Abstract
Purpose
The purpose of this study was to examine effects of the Permission, Limited Information, Specific Suggestions, Intensive Therapy (PLISSIT) model sexual health enhancement program on, and development in, sexual function, sexual distress, marital intimacy, and subjective happiness of women with gynecologic cancer and their husbands.
Methods
The comprehensive program (4 session, 90 minutes per session) was developed based on the PLISSIT model. Participants were 43 couples, 21 assigned to the experimental group who attended the 4-week program, and 22 to the control group. Sexual function, sexual distress, marital intimacy, subjective happiness of the women, marital intimacy, subjective happiness of husbands were determined by a questionnaire that was completed by the participants before and after the program. The control group received the intervention post experiment. Chi-square test, t-test, Fisher's exact test were used to test the effectiveness of the program.
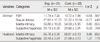
Figures and Tables
References
1. Anderson B, Anderson JE, Yi MY. Stretching. Seoul: Nexusbook;2001.
2. Annon JS. Behavioural treatment of sexual problems: Brief therapy. Hagerstown, MD: Joanna Cotler Books;1977.
3. Brotto LA, Heiman JR, Goff B, Greer B, Lentz GM, Swisher E, et al. A psychoeducational intervention for sexual dysfunction in women with gynecologic cancer. Arch Sex Behav. 2008; 37(2):317–329. http://dx.doi.org/10.1007/s10508-007-9196-x.
4. Chun N. A structural equation model on sexual function in women with gynecologic cancer. J Korean Acad Nurs. 2008; 38(5):639–648. http://dx.doi.org/10.4040/jkan.2008.38.5.639.
5. Chun N. Effectiveness of PLISSIT model sexual program on female sexual function for women with gynecologic cancer. J Korean Acad Nurs. 2011; 41(4):471–480. http://dx.doi.org/10.4040/jkan.2011.41.4.471.
6. Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. Hillsdale, NJ: Lawrence Erlbaum Associates;1988.
7. Derogatis LR, Rosen R, Leiblum S, Burnett A, Heiman J. The female sexual distress scale (FSDS): Initial validation of a standardized scale for assessment of sexually related personal distress in women. J Sex Marital Ther. 2002; 28(4):317–330.
8. Faul F, Erdfelder E, Lang AG, Buchner A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007; 39(2):175–191.
9. Han C, Kim HC, Kang SH, Moon DG, Kim JJ, Choi JY. Validity and reliability of Korean version of the female sexual distress scale (FSDS). Korean J Androl. 2004; 22(2):68–74.
10. Jensen PT, Groenvold M, Klee MC, Thranov I, Petersen MA, Machin D. Longitudinal study of sexual function and vaginal changes after radiotherapy for cervical cancer. Int J Radiat Oncol Biol Phys. 2003; 56(4):937–949.
11. Juraskova I, Butow P, Robertson R, Sharpe L, McLeod C, Hacker N. Post-treatment sexual adjustment following cervical and endometrial cancer: A qualitative insight. Psychooncology. 2003; 12(3):267–279. http://dx.doi.org/10.1002/pon.639.
12. Kalaitzi C, Papadopoulos VP, Michas K, Vlasis K, Skandalakis P, Filippou D. Combined brief psychosexual intervention after mastectomy: Effects on sexuality, body image, and psychological well-being. J Surg Oncol. 2007; 96(3):235–240. http://dx.doi.org/10.1002/jso.20811.
13. Katz A. Breaking the silence on cancer and sexuality: A handbook for healthcare providers. Pittsburgh, PA: Oncology Nursing Society;2007.
14. Katz A. Woman cancer sex. Pittsburgh, PA: Hygeia Media;2009.
15. King IM. A theory for nursing: Systems, concepts, process. New York, NY: Wiley;1981.
16. Laumann EO, Paik A, Glasser DB, Kang JH, Wang T, Levinson B, et al. A cross-national study of subjective sexual well-being among older women and men: Findings from the global study of sexual attitudes and behaviors. Arch Sex Behav. 2006; 35(2):145–161. http://dx.doi.org/10.1007/s10508-005-9005-3.
17. Lee KH. A measure of marital intimacy. J Korean Home Econ Assoc. 1995; 33(4):235–249.
18. Lim JS. The relationships of a self-enhancement bias, life events and subjective well-being in old-adults. Seoul: Ewha Womans University;2004. Unpublished master's thesis.
19. Lyubomirsky S, Lepper HS. A measure of subjective happiness: Preliminary reliability and construct validation. Soc Indic Res. 1999; 46(2):137–155.
20. Manne S, Sherman M, Ross S, Ostroff J, Heyman RE, Fox K. Couples' support-related communication, psychological distress, and relationship satisfaction among women with early stagebreast cancer. J Consult Clin Psychol. 2004; 72(4):660–670. http://dx.doi.org/10.1037/0022-006x.72.4.660.
21. Masters WH, Johnson VE. Human sexual inadequacy. Boston, MA: Little, Brown;1970.
22. Nho JH, Park YS. Descriptive study on sexuality for women with gynecological cancer. Korean J Women Health Nurs. 2012; 18(1):17–27. http://dx.doi.org/10.4069/kjwhn.2012.18.1.17.
23. Park JS, Lee YE. Effects of integrated menopause management program for middle aged woman. Korean J Women Health Nurs. 2011; 17(1):10–20. http://dx.doi.org/10.4069/kjwhn.2011.17.1.10.
24. Park YS, Cho IS, Kim YM. A survey of urban middle-aged women's sexual function and sexual distress. Korean J Women Health Nurs. 2007; 13(4):254–261.
25. Rivalta M, Sighinolfi MC, De Stefani S, Micali S, Mofferdin A, Grande M, et al. Biofeedback, electrical stimulation, pelvic floor muscle exercises, and vaginal cones: A combined rehabilitative approach for sexual dysfunction associated with urinary incontinence. J Sex Med. 2009; 6(6):1674–1677. http://dx.doi.org/10.1111/j.1743-6109.2009.01238.x.
26. Rosen R, Brown C, Heiman J, Leiblum S, Meston C, Shabsigh R, et al. The female sexual function index (FSFI): A multidimensional self-report instrument for the assessment of female sexual function. J Sex Marital Ther. 2000; 26(2):191–208. http://dx.doi.org/10.1080/009262300278597.
27. Scott JL, Halford WK, Ward BG. United we stand? The effects of a couple-coping intervention on adjustment to early stage breast or gynecological cancer. J Consult Clin Psychol. 2004; 72(6):1122–1135. http://dx.doi.org/10.1037/0022-006x.72.6.1122.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download