Abstract
Purpose
The purpose of this study was to report the instrument modification and validation processes to make existing health belief model scales culturally appropriate for Korean Americans (KAs) regarding colorectal cancer (CRC) screening utilization.
Methods
Instrument translation, individual interviews using cognitive interviewing, and expert reviews were conducted during the instrument modification phase, and a pilot test and a cross-sectional survey were conducted during the instrument validation phase. Data analyses of the cross-sectional survey included internal consistency and construct validity using exploratory and confirmatory factor analysis.
Results
The main issues identified during the instrument modification phase were (a) cultural and linguistic translation issues and (b) newly developed items reflecting Korean cultural barriers. Cross-sectional survey analyses during the instrument validation phase revealed that all scales demonstrate good internal consistency reliability (Cronbach's alpha=.72~.88). Exploratory factor analysis showed that susceptibility and severity loaded on the same factor, which may indicate a threat variable. Items with low factor loadings in the confirmatory factor analysis may relate to (a) lack of knowledge about fecal occult blood testing and (b) multiple dimensions of the subscales.
Conclusion
Methodological, sequential processes of instrument modification and validation, including translation, individual interviews, expert reviews, pilot testing and a cross-sectional survey, were provided in this study. The findings indicate that existing instruments need to be examined for CRC screening research involving KAs.
Colorectal cancer (CRC) has been a serious problem among Korean Americans (KAs). CRC was the second most commonly diagnosed cancer for both KA men and women from 2004 to 2008 [1]. Data from Surveillance, Epidemiology, and End Results (SEER) show that CRC incidence rates increased from 54.4 to 58.2 per 100,000 for KA men and from 35.7 to 40.9 per 100,000 for KA women from the period 1998~2002 to the period 2004~2008[1].
CRC screening reduces the incidence of CRC through the early detection and removal of precancerous polyps[2]. According to the American Cancer Society, both men and women at average risk for developing CRC should be screened for CRC beginning at 50 years of age[2]. However, at 32.7%, the rate of CRC screening (defined as having one annual fecal occult blood test [FOBT], flexible sigmoidoscopy, colonoscopy, or proctoscopy in the previous five years) among KAs was the lowest among all Asian Americans and Pacific Islanders, according to merged data from the 2001, 2003, and 2005 California Health Interview Surveys[3]. The screening rates for other ethnic groups were 59.8% among Japanese, 50.7% among Chinese, 46.6% among Vietnamese, 42.3% among South Asians, 42.2% among Pacific Islanders, and 41.7% among Filipinos[3]. Furthermore, CRC screening utilization among KAs has decreased from 2001 to 2005 according to the California Health Interview Survey. KAs who reported having had an FOBT within one year of the survey declined from 14% in 2001 to 7% in 2003, and to 2% in 2005[4]. KAs who reported having had a endoscopy within five years preceding the survey changed from 30% in 2001 to 31% in 2003, and to 28% in 2005[4].
Previous studies have indicated that racial/ethnic differences in cancer screening might be due to culture-specific health beliefs or differing knowledge about and attitudes toward CRC screening among various groups[3,5]. Although beliefs may be correlates of CRC screening behaviors, and Korean culture-specific beliefs (e.g., crisis orientation or fatalism) in particular may explain low CRC screening rates in the KA population, only a few studies have examined beliefs and CRC screening behavior among KAs[5,6]. Previous research revealed that studies on CRC screening among KAs[5,6] adopted beliefs scales developed in the U.S. for the general population and lacked culturally appropriate, reliable, and validated instruments regarding CRC screening. Scales that were developed in and for Western cultures may not include constructs particular to Korean culture, as cultural influences on constructs could differ by racial and ethnic group[7]. When existing instruments are suspected to have different constructs or item contents to be used for a targeted sample, development of new scales is suggested. However, if constructs or item contents overlap but are slightly different, scale adaptation and modification are appropriate[8]. Existing studies of breast, cervical, and CRC screening have shown that health belief constructs (e.g., barriers) overlap somewhat for whites, African Americans, and KAs[6,9]. Accordingly, this study utilized scale adaptation and modification to make belief scales culturally appropriate.
The purpose of this study was to report instrument modification and validation processes to make existing health belief model (HBM) scales[10] culturally appropriate for KAs regarding health beliefs about CRC screening utilization. Among the many available options for CRC screening, FOBT was chosen for this study as the screening option because it is a basic, non-invasive, and cost-effective test[2] and it could be influenced by culture-specific health beliefs and attitudes about CRC screening[3,5].
Several sequential, methodological steps (translation, individual interviews using cognitive interviewing, expert reviews, a pilot test, and a cross-sectional survey)[11] were used to modify existing health belief scales to be culturally appropriate for KAs and to test the modified subscales of health beliefs to establish their psychometric properties. This study was conducted from January 2010 to June 2010 in the Chicago metropolitan area.
The study sample consisted of KAs who met the following inclusion criteria: (a) born in Korea and immigrated to the U.S., (b) aged 50 and older, and (c) at average risk for CRC (no history of Crohn's disease or ulcerative colitis, no history of CRC, no first-degree relative with CRC) based on the American Cancer Society's[2] guidelines. Individual interviews with 26 KAs were conducted using chain referral sampling (multiple snowballs) and quota sampling to recruit equal participants in terms of gender and age. Of the 26 KA participants, more KA women (57.7%) than KA men (42.3%) were interviewed. Middle-aged (aged 50 to 64) and older KAs (aged 65 and older) were evenly divided, with each group accounting for exactly half of the sample. Eleven KAs (36.4% men and 63.6% women; 63.6% aged 65 and older and 36.4% aged 50 to 64) were recruited for the pilot test using a combination of convenience and chain referral sampling (multiple snowballs), all of whom participated. A total of 277 KAs were recruited from a church, the Korean American Community Services and the Hanul Family Alliance.
In general, sample size guidelines for psychometric evaluation (i.e., confirmatory factor analysis [CFA]) are as follows: small samples (less than 100) may be appropriate for simple models but can result in data analysis issues; medium samples (100 to 200) may be acceptable if the model is not highly complex; and large samples (greater than 200) are acceptable for most models[12]. Given the use of instruments with 5 belief subscales and many indicators, the sample size sought in this study was at least 200, which would be acceptable for most models.
Belief variables for this study were derived from the HBM[10]. The model's constructs include perceived susceptibility (i.e., belief regarding the chance of getting a condition), perceived severity (i.e., belief about how serious a condition and its sequelae are), perceived benefits (i.e., belief in the efficacy of the advised action), perceived barriers (i.e., belief about the costs of the advised action), and self-efficacy (i.e., confidence in one's ability to take action)[10].
Health belief scales used to measure susceptibility, benefits, barriers, and self-efficacy in the present study were adapted from Menon et al.[13] after obtaining permission from the author. These scales have demonstrated good reliability, with Cronbach's alpha above .70. Construct validity was established using exploratory factor analysis with results confirming the unidimensionality of each health belief construct. Additionally, Champion's[14] severity scale was used in this study after obtaining permission from the author. This severity scale has demonstrated good reliability with Cronbach's alpha of .80[14]. The original health belief subscales (susceptibility, severity, benefits, barriers, and self-efficacy) included three susceptibility items, seven severity items, three benefit items, seven barrier items, and seven self-efficacy items. All scales in this study used five-point Likert response options ranging from "strongly disagree" (1) to "strongly agree" (5). Throughout the research process, items from the original health belief scales were modified, and several new items were added.
After translating the original scales into Korean, the successive study procedures (i.e., individual interviews, expert reviews, a pilot test, and a cross-sectional survey) were conducted using a Korean-language questionnaire, as Korean is the primary language spoken by 74.6% of foreignborn KAs[15].
The primary investigator (PI) drafted initial items for the health belief scales from existing instruments[13,14] and conducted a thorough literature review on Korean culture and cancer screening behaviors. Items were added to the scales in English based on previous studies[6,9]. Three bilingual translators who were fluent in both Korean and English translated the English version of the health belief scales into Korean using a committee translation method (the health belief scales Korean version 1). The PI and translation committee members reviewed the modified instruments for any discrepancies in translation and for unclear or awkward sentences.
Several issues emerged during translation of the original English instruments into the Korean version 1. Primarily, the medical term "fecal occult blood test" was replaced with lay language ("stool blood test"), as the medical term may be difficult to understand for KAs who are not employed in a health-related field. Therefore, the English phrase ("stool blood test") was translated into Korean as 대변 내 피검사 ("a test to detect blood in stool") by consensus among the committee members.
Additionally, difficulty emerged in translation of the item "not having privacy would keep you from having a stool blood test" into Korean. Privacy could be interpreted as several different Korean words depending on the context. The PI and committee members carefully appraised the situation of conducting a stool blood test and translated the aforementioned item into Korean as 다른 사람에게 알려지는 게 싫어서 ("not wanting to let other people know that he or she was doing the stool blood test or handling stool for the test.")
When the PI and translation committee members encountered difficulty reaching a consensus on translation, we sought guidance from either an expert or literature published in both Korean and English. For example, a 5-point Likert scale (1=strongly disagree, 2=disagree, 3=neutral, 4=agree, and 5=strongly agree) was used for all health belief scales. Committee members had difficulty finding an equivalent Korean word conveying the same meaning of "neutral" as in English. We found that one study had translated "neutral" into Korean as "don't know." We consulted an expert in survey methodology who indicated that "neutral" means "in-between agree and disagree" and deemed it inappropriate to label the midpoint "don't know" or "no opinion." We also found various published literature from South Korea that involved a 5-point Likert scale and used several Korean words for "neutral". One Korean word, 그저 그렇다 ("so-so"), was ultimately agreed upon by all translation committee members.
Cognitive interviewing techniques were used to assess KAs' health beliefs about CRC and FOBT utilization, to examine cultural differences in the operational definitions of the health belief concepts, and to make the scales culturally appropriate for KAs. The individual interviews with 26 KAs included two components: (a) a discussion of health beliefs and (b) a review of the health belief scales' items using cognitive interviewing.
Discussion of health beliefs concepts. Study participants were asked about their health beliefs related to CRC and FOBT behavior using semistructured and open-ended questions (Table 1). Most KAs reported that this study was the first instance in which they had heard about the stool blood test as an option for CRC screening. The main themes that emerged during the individual interviews included valuing family before self, seeing a doctor only if symptoms presented, and believing one would not get CRC. The scale items were validated as appropriate by the individual interviews because most themes mentioned by the participants during the interviews reflected these items. More detailed findings from the individual interviews exist elsewhere[16]. New items were added only to the barriers scale, as participants revealed many barriers to FOBT during individual interviews. The belief "I will be okay" was a commonly cited reason for not having an FOBT. Participants reported both general barriers (e.g., time or financial reasons, such as medical costs and health insurance) and cultural barriers (e.g., fear of being a burden to the family if diagnosed with CRC) to having an FOBT.
Cognitive interviews. Participants reviewed all health belief scales during cognitive interviews and agreed that most scale items were culturally appropriate for KAs. After discussion of concepts, the concurrent verbal probing method[11] (e.g., the PI began with scripted probes and used unscripted follow-up probes if necessary) was used to review the health belief scale items. Using this cognitive interviewing technique, the PI evaluated sources of response error in survey questionnaires and observed both how KAs understand and interpret the items for health scales and how this understanding differed from a Western cultural perspective.
Several other issues emerged during cognitive interviews. First, some KAs understood "stool blood test" to be a general blood test. Thus, the PI consulted with the translation committee members to find a more appropriate Korean translation. After discussion, the Korean translation was modified to 대변혈검사 ("stool test") to emphasize stool rather than blood. Second, some KAs did not understand the meaning of the term privacy on the barriers items. Participants reported that it was difficult to understand the relationship between privacy and the stool blood test. Hence, the PI consulted with the author who developed the barrier scale. The author clarified that the term privacy related to the ability to conduct the FOBT alone at home. For example, someone in a large family may have only one bathroom and be unable to take the required amount of time to perform the test, indicating a lack of privacy. The PI and translation committee members discussed this item and decided to include the above explanations because KAs may not understand the item if only the word "privacy" was translated into Korean. Additionally, KAs may not be familiar with the concept of privacy within the family due to close-knit relationships among family members in the traditional Korean family system. Therefore, the item was rephrased in Korean as, "It is hard to use a bathroom alone, which would keep me from having an FOBT". Third, KAs revealed they did not understand the barrier item, "I have other problems more important than having a stool blood test", as several participants subsequently asked, "What other problems? What does that mean?" After discussion with the translation committee members, the item was rephrased as "Having a stool blood test is not the most urgent and important problem I have, which keeps me from having it."
The individual interviews were conducted in Korean and recorded by audiotape. Each individual interview lasted approximately 80 to 120 minutes. Based on findings from analysis of the individual interviews, the PI revised the initial scales by modifying or adding items after discussion and consultation with translation committee members and experts in Korean culture and/or cancer screening research. These efforts produced the Korean version 2 scales.
Three Korean researchers with doctoral degrees in health-related areas and expertise in Korean culture and/or cancer screening research reviewed the content of the health belief scales (Korean version 2) to ensure content validity. Both quantitative (categorization of the level of judgment) and qualitative procedures (written comments about specific items) were used for content review. Each expert was asked to independently rate the content representativeness on a four-point ordinal scale (1=the item is not representative of a measure; 2=the item needs major revision to be representative of a measure; 3=the item needs minor revision to be representative of a measure; 4=the item is representative of a measure). Experts also provided written comments and suggestions related to item content, wording clarity, and the comprehensiveness of the subscale.
The PI calculated the item-level content validity index (I-CVI) and the scale-level content validity index (S-CVI). The I-CVI is calculated as the number of experts giving a rating of either 3 or 4 divided by the total number of experts[17]. The S-CVI/Ave (average proportion of items rated as 3 or 4 across the various judges) was calculated by summing the I-CVIs and dividing by the number of items[17].
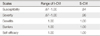
Three experts rated the survey questionnaire items using an ordinal four-point scale. The I-CVI ranged from .67 to 1.0, whereas the S-CVI ranged from .84 to 1.0 (see Table 2). The PI reviewed I-CVIs lower than 1.0 and S-CVIs lower than .90 to consider item revision and/or deletion; the items were ultimately modified based on expert recommendations. Two susceptibility items ("I will get colon cancer"; "I will get colon cancer sometime during my lifetime") and one severity item ("Problems I would experience with colon cancer would last a long time") had I-CVI values lower than 1.0. However, all three items were retained in the scales because susceptibility and severity items have been tested in many cancer-screening studies with diverse populations, including KAs, and have been proven reliable and valid.
Pilot testing of the scales was conducted to assess respondents' understanding of questions on version 3 of the health belief scale. The PI gave participants a survey packet containing a questionnaire and a consent form either in person or via mail, and packets were returned in kind. The PI documented the survey start and completion times, took notes about questions on survey items during the survey, and questioned participants about any difficulties they experienced once they completed the surveys. Findings from the pilot study demonstrated the feasibility of a larger study, as all respondents successfully completed the questionnaire. The amount of time taken to complete the instrument ranged from 60 to 90 minutes. The participants reported issues with redundant wording and numbers, which the PI removed. The response rate for the pilot test was 100%.
The aim of the cross-sectional survey was to test the psychometric properties of the modified health beliefs subscales (susceptibility, severity, benefits, barriers, and self-efficacy) related to FOBT utilization among KAs aged 50 and older. The PI provided KAs a survey package in person that included a self-administered questionnaire, a consent form, and a stamped return envelope. Participants returned the consent form and questionnaire to the PI either in person or by mail.
Modified health beliefs scales based on findings from the individual interviews, expert reviews, and pilot test were used for the cross-sectional survey. The final version of the health belief scales on the study questionnaire consisted of the following: susceptibility (4 items), severity (8 items), benefits (5 items), barriers (22 items), and self-efficacy (7 items). Table 4 shows the original and modified items on the health belief subscales.
This study was approved by the institutional review board of the University (IRB No. 2009-1088). Verbal or written informed consent, including information on protection of privacy and confidentiality, was translated into Korean and obtained from all participants. To ensure the protection of confidential participant information, all study materials, including audiotapes, signed consent forms, and paper surveys, were stored in a locked file cabinet in the PI's office at the University's College of Nursing.
The final health belief subscales were tested for construct validity (exploratory factor analysis [EFA] and confirmatory factor analysis [CFA]) and reliability (internal consistency reliability) using SPSS Version 18[18] and the Amos 18 program[19]. An EFA is used to determine what a subscale's underlying structure is, while a CFA is used to confirm a particular pattern of relationships predicted on the basis of theory[20]. Thus, an EFA using principal components extraction with a varimax rotation was conducted, and a scree plot was used to identify the number of factors. Additionally, a CFA using a structural equation modeling (SEM) with oblique (intercorrelated) factors was performed. Each scale was factored separately during SEM. SEM was performed using three procedures, including model specification, data specification, and the calculation of parameter estimates within the framework of AMOS Graphics. Adequate fit for the SEM models was based on achievement of a relative chi-square (chisquare divided by degrees of freedom) less than 2.0[20]. Model modification (respecification) was performed by adding a covariance between the paired item error terms of the high modification indices value in AMOS Graphics. Factor loadings of each item were expected to be .40 or greater, as suggested by Nunnally[21]. Internal consistency reliability analysis was performed with all items from each scale using SPSS. Each of the subscales was expected to have internal consistency reliability with a Cronbach's alpha of .70 or greater based on DeVellis'[22] recommendation.
Of the 277 KAs recruited, 202 completed and returned the surveys response rate=72.9%) either in person or by mail. The mean age of participants was 63.92 (SD=8.86; ranges 50~84). Sixty-three percent of respondents were female, and 37% were male. The mean number of years in the U.S. was 27 (SD=9.28). Forty-one percent had attained a bachelor degree or higher, 26% had attained a high school diploma, and 9% had attained an 8th grade education or lower. Seventy-eight percent were married, 11% were widowed, and 8% were divorced. Sixty-seven percent had health insurance, and 33% did not have health insurance.
The EFA showed that determination of factors to be extracted and interpreted was most meaningful when 4 factors were extracted. Barriers items loaded on factor 1, susceptibility and severity items loaded on factor 2, self-efficacy items loaded on factor 3, and benefits items loaded on factor 4 (Table 3). Four factors accounted for 41.8% of the variance and represented eigenvalues that were greater than 1. Four factors extracted from results of the EFA were subjected to the CFA using SEM to determine how well items fit theoretical concepts. The models of all scales did not fit observed data, indicating the need for model respecification. Table 4 shows factor loadings of final scale models by SEM. Factor loadings ranged from .06 to .99.
The addition of items reflecting family perspectives to the severity scale ("if I had colon cancer, it would disrupt the harmony in my family"), the benefits scale ("stool blood test can help me reduce a burden to my family by finding colon cancer early"), and the barriers scale ("fear of being a burden to the family if diagnosed with colon cancer would keep me from having a stool blood test") contributed to good scale validity. However, some items from the original health belief scales and newly added items had weak validity. For instance, the EFA indicated that five items (one item from the original scale and four newly added items) were not greater than .40, including four barriers items and one susceptibility item. The CFA indicated that a total of 12 items (seven items from the original scale and five newly added items) had factor loadings less than .40, including all four susceptibility items, one benefit item, five barriers items, and two self-efficacy items. Out of these poorly performing items, four items had factor loadings less than .40 in both EPA and CFA, including one susceptibility item and three barriers items. The susceptibility item was "as I get older, my chances of getting colon cancer increase". The three barriers items were "no interest of having a stool blood test would keep me from having it", "at my age, a stool blood test is not necessary, which would keep me from it", and "other colon cancer screening options such as colonoscopy are more accurate than a stool blood test, which would keep me from having a stool blood test".
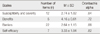
Table 5 shows the number of items, the item mean, the mean of item standard deviations (SDs), and Cronbach's alpha for each subscale. For all subscales, the Cronbach's alpha values were more than .70. Overall, all scales demonstrated good reliability.
The purpose of this study was to report modification and validation processes of culturally appropriate instruments for measuring beliefs about CRC and CRC screening utilization among KAs using findings from translation, individual interviews, expert reviews, pilot testing and a cross-sectional survey. Few studies have reported details regarding the modification and validation processes for Korean versions of instruments on beliefs about CRC. To the best of our knowledge, this study is the first to report the sequential process of developing culturally appropriate measures of CRC screening behaviors among KAs.
Methodologically, scale modification was more appropriate than development of a new instrument because results of modification and validation processes showed that most scale items that were adapted from existing instruments were appropriate for Korean culture. The reliability and validity of belief scales used in this study had previously been established[13,14]; hence, few changes in the scales were needed for Korean cultural appropriateness. These findings are consistent with scale development and modification guidelines[8], which indicate that scale adaptation and modification rather than scale development are appropriate if constructs or item contents overlap but are slightly different.
The sequential, methodological steps of this study included translation, individual interviews, and expert reviews to ensure that the final instrument was culturally appropriate. Several important issues were highlighted in the translation and individual interviews stages. First, translation issues in this study reflected both cultural issues (i.e., privacy) and linguistic issues (translation of the terms "stool blood test" and "neutral"). Privacy is understood differently in different cultures. In Western countries, privacy refers to an individual's ability to manage personal information and space (e.g., the ability to avoid public disclosure of personal information)[23]. However, the concept of privacy in Eastern countries is different from its Western counterpart. For example, some researchers have asserted that there is no concept of privacy in traditional Chinese culture; thus, Chinese people do not understand the term[23]. This misunderstanding may be a result of the fact that relations among Chinese family members are highly intimate, open and honest[23]. Similar to the Chinese, KAs in this study did not understand what privacy meant and why it was a barrier to cancer screening during cognitive interviews. KAs traditionally have close-knit family relationships, so the need for privacy to perform CRC screening is not a key barrier for them. In regards to linguistic issues that emerged, we encountered difficulties finding appropriate words to substitute for "stool blood test" and "neutral" in Korean. Through literature reviews, discussion with translation committee members and experts, and cognitive interviews with participants, the PI found appropriate translations that were validated by participants and experts.
In contrast to frequently used methods of cross-cultural adaptation in previous studies (i.e., translation, synthesis, back translation, expert committee review, and pretesting)[24], in this study individual interviews related to health beliefs were conducted and a review of scale items using cognitive interview techniques to make scales culturally appropriate was done. During individual interviews, the combination of methods related to beliefs discussion and participants' reviews of survey questions using the cognitive interview technique was useful because it identified KAs' beliefs more deeply and precisely. First, the PI learned KAs' general thoughts about health beliefs through the concept discussion; the subsequent review of survey questions with participants during cognitive interviews confirmed what participants discussed. This process allowed the PI to identify scale items that needed to be added or modified because the participants elaborated concepts more specifically during cognitive interviews after first discussing the concepts generally.
The newly added items related to barriers to CRC screening among KAs. Several new barriers items reflect Korean traditional beliefs about health and CRC screening, such as familism and unrealistic optimism (e.g., believing that they would not get CRC)[16], which contrast with Western beliefs, such as individualism and awareness of vulnerability to illness[13].
Qualitative (individual interviews) and quantitative (survey) methods were used to understand health beliefs about CRC screening among KAs. Based on qualitative data, items reflecting Korean cultural perspectives (e.g., familism) were added to the scales for susceptibility, severity, benefits, and barriers. Overall, revised scales became more culturally sensitive by adding KAs' perspectives on the interpersonal context of CRC screening to original scales that emphasized Western intrapersonal perspectives on CRC screening.
We examined psychometric properties such as the validity and reliability of CRC belief scales with a large sample of KAs following the revision processes. Although all scales demonstrated good internal consistency reliability (i.e., Cronbach's alpha values greater than .70), construct validity testing partially supported the validity of the instruments used in this study. Interestingly, the EFA extracted 1 factor for both susceptibility and severity in this study, which is consistent with the initial HBM[10]. Susceptibility and severity were collectively identified as a threat and were initially combined in the HBM as a predictor of health behaviors[10]. A previous study with a diverse ethnic population (68% Caucasian, 30% African-American and 2% others)[25] indicated that both susceptibility and severity need to get cancer screening; in contrast, little variance is found in breast cancer severity, and susceptibility alone is used as the threat variable. In the case of KAs, the EFA indicated that both susceptibility and severity loaded on one factor (which can be named a threat based on the HBM) and the CFA further indicated that severity was a main threat variable. Therefore, our data supporting the revised instruments are still grounded in the HBM.
The unrealistic optimism related to CRC susceptibility among KAs found from individual interviews in this study were consistent with a previous study[6] that KAs have low perceived susceptibility related to CRC and that they may be overly confident in their chances of developing CRC compared to other groups. A limited body of research is available on unrealistic optimism regarding cancer among KAs. One recent cross-sectional survey[26] conducted in Korea with a convenience sample of 600 individuals aimed to identify relationships between optimistic bias about cancer and cancer preventive behavior in Korean, Chinese, American, and Japanese residents in Korea. Results of the study showed that Koreans had the highest level of unrealistic optimism about cancer among the diverse ethnic groups studied and that participants with optimistic bias about cancer were less likely to engage in cancer preventive behavior[26].
Out of 46 items, the EFA demonstrated that 5 items had factor loadings less than .40, and the CFA demonstrated that 12 items had factor loadings less than .40. Although items from the original scales had good reliability and validity in previous studies[27,28], some items (e.g., "having a stool blood test will help me not worry as much about colon cancer", "I can obtain a stool blood test kit") had weak validity in this study. The poor performance of these items might relate to (a) lack of knowledge about FOBT and (b) the multidimensionality of the scales. First, the weak validity of benefits items (e.g., "having a stool blood test will help me not worry as much about colon cancer"), and self-efficacy items (e.g., "I can obtain a stool blood test kit") in this study might relate to the lack of knowledge regarding FOBT. Given that KA participants during individual interviews reported they had never heard about FOBT, they did not know how FOBTs worked, and they assumed FOBT would help find CRC, it may be difficult for KAs to respond to the items on these scales. Second, the barriers scale was highly multi-dimensional. Many barrier items, including affection (fear and being embarrassed), financial problems, privacy, symptoms, physician recommendations, and communication in English, were used in this study. In fact, the EFA using SPSS indicated six eigenvalues greater than one in the barriers scale, indicating that this scale was multi-dimensional. Surprisingly, the CFA revealed that two barriers items assessing absence of symptoms and lack of physician recommendation were not good indicators of barriers to FOBT in this study, although previous studies[29,30] have indicated that these items are important barriers to cancer screening. Due to the multidimensionality of the barriers scale, these two barrier items may not load on one factor and thus had weak validity.
This study had limitations. First, generalizability may be limited because a voluntary convenience-sampling method was used with KAs in Chicago. Thus, findings should be limited to the period January to June 2010 in Chicago and should not be considered representative of the entire population. Further research studies are needed that investigate the prevalence of and beliefs about FOBT with a larger sample of KAs from different geographic areas to improve the generalizability of findings.
Scale modification and validation processes using existing instruments based on the HBM designed to measure beliefs about CRC screening utilization are described in this study. The instruments revised to be culturally appropriate were validated for reliability and validity with KAs. Because few studies have reported instrument modification and validation processes related to CRC beliefs among KAs or have highlighted the methodological and conceptual issues relevant to instruments for KAs, the methodology, sequential processes of translation, individual interviews, expert reviews, pilot testing and cross-sectional survey utilized in this study will be helpful for future research on CRC screening among KAs. Clinicians and researchers should be able to more accurately measure KAs' CRC screening beliefs by using the revised instruments instead of the original instruments.
Figures and Tables
Notes
References
1. Gomez SL, Noone AM, Lichtensztajn DY, Scoppa S, Gibson JT, Liu L, et al. Cancer incidence trends among Asian American populations in the United States, 1990-2008. J Natl Cancer Inst. 2013; 105(15):1096–1110. DOI: 10.1093/jnci/djt157.
2. American Cancer Society. Colorectal cancer facts & figures 2014-2016. Atlanta, GA: Author;2014.
3. Lee HY, Lundquist M, Ju E, Luo X, Townsend A. Colorectal cancer screening disparities in Asian Americans and Pacific Islanders: Which groups are most vulnerable? Ethn Health. 2011; 16(6):501–518. DOI: 10.1080/13557858.2011.575219.
4. Maxwell AE, Crespi CM. Trends in colorectal cancer screening utilization among ethnic groups in California: Are we closing the gap? Cancer Epidemiol Biomarkers Prev. 2009; 18(3):752–759. DOI: 10.1158/1055-9965.epi-08-0608.
5. Lee HY, Im H. Colorectal cancer screening among Korean American immigrants: Unraveling the influence of culture. J Health Care Poor Underserved. 2013; 24(2):579–598. DOI: 10.1353/hpu.2013.0087.
6. Jo AM, Maxwell AE, Wong WK, Bastani R. Colorectal cancer screening among underserved Korean Americans in Los Angeles County. J Immigr Minor Health. 2008; 10(2):119–126. DOI: 10.1007/s10903-007-9066-6.
7. Sanders Thompson VL. Cultural context and modification of behavior change theory. Health Educ Behav. 2009; 36:5 Suppl. 156S–160S.
8. van de Vijver FJR, Leung K. Methods and data analysis for cross-cultural research. Thousand Oaks, CA: SAGE Publications;1997.
9. Lee EE, Fogg L, Menon U. Knowledge and beliefs related to cervical cancer and screening among Korean American women. West J Nurs Res. 2008; 30(8):960–974. DOI: 10.1177/0193945908319250.
10. Becker MH, editor. The health belief model and personal health behavior. Thorofare, NJ: C. B. Slack;1974.
11. Willis GB. Cognitive interviewing: A tool for improving questionnaire design. Thousand Oaks, CA: SAGE Publications;2005.
12. Kline RB. Principles and practice of structural equation modeling. 2nd ed. New York, NY: Guilford;2005.
13. Menon U, Champion VL, Larkin GN, Zollinger TW, Gerde PM, Vernon SW. Beliefs associated with fecal occult blood test and colonoscopy use at a worksite colon cancer screening program. J Occup Environ Med. 2003; 45(8):891–898. DOI: 10.1097/01.jom.0000083038.56116.30.
14. Champion VL. Instrument refinement for breast cancer screening behaviors. Nurs Res. 1993; 42(3):139–143.
15. United States Census Bureau. Place of birth by citizenship status. Universe: Total population 2006-2010 American Community Survey selected population tables. Washington, DC: Author;2010. cited 2013 February 21. Available from: http://factfinder.census.gov/faces/tableservices/jsf/pages/productview.xhtml?pid=ACS_10_SF4_B05002&prodType=table.
16. Lee SY, Lee EE. Korean Americans’ beliefs about colorectal cancer screening. Asian Nurs Res (Korean Soc Nurs Sci). 2013; 7(2):45–52. DOI: 10.1016/j.anr.2012.10.001.
17. Polit DF, Beck CT. The content validity index: Are you sure you know what’s being reported? Critique and recommendations. Res Nurs Health. 2006; 29(5):489–497. DOI: 10.1002/nur.20147.
18. SPSS Inc. SPSS 18.0 for windows. Chicago, IL: Author;2009.
19. Arbuckle JL. AMOS 18: User's guide. Chicago, IL: SPSS Inc.;2009.
20. Ullman JB. Structural equation modeling. In : Tabachnick BG, Fidell LS, editors. Using multivariate statistics. 4th ed. Boston, MA: Allyn & Bacon;2001. p. 653–771.
21. Nunnally JC. Psychometric theory. 2nd ed. New York, NY: McGraw Hill;1978.
22. DeVellis RF. Scale development: Theory and applications. Newbury Park, CA: SAGE Publications;1991.
23. Chan YK. Privacy in the family: Its hierarchical and asymmetric nature. J Comp Fam Stud. 2000; 31(1):1–17.
24. Beaton DE, Bombardier C, Guillemin F, Ferraz MB. Guidelines for the process of cross-cultural adaptation of self-report measures. Spine (Phila Pa 1976). 2000; 25(24):3186–3191.
25. Champion VL. Revised susceptibility, benefits, and barriers scale for mammography screening. Res Nurs Health. 1999; 22(4):341–348.
26. Lee SH, Ham EM. The relationship between the optimistic bias about cancer and cancer preventive behavior of the Korean, Chinese, American, and Japanese adult residing in Korea. J Korean Acad Nurs. 2010; 40(1):52–59. DOI: 10.4040/jkan.2010.40.1.52.
27. Champion VL. Development of a benefits and barriers scale for mammography utilization. Cancer Nurs. 1995; 18(1):53–59.
28. Rawl S, Champion V, Menon U, Loehrer PJ, Vance GH, Skinner CS. Validation of scales to measure benefits of and barriers to colorectal cancer screening. J Psychosoc Oncol. 2001; 19(3-4):47–63. DOI: 10.1300/J077v19n03_05.
29. Maxwell AE, Bastani R, Warda US. Demographic predictors of cancer screening among Filipino and Korean immigrants in the United States. Am J Prev Med. 2000; 18(1):62–68. DOI: 10.1016/S0749-3797(99)00110-5.
30. Kandula NR, Wen M, Jacobs EA, Lauderdale DS. Low rates of colorectal, cervical, and breast cancer screening in Asian Americans compared with non-Hispanic whites: Cultural influences or access to care? Cancer. 2006; 107(1):184–192. DOI: 10.1002/cncr.21968.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download