Abstract
Purpose
This study was done to identify pain perception (P-PER) by nurses and pain expression (P-EXP) by patients in critical care units (ICUs) and degree of agreement between nurses' P-PER and patients' P-EXP.
Methods
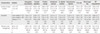
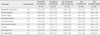
Nurses' P-PER was measured with a self-administered questionnaire completed by 99 nurses working in ICUs during May, 2013. Patients' P-EXP was measured with the Critical Care Non-Verbal Pain Scale through observations of 31 ICU patients during nine nursing procedures (NPs) performed between May and July, 2013.
Results
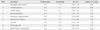
Nurses' P-PER was from 4.49 points for nasogastric tube (NGT) insertion to 0.83 for blood pressure (BP) measurement based on a 9-point scale, Patients' P-EXP was 4.48 points for NGT to 0.18 for BP measurement based on a 10-point scale. Eight NPs except oral care showed higher scores for nurses' P-PER than for patients' P-EXP. Position change (p=.019), subcutaneous injection (p<.001), blood sugar test (p<.001), and BP measurement (p<.001) showed significant differences between nurses' P-PER and patients' P-EXP.
Figures and Tables
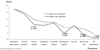 | Figure 1Comparison of pain perception of nurses and pain expression of patients for nursing procedures. |
References
1. International Association for the Study of Pain Subcommittee on Taxonomy. Pain terms: A list with definitions and notes on usage. Recommended by the IASP subcommittee on taxonomy. Pain. 1979; 6(3):249–252.
2. Carbajal R, Rousset A, Danan C, Coquery S, Nolent P, Ducrocq S, et al. Epidemiology and treatment of painful procedures in neonates in intensive care units. JAMA. 2008; 300(1):60–70. http://dx.doi.org/10.1001/jama.300.1.60.
3. Puntillo KA, Max A, Timsit JF, Vignoud L, Chanques G, Robleda G, et al. Determinants of procedural pain intensity in the intensive care unit. The Europain® study. Am J Respir Crit Care Med. 2014; 189(1):39–47. http://dx.doi.org/10.1164/rccm.201306-1174OC.
4. Puntillo KA, White C, Morris AB, Perdue ST, Stanik-Hutt J, Thompson CL, et al. Patients' perceptions and responses to procedural pain: Results from thunder project II. Am J Crit Care. 2001; 10(4):238–251.
5. de Jong A, Molinari N, de Lattre S, Gniadek C, Carr J, Conseil M, et al. Decreasing severe pain and serious adverse events while moving intensive care unit patients: A prospective interventional study (the NURSE-DO project). Crit Care. 2013; 17(2):R74. http://dx.doi.org/10.1186/cc12683.
6. Greisen J, Juhl CB, Grøfte T, Vilstrup H, Jensen TS, Schmitz O. Acute pain induces insulin resistance in humans. Anesthesiology. 2001; 95(3):578–584.
7. Alsaadi SM, McAuley JH, Hush JM, Lo S, Lin CW, Williams CM, et al. Poor sleep quality is strongly associated with subsequent pain intensity in patients with acute low back pain. Arthritis Rheumatol. 2014; 66(5):1388–1394. http://dx.doi.org/10.1002/art.38329.
8. Courtenay M, Carey N. The impact and effectiveness of nurse-led care in the management of acute and chronic pain: A review of the literature. J Clin Nurs. 2008; 17(15):2001–2013. http://dx.doi.org/10.1111/j.1365-2702.2008.02361.x.
9. Registered Nurses' Association of Ontario. Assessment and management of pain. 3rd ed. Toronto, CA: Author;2013.
10. Hwang KH, Ryoo EN, Park KS. A study of the nurses' knowledge and attitude about pain management. J Korean Acad Soc Nurs Educ. 2007; 13(1):41–51.
11. Song SS, Park CS. Pain management knowledge and attitude of internal medicine and surgery stream nurses. J Korean Acad Soc Home Care Nurs. 2010; 17(1):55–62.
12. Bergeron DA, Leduc G, Marchand S, Bourgault P. Descriptive study of the postoperative pain assessment and documentation process in a university hospital. Pain Res Manag. 2011; 16(2):81–86.
13. Puntillo K, Neighbor M, O'Neil N, Nixon R. Accuracy of emergency nurses in assessment of patients' pain. Pain Manag Nurs. 2003; 4(4):171–175.
14. Payen JF, Bru O, Bosson JL, Lagrasta A, Novel E, Deschaux I, et al. Assessing pain in critically ill sedated patients by using a behavioral pain scale. Crit Care Med. 2001; 29(12):2258–2263.
15. Gélinas C, Fillion L, Puntillo KA, Viens C, Fortier M. Validation of the critical-care pain observation tool in adult patients. Am J Crit Care. 2006; 15(4):420–427.
16. Choi EH, Kim JH, Choi KO, Yoo JS, Kim MS, Kim PJ, et al. Development of a pain assessment tool for critically ill patients. J Korean Clin Nurs Res. 2012; 18(1):136–148.
17. Choi EH, Kim JH, Ko MS, Kim JY, Kwon EO, Jang IS. Validation of critical care non-verbal pain scale for critically ill patients. J Korean Clin Nurs Res. 2013; 19(2):245–254.
18. Gélinas C, Fortier M, Viens C, Fillion L, Puntillo K. Pain assessment and management in critically ill intubated patients: A retrospective study. Am J Crit Care. 2004; 13(2):126–135.
19. Rose L, Haslam L, Dale C, Knechtel L, Fraser M, Pinto R, et al. Survey of assessment and management of pain for critically ill adults. Intensive Crit Care Nurs. 2011; 27(3):121–128. http://dx.doi.org/10.1016/j.iccn.2011.02.001.
20. Chanques G, Jaber S, Barbotte E, Violet S, Sebbane M, Perrigault PF, et al. Impact of systematic evaluation of pain and agitation in an intensive care unit. Crit Care Med. 2006; 34(6):1691–1699. http://dx.doi.org/10.1097/01.ccm.0000218416.62457.56.
21. Chanques G, Sebbane M, Barbotte E, Viel E, Eledjam JJ, Jaber S. A prospective study of pain at rest: Incidence and characteristics of an unrecognized symptom in surgical and trauma versus medical intensive care unit patients. Anesthesiology. 2007; 107(5):858–860. http://dx.doi.org/10.1097/01.anes.0000287211.98642.51.
22. Payen JF, Chanques G, Mantz J, Hercule C, Auriant I, Leguillou JL, et al. Current practices in sedation and analgesia for mechanically ventilated critically ill patients: A prospective multicenter patient-based study. Anesthesiology. 2007; 106(4):687–695. http://dx.doi.org/10.1097/01.anes.0000264747.09017.da.
23. Gélinas C. Management of pain in cardiac surgery ICU patients: Have we improved over time? Intensive Crit Care Nurs. 2007; 23(5):298–303. http://dx.doi.org/10.1016/j.iccn.2007.03.002.
24. Kim DH, Kim C, Sohn KT, Jeong KM, Chung Y, Choi YS, et al. Statistics: Theory and application. Paju: Freeacademy;2003.
25. Siffleet J, Young J, Nikoletti S, Shaw T. Patients' self-report of procedural pain in the intensive care unit. J Clin Nurs. 2007; 16(11):2142–2148. http://dx.doi.org/10.1111/j.1365-2702.2006.01840.x.
26. Resnick S, Morrison RS. Physicians' perceptions of procedural pain and discomfort. J Palliat Med. 2004; 7(5):646–651.
27. Koeppen BM, Stanton BA. Berne & Levy physiology. 6th ed. Philadelphia, PA: Mosby;2009.
28. Korea Institute for Healthcare Accreditation. KOIHA evaluation criteria for healthcare accreditation: Tertiary general hospital (Ver 2.0). Seoul: Ministry of Health & Welfare, Korea Institute for Healthcare Accreditation;2014.
29. Li KK, Harris K, Hadi S, Chow E. What should be the optimal cut points for mild, moderate, and severe pain? J Palliat Med. 2007; 10(6):1338–1346. http://dx.doi.org/10.1089/jpm.2007.0087.
30. World Health Organization. Pain relief ladder for cancer pain relief [Internet]. Geneva: World Health Organization;2012. cited 2014 July 28. Available from: http://www.who.int/cancer/palliative/painladder/en/.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download