prevent pressure ulcers [Internet]. Cambridge, MA: Author;2011. cited 2011 December 1. Available from: http://www.ihi.org/resources/Pages/Tools/HowtoGuidePreventPressureUlcers.aspx.
26. Yoo SH, Kim SS. Development and evaluation of an enteral nutrition protocol for dysphagia in patients with acute stroke. J Korean Acad Nurs. 2014; 44(3):280–293. DOI: 10.4040/jkan.2014.44.3.280.
27. Fader M, Clarke-O'Neill S, Cook D, Dean G, Brooks R, Cottenden A, et al. Management of night-time urinary incontinence in residential settings for older people: An investigation into the effects of different pad changing regimes on skin health. J Clin Nurs. 2003; 12(3):374–386.
28. Lyder CH, Clemes-Lowrance C, Davis A, Sullivan L, Zucker A. Structured skin care regimen to prevent perineal dermatitis in the elderly. J ET Nurs. 1992; 19(1):12–16.
29. Bliss DZ, Savik K, Harms S, Fan Q, Wyman JF. Prevalence and correlates of perineal dermatitis in nursing home residents. Nurs Res. 2006; 55(4):243–251. DOI: 10.1097/00006199-200607000-00004.
30. Newman DK, Preston AK, Salazar S. Moisture control, urinary and faecal incontinence, and perineal skin management. In : Krasner DL, Rodeheaver GT, Sibbald RG, editors. Chronic wound care: A clinical source book for healthcare professionals. 4th ed. Malvern, PA: HMP Communications;2007. p. 609–627.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download