Abstract
Purpose
The purpose of this study was to compare the effect of alcohol gel according to the amount and drying time in health personnel hand hygiene and to promote in their practice adequate and effective hand hygiene.
Methods
The cross-over experimental study was performed with 14 volunteers. Hands were artificially contaminated with 5 mL of 108 CFU/mL of Serratia marcescens (ATCC 14756) and four different alcohol gel hand hygiene methods varying by the amount of alcohol gel (2 mL vs. 1 mL) and drying time (complete vs. incomplete) were compared. Samples were collected by glove juice sampling procedures.
Results
Mean log reduction values of the four different hand hygiene methods were 2.22±0.36, 1.26±0.53, 1.49±0.60, 0.89±0.47 respectively for the 4 groups: adequate amount (2mL) and complete dry (30 seconds rubbing followed by 2 min air-dry), inadequate amount (1 mL) and complete dry, adequate amount and incomplete dry (15 seconds rubbing and no air-dry), and inadequate amount and incomplete dry. The difference was statistically significant in the adequate amount and complete dry group compared to other three groups (p<.001).
Figures and Tables
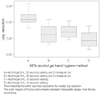 | Figure 2Box and whisker plots of antimicrobial effect of four types 62% alcohols gel hand hygiene methods. |
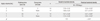
Table 1
Baseline and Residual Bacterial Density among Four Types of 62% Alcohol Gel Hand Hygiene Method
References
1. Ahn MJ. Handwashing related factors of handwashing practice by nursing personal in crictical care unit. Seoul: Yonsei University;2002. Unpublished master's thesis.
2. Boyce JM, Pittet D. Guideline for hand hygiene in health-care settings: Recommendations of the healthcare infection control practices advisory committee and the HICPAC/SHEA/APIC/IDSA hand hygiene task force. Infect Control Hosp Epidemiol. 2002; 23:12 Suppl. S3–S40. http://dx.doi.org/10.1086/503164.
3. Dharan S, Hugonnet S, Sax H, Pittet D. Comparison of waterless hand antisepsis agents at short application times: Raising the flag of concern. Infect Control Hosp Epidemiol. 2003; 24(3):160–164. http://dx.doi.org/10.1086/502182.
4. Garner JS. Guideline for isolation precautions in hospitals. The hospital infection control practices advisory committee. Infect Control Hosp Epidemiol. 1996; 17(1):53–80.
5. Guilhermetti M, Marques Wiirzler LA, Castanheira Facio B, da Silva Furlan M, Campo Meschial W, Bronharo Tognim MC, et al. Antimicrobial efficacy of alcohol-based hand gels. J Hosp Infect. 2010; 74(3):219–224. http://dx.doi.org/10.1016/j.jhin.2009.09.019.
6. Han MJ. The effect of an educational handwashing program on the handwashing compliance. Cheonan: Dankook University;2003. Unpublished master's thesis.
7. Jeong JS, Choe MA. The effect of hand washing improving programs on the adherence of hand washing and nosocomial infections in a surgical intensive care unit. Korean J Nosocomial Infect Control. 2004; 9(2):117–129.
8. Jeong JS, Kim DH, Kim MN, Choe MA. Bactericidal effect of waterless alcohol gel hand washing agent. J Korean Biol Nurs Sci. 2002; 4(2):127–137.
9. Ju HL, Sim JS, Kim MN, Park KO. A comparison of antimicrobialeffect of two waterless alcohol-based hand rubs with a povidone-iodine hand scrub for surgical hand antisepsis. J Korean Clin Nurs Res. 2009; 15(1):55–65.
10. Kampf G. How effective are hand antiseptics for the postcontamination treatment of hands when used as recommended? Am J Infect Control. 2008; 36(5):356–360. http://dx.doi.org/10.1016/j.ajic.2007.07.017.
11. Kampf G, Ostermeyer C. Efficacy of alcohol-based gels compared with simple hand wash and hygienic hand disinfection. J Hosp Infect. 2004; 56:Suppl 2. S13–S15. http://dx.doi.org/10.1016/j.jhin.2003.12.026.
12. Kang MW. National survey and development of standardized practice on the infection control in Korea. Gwacheon: Ministry of Health and Welfare;2004.
13. Kramer A, Rudolph P, Kampf G, Pittet D. Limited efficacy of alcohol-based hand gels. Lancet. 2002; 359(9316):1489–1490. http://dx.doi.org/10.1016/s0140-6736(02)08426-x.
14. Larson EL, Eke PI, Wilder MP, Laughon BE. Quantity of soap as a variable in handwashing. Infect Control. 1987; 8(9):371–375.
15. Larson EL, Strom MS, Evans CA. Analysis of three variables in sampling solutions used to assay bacteria of hands: Type of solution, use of antiseptic neutralizers, and solution temperature. J Clin Microbiol. 1980; 12(3):355–360.
16. Laustsen S, Lund E, Bibby BM, Kristensen B, Thulstrup AM, Kjølseth Møller J. Effect of correctly using alcohol-based hand rub in a clinical setting. Infect Control Hosp Epidemiol. 2008; 29(10):954–956. http://dx.doi.org/10.1086/590393.
17. Lim OB. Effect of education and feedback on the frequency and quality of hand hygiene. Ulsan: University of Ulsan;2004. Unpublished master's thesis.
18. Park ES, Jeong JS, Kim KM, Kim OS, Jeong SY, Jang SY, et al. Descriptive study on the current Usage of disinfectants in Korea. Korean J Nosocomial Infect Control. 2006; 11(1):42–49.
19. Pittet D. Improving adherence to hand hygiene practice: A multidisciplinary approach. Emerg Infect Dis. 2001; 7(2):234–240. http://dx.doi.org/10.3201/eid0702.700234.
20. Pittet D, Hugonnet S, Harbarth S, Mourouga P, Sauvan V, Touveneau S, et al. Effectiveness of a hospital-wide programme to improve compliance with hand hygiene. Infection Control Programme. Lancet. 2000; 356(9238):1307–1312.
21. Tvedt C, Bukholm G. Alcohol-based hand disinfection: A more robust hand-hygiene method in an intensive care unit. J Hosp Infect. 2005; 59(3):229–234. http://dx.doi.org/10.1016/j.jhin.2004.10.003.
22. Widmer AE, Dangel M. Alcohol-based handrub: Evaluation of technique and microbiological efficacy with international infection control professionals. Infect Control Hosp Epidemiol. 2004; 25(3):207–209. http://dx.doi.org/10.1086/502379.
23. World Health Organization. WHO guidelines on hand hygiene in health care. Switzerland: World Health Organization;2009.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download