Abstract
Purpose
The aims of this study were to construct a hypothetical structural model which explains the premenstrual syndrome (PMS) in adolescent girls and to test the fitness with collected data.
Methods
The participants were 1,087 adolescent girls from 3 high schools and 5 middle schools in B city. Data were collected from July 3 to October 15, 2012 using self-reported questionnaires and were analyzed using PASW 18.0 and AMOS 16.0 programs.
Results
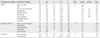
The overall fitness indices of hypothetical model were good (χ2 =1555, p<.001), χ2/df=4.40, SRMR=.04, GFI=.91, RMSEA=.05, NFI=.90, TLI=.91, CFI=.92, AIC=1717). Out of 16 paths, 12 were statistically significant. Daily hassles had the greatest impact on PMS in the adolescent girls in this model. In addition, PMS in adolescent girls was directly affected by menarche age, Body Mass Index (BMI), amount of menstruation, test anxiety, social support, menstrual attitude and femininity but not by academic stress. This model explained 27% of the variance in PMS in adolescent girls.
Figures and Tables
References
1. Lee MH. Abnormal pubertal development in Korean adolescent girls. Korean J Obstet Gynecol. 2009; 52(12):1197–1203.
2. Sung MH, Joo KS. Relationships among attitudes toward menstruation, peri-menstrual symptoms, and coping in adolescent girls. Korean J Health Promot. 2011; 11(2):106–114.
3. Chang HJ, Jeong HG, Ko YH, Han CS, Joe SH. Frequency, clinical characteristics and correlates of premenstrual syndrome in high school students. Korean J Psychosom Med. 2013; 21(1):44–54.
4. Statistics Korea, The Ministry of Gender Equality & Family. Adolescent statistics 2012 [Internet]. Daejeon: Statistics Korea;2012. cited 2012 November 1. Available from: http://kostat.go.kr/portal/korea/kor_nw/2/1/index.board?bmode= read&aSeq=255358.
5. Park JW, Kim JS, Lee KY, Park TJ, Kim SH. Factors associated with premenstrual syndrome in high school students. Korean J Fam Med. 2009; 30(9):710–716. http://dx.doi.org/10.4082/kjfm.2009.30.9.710.
6. Gollenberg AL, Hediger ML, Mumford SL, Whitcomb BW, Hovey KM, Wactawski-Wende J, et al. Perceived stress and severity of perimenstrual symptoms: The BioCycle study. J Womens Health (Larchmt). 2010; 19(5):959–967. http://dx.doi.org/10.1089/jwh.2009.1717.
7. Parker MA, Sneddon AE, Arbon P. The menstrual disorder of teenagers (MDOT) study: Determining typical menstrual patterns and menstrual disturbance in a large population-based study of Australian teenagers. BJOG. 2010; 117(2):185–192. http://dx.doi.org/10.1111/j.1471-0528.2009.02407.x.
8. Delara M, Ghofranipour F, Azadfallah P, Tavafian SS, Kazemnejad A, Montazeri A. Health related quality of life among adolescents with premenstrual disorders: A cross sectional study. Health Qual Life Outcomes. 2012; 10:1. http://dx.doi.org/10.1186/1477-7525-10-1.
9. Kim SM. A study on premenstrual syndrome, dietary behavior and life habits among high school girls [master's thesis]. Seoul: Dongguk University;2012.
10. Rizk DE, Mosallam M, Alyan S, Nagelkerke N. Prevalence and impact of premenstrual syndrome in adolescent schoolgirls in the United Arab Emirates. Acta Obstet Gynecol Scand. 2006; 85(5):589–598. http://dx.doi.org/10.1080/00016340600556049.
11. Wong LP, Khoo EM. Menstrual-related attitudes and symptoms among multi-racial Asian adolescent females. Int J Behav Med. 2011; 18(3):246–253. http://dx.doi.org/10.1007/s12529-010-9091-z.
12. Bertone-Johnson ER, Hankinson SE, Willett WC, Johnson SR, Manson JE. Adiposity and the development of premenstrual syndrome. J Womens Health (Larchmt). 2010; 19(11):1955–1962. http://dx.doi.org/10.1089/jwh.2010.2128.
13. Cosgrove L, Riddle B. Constructions of femininity and experiences of menstrual distress. Women Health. 2003; 38(3):37–58. http://dx.doi.org/10.1300/J013v38n03_04.
14. Lee HK. Impact of perfectionism and testing anxiety on the menstrual cycle during test evaluations among high school girls. Korean J Women Health Nurs. 2008; 14(4):314–322. http://dx.doi.org/10.4069/kjwhn.2008.14.4.314.
15. Eissa M. Personality and psychosocial factors affecting premenstrual syndrome. Curr Psychiatr. 2010; 17(1):55–61.
16. Lenz ER, Pugh LC, Milligan RA, Gift A, Suppe F. The middle-range theory of unpleasant symptoms: An update. ANS Adv Nurs Sci. 1997; 19(3):14–27.
17. Kim H, Kim S, Lee H, Oh S. Factors affecting symptom experiences of breast cancer patients: Based on the theory of unpleasant symptoms. Asian Oncol Nurs. 2014; 14(1):7–14. http://dx.doi.org/10.5388/aon.2014.14.1.7.
18. Kirkpatrick MK, Brewer JA, Stocks B. Efficacy of self-care measures for perimenstrual syndrome (PMS). J Adv Nurs. 1990; 15(3):281–285.
19. Lee YS, Park CS, Lee HK, Park YJ. Maternity and women's health nursing. 3rd ed. Seoul: Hyunmoon;2014.
20. Masho SW, Adera T, South-Paul J. Obesity as a risk factor for premenstrual syndrome. J Psychosom Obstet Gynaecol. 2005; 26(1):33–39.
21. Jöreskog KG, Sörbom D. LISREL 7: A guide to the program and applications. 2nd ed. Chicago, IL: SPSS Inc.;1989.
22. Park SY. A study on stress level and coping style of adolescents [master's thesis]. Chuncheon: Kangwon National University;1998.
23. Oh MH, Cheon SM. Analysis of academic stressors and symptoms of juveniles and effects of meditation training on academic stress reduction. Underst People. 1994; 15:63–96.
24. Spielberger CD. Preliminary professional manual for the test anxiety inventory TAI. Palo Alto, CA: Consulting Psychologists Press;1980.
25. Lee MR. A study on the social support system to influence on the high school students' adaptation to school life [master's thesis]. Daegu: Daegu University;2000.
26. Yang DO, Youn G. Attitudes toward menstruation according to the increased years after menarche. Korean J Woman Psychol. 2001; 6(3):37–48.
27. Chung JK. Korean sex role inventory (KSRI). Korean J Soc Psychol. 1990; 5(1):82–92.
28. Kim HW, Kwon MK. Study on the validity and reliability of MMDQ (Moos menstrual distress questionnaire) among middle school students. Korean Parent Child Health J. 2004; 7(2):111–120.
29. Shin MA. A structural model of premenstrual symptom in female college students [dissertation]. Seoul: Hanyang University;2005.
30. Shin Y, Kang SJ. Health behaviors and related demographic factors among Korean adolescents. Asian Nurs Res. 2014; 8(2):150–157.
31. Ryu E, Seo J, Ham M, Park Y, Moon S, Nam B. Sex-role identity in adolescents and its relation to anxiety, depression and suicidal ideation. J Korean Acad Psychiatr Ment Health Nurs. 2006; 15(2):136–143.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download