Abstract
Purpose
This study was to develop a breastfeeding promotion program and to test effects of the program on levels of breast discomfort, breast size, sodium in breast milk, and type of feeding in mothers with breast engorgement following cesarean birth.
Methods
A non-synchronized non-equivalent control group pretest-posttest design was used in this study. The participants were 70 postpartum mothers who were admitted to a postpartum care center and experienced breast engorgement following cesarean birth. The planned nursing intervention was the breastfeeding promotion program consisting of breast massage and 1:1 breastfeeding education, counseling, and support focusing on individualized problem solving provided for 10 days. Fifty-three women completed the program (experimental group 26, control group, 27). Measurements were level of breast discomfort, breast size, sodium in breast milk and type of feeding at pre and posttest.
Figures and Tables
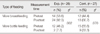
Table 2
Homogeneity Test for Participants' Characteristics between Experimental and Control Group (N=53)

References
1. World Health Organization. Infant and young child feeding: Model chapter for textbooks for medical students and allied health professionals. Geneva, CH: World Health Organization;2009.
2. Thulier D, Mercer J. Variables associated with breastfeeding duration. J Obstet Gynecol Neonatal Nurs. 2009; 38(3):259–268. http://dx.doi.org/10.1111/j.1552-6909.2009.01021.x.
3. Kim SK, Kim YK, Kim HR, Park JS, Son CK, Choi Y, et al. Report No.: Research Paper 2012-54. The 2012 national survey on fertility, family health & welfare in Korea. Seoul: Korea Institute for Health and Social Affairs;2012. 12.
4. Jang GJ, Kim SH. Effects of breast-feeding education and support services on breast-feeding rates and infant's growth. J Korean Acad Nurs. 2010; 40(2):277–286. http://dx.doi.org/10.4040/jkan.2010.40.2.277.
5. Lee SO, Chung ES, Ahn SH, Moon GN, Park NH. A study of predictors of breastfeeding. Korean J Child Health Nurs. 2003; 9(4):368–375.
6. Eum GR, Sohn HS, Kim HY. Breastfeeding rate and related factors in Busan. J Korean Soc Matern Child Health. 2007; 11(1):78–85.
7. Zanardo V, Svegliado G, Cavallin F, Giustardi A, Cosmi E, Litta P, et al. Elective cesarean delivery: Does it have a negative effect on breastfeeding? Birth. 2010; 37(4):275–279. http://dx.doi.org/10.1111/j.1523-536X.2010.00421.x.
8. Evans KC, Evans RG, Royal R, Esterman AJ, James SL. Effect of caesarean section on breast milk transfer to the normal term newborn over the first week of life. Arch Dis Child Fetal Neonatal Ed. 2003; 88(5):F380–F382.
9. Shawky S, Abalkhail BA. Maternal factors associated with the duration of breast feeding in Jeddah, Saudi Arabia. Paediatr Perinat Epidemiol. 2003; 17(1):91–96.
10. Cakmak H, Kuguoglu S. Comparison of the breastfeeding patterns of mothers who delivered their babies per vagina and via cesarean section: An observational study using the LATCH breastfeeding charting system. Int J Nurs Stud. 2007; 44(7):1128–1137. http://dx.doi.org/10.1016/j.ijnurstu.2006.04.018.
11. Mass S. Breast pain: Engorgement, nipple pain and mastitis. Clin Obstet Gynecol. 2004; 47(3):676–682.
12. Cho J, Ahn HY, Ahn S, Lee MS, Hur MH. Effects of oketani breast massage on breast pain, the breast milk pH of mothers, and the sucking speed of neonates. Korean J Women Health Nurs. 2012; 18(2):149–158. http://dx.doi.org/10.4069/kjwhn.2012.18.2.149.
13. Kim EK. Physiology of lactation. Hanyang Med Rev. 2010; 30(1):1–7. http://dx.doi.org/10.7599/hmr.2010.30.1.1.
14. Neville MC, Morton J, Umemura S. Lactogenesis. The transition from pregnancy to lactation. Pediatr Clin North Am. 2001; 48(1):35–52.
15. Hsien CF, Fu JC, Long CY, Lin HS. Factors influencing breast symptoms in breastfeeding women after cesarean section delivery. Asian Nurs Res. 2011; 5(2):88–98.
16. Neville MC. Introduction: Tight junctions and secretory activation in the mammary gland. J Mammary Gland Biol Neoplasia. 2009; 14(3):269–270. http://dx.doi.org/10.1007/s10911-009-9150-8.
17. Oketani Lactation Management Association. Oketani lactation management: Japanese breast massage manual. Tokyo, JP: Oketani Lactation Management Association;2004.
18. Morton JA. The clinical usefulness of breast milk sodium in the assessment of lactogenesis. Pediatrics. 1994; 93(5):802–806.
19. Humenick SS, Hill PD, Thompson J, Hart AM. Breast-milk sodium as a predictor of breastfeeding patterns. Can J Nurs Res. 1998; 30(3):67–81.
20. Becker GE, Cooney F, Smith HA. Methods of milk expression for lactating women. Cochrane Database Syst Rev. 2011; 12:CD006170. http://dx.doi.org/10.1002/14651858.CD006170.pub3.
21. Ahn S, Kim J, Cho J. Effects of breast massage on breast pain, breast-milk sodium, and newborn suckling in early postpartum mothers. J Korean Acad Nurs. 2011; 41(4):451–459. http://dx.doi.org/10.4040/jkan.2011.41.4.451.
22. Lee JA, So JS, Kim MJ, Na HN, Kim MH, Seo MS, et al. Reduction for incidence rate of breast engorgement in women with cesarean birth. In : The 2010 Fall Conference of the Korean Society of Quality Assurance in Health Care; 2008 December 4-5; BEXCO Convention Hall. Busan: The Korean Society of Quality Assurance in Health Care;2008. p. 106–108.
23. Yun SE, Lee HK. Effects of breast-feeding adaptation, attitude and practice of primipara depending on method of postpartum breast-feeding education. Korean J Women Health Nurs. 2012; 18(2):75–84. http://dx.doi.org/10.4069/kjwhn.2012.18.2.75.
24. Park YR. The effects of the integrated breast-feeding education on the knowledge, the adhesiveness and the attitude on breast-feeding [master's thesis]. Incheon: Inha University;2005.
25. Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. Hillsdale, NJ: Lawrence Erlbaum Associates;1988.
26. Walker M. Breastfeeding and engorgement. Breastfeed Abstr. 2000; 20(2):11–12.
27. Jung SH. The change of breast engorgement for non-breast feeding mother after cold cabbage compress [master's thesis]. Gwangju: Chonnam National University;2004.
28. Furman L, Minich N, Hack M. Correlates of lactation in mothers of very low birth weight infants. Pediatrics. 2002; 109(4):e57.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download