Abstract
Purpose
The purpose of this study was to investigate the contribution of actual cardiovascular disease (CVD) risk, as well as, individual, psychosocial, and work-related factors as predictors of CVD risk perception among Korean blue-collar workers.
Methods
The participants were 238 Korean blue-collar workers who worked in small companies. Data were collected through a survey; anthropometric and blood pressure measures; and blood sampling for lipid levels.
Results
Blue-collar workers had high actual CVD risk and low CVD risk perception. The significant predictors of risk perception included perceived health status, alcohol consumption, knowledge of CVD risk, actual CVD risk, decision latitude, and shift work. The model explained 26% of the variance in CVD risk perception.
Conclusion
The result suggests when occupational health nurses are giving routine health examination in small companies, they can enhance CVD risk perception in blue-collar workers by providing essential information about CVD risk factors and personal counseling on the individual worker's CVD risk status.
Cardiovascular Disease (CVD) is the second cause of death in Korean workers (Korea National Statistical Office [KNSO], 2010). Healthcare costs for CVD doubled between 2000 and 2005 in Asian Pacific countries (World Health Organization [WHO], 2008). Specifically, in Korea, CVD has become recognized as a compensable work-related disease and has, therefore, resulted in a dramatic increase in worker's compensation for CVD caused by overwork. Escalating health care costs for work-related compensation reached $352 billion in 2010, 1.75% increase compared to that of 2009 and is estimated to reach $1,761 billion including direct and indirect economic cost (Korea Occupational Safety and Health Agency [KOSHA], 2010).
Blue-collar workers, particularly those in small companies having 300 or fewer employees, are vulnerable to CVD risks because health promotion program more focused on large companies than such small companies. Also, occupational health nurses are only available to larger companies, although the occupational health center (OHC) has responsibility for the aggregated workers' health check-ups in small companies (Hwang, 2011; June, Hong, & Cho, 2003).
Individuals' perception of their own risk for CVD had been found to be a primary risk factor for eventually becoming inflicted with CVD. According to the health belief model, perceived risk is an important precursor in engaging risk reduction behaviors (Janz & Becker, 1984). Most people, however, do not accurately perceive their risk for CVD and, most often underestimate the likelihood that they will suffer from CVD. This is particularly true among Korean blue-collar workers. It is important that health educators, as well as those in the occupational health field, understand workers' perceptions of risk for developing CVD. Measuring perceived risk, and understanding the implications of those measurements, is a critical piece in the development and implementation of appropriately targeted interventions for assisting Korean blue-collar workers to accurately identify CVD risk and make achievable lifestyle changes to lower CVD risk. The major goal of this research was to investigate variables that increase or decrease accurate risk perception and, eventually, use those variables that increase accurate risk perception to develop methods to reduce the incidence and prevalence of CVD among Korean blue-collar workers.
CVD actual risk was defined as the absolute risk of having a CVD event in 10 years. Actual 10-year risk can be calculated using objective data, such as blood pressure (BP), cholesterol, and the presence of left ventricular hypertrophy (LVH) (Frijling et al., 2004). Risk perception of CVD is defined as how a person perceives the likelihood of having a CVD event within the next ten years (Frijling et al.).
Numerous factors have been identified that influence CVD risk perception. First, risk perception has been found to be influenced by actual risk. Actual risk is oftentimes measured by the existence of common comorbidities or preexisting conditions, such as MI (myocardial infarction), hypertension, ischemic heart disease, and stroke. Several studies have reported that family history of MI and hypertension significantly increased personal risk perceptions of CVD (Choi, Rankin, Stewart, & Oka, 2008; Frijling et al., 2004). Some studies, however, noted that a personal history of MI did not increase perception of risk (Meischke et al., 2002; van der Weijden, van Steenkiste, Stoffers, Timmermans, & Grol, 2007). A German study found that positive family history for CVD was not determinants of perceived high risk, although patients with diabetes and family history of CVD have, by definition, a high actual risk (van der Weijden et al. 2007). Smoking, obesity, and hypertension were determinants of perceiving CVD risk as high, while diabetic patients surprisingly did not report high perceived CVD risk. Men were more likely than women to incorrectly perceive their CVD risk as low (van der Weijden et al.). The results contrast with those of other studies (Frijling et al.; Jones, Weaver, & Friedmann, 2007).
Second, risk perception is known to be primarily determined by emotions rather than facts. Frijling et al. (2004) did not, however, collect patients' psychological factors and suggested investigation into the influence of perceived stress, anxiety, depression, quality of life, and social support because people's emotional response to the risk of having disease may play an important role in people's motivation to engage in risk reduction behaviors.
Third, knowledge of CVD risk factors (Choi et al., 2008) and perceived health status (Oliver-Mcneil & Artinian, 2002) influence CVD risk perception. More knowledge of CVD and poorer health status were associated with higher CVD risk perception (Choi et al.). Communicating the results and implication of health risk appraisal could effectively change the perception of those at high risk (Meischke et al., 2002).
Fourth, literature review also suggests that demographic characteristics such as age, gender, level of education, and income are associated with perceived risk of CVD (Christian, Mochari, & Mosca, 2005; Frijling et al.; Jones et al., 2007; van der Weijden et al., 2007). However, work-related factors such as shift work, decision latitude, and social support in workplace have not been included to the previous risk perception studies, although those factors were found to be relevant to the work-related CVD risk factors (Hwang & Hong, 2012).
In summary, the literature provides inconsistent findings on the association between CVD risk perception and influencing factors. There was no study that has considered the relationship between CVD risk perception, the working environment, psychosocial factors, and actual risk for CVD among blue-collar workers. Research addressing this gap would provide a better understanding of CVD risks in the work environment. The purpose of this study was to examine the relationships between actual CVD risks, individual, psychosocial, and work-related factors and CVD risk perception among blue-collar workers employed at small companies in Korea.
A cross-sectional survey was implemented, along with blood testing, anthropometric measuring, and blood pressure readings.
The target population for this study was skilled or non-skilled manual workers based on the Korean standard classification of occupations (KNSO, 2007). Recruitment took place at eight different worksites during the OHC's annual prevention program. These eight worksites are small companies who do not have their own in house occupational health professional to provide annual physical examinations and occupational injury prevention programs for their employees. Study participants met inclusion criteria if they were above 18 years of age and had no history of MI, percutaneous transluminal coronary angioplasty, or cognitive impairment.
Two hundred fifty workers who met the study criteria were asked to participate in the study. Two hundred forty workers agreed to participate in the study. The common reason for not enrolling was lack of time to finish questionnaires and blood testing. Data from two participants were deleted from the analysis because they missed over 50% of the questions in the survey. Thus, the final sample for the analysis was 238 participants.
Data collection was preformed over the course of two months, from June to July of 2010. Data collection was comprised of three approaches. First, a survey was completed by all participants. The survey consisted of three quantitative measures; Job Contents Questionnaire (JCQ), Knowledge of CVD Risk, and Risk Perception Questionnaire. Socio-demographics and CVD risk factors questionnaires were modified for this study. The first three instruments had been previously translated into Korean and validated with Korean workers and adults (Choi et al., 2008; Kang et al., 2005). The reliability and validity of instruments are described in the following section.
Second, data were collected on anthropometric measures of study participants. These measurements included weight and height, in order to assess body mass index. Weight was measured in kilograms using an automatic body-weight scale. Height was measured in centimeters to the top of the head using a non-stretching measuring tape secured to the wall. BP was measured twice, 2-minutes apart with an electronic BP monitor.
Third, blood tests were conducted to calculate actual CVD risk. However, LVH was checked through the most recent chest-X ray results of the individual record review. Blood sampling was obtained from the participants by a registered nurse. Samples were collected in two tubes, one with, and another without anticoagulants such as sodium citrate/EDTA. The analysis of the blood was performed by certified laboratories. Total serum cholesterol (TC) and high-density lipoprotein cholesterol (HDL) were measured. In triglycerides (TG) less than 400 mg/dL, low density lipoprotein cholesterol (LDL) were calculated using the Friedewald formula (LDL=TC-HDL-TG/5).
Perceived risk of CVD was assessed by the risk perception questionnaire developed and tested by Becker and Levine (1987) in a study of a high-risk group. The questionnaire is composed of four items that investigate a person's a) frequency of concern over having CVD, b) his or her estimate of the likelihood of having such an event in the next ten years, c) the likelihood of having such an event in his or her lifetime, and d) his or her estimated CVD risk compared with people of similar age and sex in the general population. Items 1-3 was assessed on a 5-point Likert scale. The response categories for the fourth item would be much less, less, about the same, more, and much more risk than people in the general population. Scores for the four items were summed up. A high score indicates a high level of perceived risk. This instrument has demonstrated good internal consistency with Cronbach's α of .78 in Korean immigrant sample (Choi et al., 2008). Cronbach's α was .86 for this study sample.
A KOSHA (Korea Occupational Safety and Health Agency) risk assessment (KOSHA, 2008) was used to calculate CVD actual risk based on WHO International Society of Hypertension guidelines (Whitworth, 2003). The CVD actual risk score was calculated by adding the following CVD risk factors: age ≥55 years in men or age ≥65 years in women, TC ≥240 mg/dl or LDL ≥160 mg/dl, smoking, HDL ≤35 mg/dl, family history of CVD, body mass index ≥30 kg/m2 or lack of physical activity, and the presence of LVH. The composite score (maximum: 7 points) for CVD risk was reduced by 1 point if HDL was ≥60 mg/dl. For physical activity, appropriate amount of exercise was defined as doing exercise 30 min/day for more than three days per week. A positive family history was defined as a report by participants of CVD in any of the subject's biological parents and siblings. In this study, the participants were categorized into normal and three risk groups (low, medium, and high) and then they were further stratified into two groups (high risk and non-high risk group). According to KOSHA risk management guideline stated in Table 1, non-high risk group included normal, low, and medium risk group.
Knowledge of CVD risk factors was assessed using a checklist with a single question. Participants were given a list of possible responses and asked to check the factors that they thought either caused, or were associated with CVD. Possible responses included smoking, consumption of fat or high serum cholesterol, high BP, family history of CVD, age, gender, sedentary lifestyle, stress, obesity, diabetes, chemical exposure, lead exposure, noise exposure, shift work, and overtime work. Each response was worth one point. Scores range from 0 to 15 points. A higher score is indicative of a higher level of CVD knowledge. This instrument was adopted from a similar method used in the study of high risk groups such as CVD parents and immigrants (Becker & Levine, 1987; Choi et al., 2008). Although it is not possible to determine internal consistency for this instrument because it is an index, the scale has face validity since all of the risk factors have been associated with CVD. It has been used in several studies and mean scores typically range from 6 to 8 (Becker & Levine; Choi et al.).
Health status was measured by asking the participant about his/her perceived health status on a 5-point scale (1=Excellent to 5=Poor). This single-item measure came from the Medical Outcomes Study 36-item short form survey developed by Ware and Sherbourne (1992). It has been demonstrated to be significant predictor of later health outcomes (Boustrom & Fredlund, 2001).
Social support was measured by JCQ, which consists of 22-items including psychological demands (n=5), skill discretion (n=6), decision authority (n=3), supervisor support (n=4), and coworker support (n=4). All of these scales were measured on a 4-point Likert-type scale (1=strongly agree, 4=strongly disagree). The total score of social support was determined by adding the scores of the two subscales of JCQ, supervisor support and coworker support. Eum and colleagues (2007) evaluated the Korean version of JCQ with 157 Korean healthcare workers. Cronbach's alpha coefficients were .87 for supervisor support and .77 for coworker support in the present study.
Decision latitude was also measured by JCQ. The score for decision latitude was obtained by adding the subscale scores of skill discretion and decision authority using the formulas recommended by Karasek et al. (1998). A high score represents a high level of perceived decision latitude over the job. The reported internal consistency of the instrument ranged from .73 to .81 for the decision latitude scale (Karasek et al.). The studies using Korean JCQ showed .87 (Kang et al., 2005), and .74 (Eum et al., 2007; Kang et al.). Cronbach's alpha for decision latitude was .76 in the current study.
Participants were asked to report whether they were exposed to noise or chemicals (carbon monoxide, carbon disulfide, lead, and solvents) at work. Participants also were asked whether they worked on shifts including night shift. All responses were in a yes/no format.
Alcohol consumption was measured by self-report of alcohol use. If a worker reported alcohol use, he/she was asked subsequent questions to assess the number of drinks of Soju and beer typically consumed over the course of one month. The number of standard servings of alcohol over the course of one month was estimated. For example, assuming that 1-2 drinks of Soju is equivalent to a single beer, 3-4 drinks of Soju is equivalent to 2 servings of beer. The two servings of beer or more per month was considered to be an alcohol consumer.
This study was approved by a university institutional review board in the U.S. and the health center's human rights review committee in Korea. A written informed consent was obtained from each participant. The purpose and protocol of the study was explained to the director of the OHC and administrators of the participating workplaces and their support was obtained for the recruitment of study participants.
Descriptive statistics (i.e., mean, standard deviation, percentage, and range) were used to describe the characteristics of participants and study variables. Scatter plots of each independent variable with each outcome variable was created to assess whether the associations are linear. Pearson correlations were done to examine associations between independent and dependent variables. Multivariate analysis was conducted using multiple linear regressions and included variables for which p<.20 in bivariate analyses.
Categorical variables with two levels were directly entered as predictor variables in a multiple regression model. Level of education was coded into 1=college or more and 0=less than high school. The dichotomous variable is coded as 1=exposure and 0=non exposure. First, the R2 of the complete model was examined for significance. Then, the unique contribution of each independent variable was tested to explain the variance in CVD risk perception. All analyses were performed using Statistical Package for the Social Science version 18.0 for Windows.
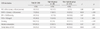
Table 2 shows the demographic and work characteristics of the participants. Over 60% (n=156) of the participants were male, and the mean age was 37 years (SD=8.5; range=19 to 58). Workers in the sample were predominantly regular employment status. The mean duration of work in the current job was 6.8 years (SD=5.4). Each participant worked for one of five manufacturing sectors: a) shipbuilding (38.2%); b) manufacture of print chips (19.8%); c) electronics (12.2%); d) weaponry (8.4%); and e) manufacture of butane gas (21.4%). Participants were economically lacking and had a low educational level. Approximately 62 % were married, more than one third (37%) did shift work, more than two thirds (77%) reported alcohol consumption, and about 46 % of the sample reported that they had been exposed to the combined exposure of chemicals and noise. The majority (82%) indicated that their health status was good, very good, or excellent. Only 18% reported fair and two participants reported poor health.
In responses to a question about frequency of concern about having a CVD event, more than half of the participants (56%) responded never and rarely. Around two thirds reported that the likelihood of their having a CVD event in the next 10 years and in their lifetime was answered as not likely. Over 60% indicated that their CVD risk was the same as or lower than people in the worker population of similar age and gender. The mean score for CVD risk perception was 9.36 (SD=4.31; median 8.0), indicating that the blue-collar workers had low CVD risk perception. The normal distribution of the score was showed (Skewness=.52, SE=.16).
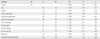
Based on the KOSHA CVD risk assessment classification (see Table 1); about 68% participants were in medium risk group. About 12 % was in the high risk group with more than three risk factors and third-degree hypertension. The prevalence of each component of CVD risk factors by KOSHA risk group was shown in Table 3. High KOSHA risk group was significantly associated with CVD risk factors such as waist circumference (t=3.96, p=.001) and waist hip ratio (t=16.5, p<.001). Among lipid level, high triglyceride level correlated with a higher KOSHA risk group (t=5.8, p<.016). The mean total CVD knowledge score was 8.34 (SD=4.5; range=0 to 15), indicating that participants had a moderate level of knowledge on CVD risk factors.
Multiple regression analyses showed the linear combination of the predictors was significantly related to CVD risk perception. The R2 was .26 (Adjusted R2=.22), indicating that the model explained about 26% of the variance in CVD risk perception, F (11, 226)=7.82, p<.001. Individual factors (CVD knowledge, alcohol consumption), psychosocial factors (perceived health status), actual CVD risk, and work-related factors (decision latitude and shift work) were significant predictors of CVD risk perception. People with higher level of CVD knowledge and better perceived health status showed lower levels of CVD risk perception. Higher decision latitude and alcohol consumption was related to an increase of CVD risk perception (Table 4).
The findings of the study support the hypothesis that CVD actual risk was associated with risk perception. Blue-collar workers had low perception of CVD risks and their actual risk was high (11.8%). Corresponding numbers using the same KOSHA CVD risk assessment, the medium-risk and high-risk groups were 6.9% and 5.7%, respectively, among male-workers (Kim & Kang, 2010). The present study suggests that CVD knowledge and perceived health status are important in determining CVD risk perception in this group.
Higher levels of actual risk of CVD based on the KOSHA CVD risk assessment, predicted risk perception of CVD. Blue-collar workers in the high CVD risk group perceived they were vulnerable and susceptible to CVD. Several studies that incorporated actual risk and perceived risk (Barnhart et al., 2009; Christian et al., 2005; Frijling et al., 2004; Homko et al., 2008) were identified. Of these, three studies used the Framingham 10-year risk score to measure actual risk of CVD (Christian et al.; Frijling et al.; Homko et al.). Christian et al. and Homko et al. did not find a similar association, however, Barnhart et al. and Frijling et al. showed an association between CVD risk and CVD risk perception. The finding of this study concurs with those of Barnhart et al. and Frijling et al. Feedback on actual risk has been found to improve risk perception (Frijling et al.). Based on these findings, any strategy of occupational health nurse to prevent the risk of CVD in small companies should begin with a discussion about CVD's severity and a worker's susceptibility to the disease.
Knowledge of CVD risk is one method to improve awareness of actual CVD risk, thereby, theoretically, improving the accuracy of risk perception. In this study, we found a positive association between CVD knowledge and risk perception among participants. This is consistent with other study findings (Choi et al., 2008; Homko et al., 2008; Jones et al., 2007; Meischke et al., 2002). Therefore, lack of CVD knowledge may contribute to low level of risk perception. It has been suggested that occupational health nurses' informing workers about occupational risk factors for CVD draws more attention to worksite risk, heightening workers' risk perception of CVD. Educational programs on work-related risk factors for CVD, designed for blue-collar workers, should be part of a worksite intervention program. This finding and its implications have not been supported in all studies on the subject. Several studies have shown no relationship between CVD knowledge and risk perception (Becker & Levine, 1987; Oliver-Mcneil & Artinian, 2002).
Perceived health status was found to be strongly associated with CVD risk perception, as has been shown in previous studies (Frijling et al., 2004; Meischke et al., 2002). These results suggest that blue-collar workers who report their health status to be good feel less vulnerable to having any diseases, including CVD. Further studies need to investigate effective ways to communicate CVD risk to blue-collar workers so that these persons understand their risk of CVD and adopt health promotion behaviors.
Decision latitude, a work-related factor, was found to be a predictor of overall risk perception. Few studies have been performed on the relationship between work-related factors and risk perception of CVD. Many studies have shown that job stress affects actual CVD, such as coronary heart disease and stroke (Xu, Zhao, Guo, Guo, & Gao, 2009). Furthermore, decision latitude has been shown to be significantly associated with CVD among health care workers and industrial workers (Kang et al., 2005). Workers with low decision latitude may feel more vulnerable about their health or be more aware of the negative aspects of their working conditions, leading to perceptions of an increased risk of CVD. However, decision latitude was positively associated with risk perception of CVD in this study, indicating that high decision latitude increased risk perception of CVD. Further research is needed to support these findings and interpretations.
Shift work was noted to be negatively related to CVD risk perception in Korean blue-collar workers. In other words, shift workers reported less risk perception of CVD than non-shift workers. Shift work is well-known to be a significant risk factor for CVD in Asian countries and in the United States (Hwang & Hong, 2012; Kim & Kang, 2010), but its relationship with the risk perception has not been studied. Only 40% of participants in this study correctly answered that shift work is a risk factor for CVD. The finding that blue-collar workers who are currently involved in shift work are not aware of their risk of CVD is important. These results are particularly telling because they were obtained even after potential controlling for confounding factors. These factors included not only individual factors but also psychosocial work conditions (i.e., job stress and social support).
However, among psychosocial factors, social support was not found to influence on CVD risk perception. This finding is contrast to other studies, which have reported an association between social support and CVD risk (Fan, Blumenthal, Hinderliter, & Sherwood, 2012; Hwang & Hong, 2012). In this study, we measured only coworker and supervisor support related to CVD risk perception, which are different from network support and actual CVD risk, respectively. Future studies comparing the social support including network support with CVD risk perception may explain the difference found in the present study.
Another significant predictor of CVD risk perception in Korean blue-collar workers was alcohol consumption. To the authors' knowledge, no studies have investigated the relationship between risk perception and alcohol consumption. Conversely, many studies have found that alcohol consumption clearly affects the risk of CVD (Leon, Shkolnikov, McKee, Kiryanov, & Andreev, 2010). Thus, an increase in perceived risk accompanying increased alcohol use may reflect an appropriate awareness of this risk of CVD. The precise mechanism linking alcohol to the risk of CVD, however, remains unclear (Leon et al., 2010). More than half of the participants in this study drank alcohol. Although it appears that workers drink alcohol with the understanding that it increases their risk for CVD, Hwang and Lee (2005) found that workers did not stop or reduce alcohol consumption. Continuation of alcohol consumption, even with the knowledge of CVD risk is likely due to the fact that drinking is a common social activity in Korean society, especially among colleagues.
This study, however, has several limitations. First, the study used a convenience sample of blue-collar workers from small companies with less than 300 employees. Also, the sample was recruited from only .002% of total small companies in Korea. The results may not be generalized beyond the study participants. Second, the instruments to measure CVD risk perception and knowledge were limited to awareness of risk factors and, thus, they may not have totally reflected the workers' understanding of CVD risk. Culturally appropriate measures specific to the working population may need to be developed. The norms, beliefs, values, expectations, linguistic appropriateness, and reading comprehension levels among this study population should be considered more thoroughly in similar future studies. Finally, dose-response relationship between chemical and noise exposure levels and risk perception were not included, although we adjusted for all possible confounders mentioned earlier.
Risk perception of CVD has been identified as one of critical factor influencing behavior change. Study findings suggest that blue-collar workers at small companies are likely to underestimate their risks for CVD. This provides a unique opportunity for occupational health nurses, to develop and implement interventions that will affect risk perception by improving understanding of actual risk, CVD knowledge, and the risks of shift work. Many actions have been taken in workplaces with medium- and large-scaled, according to the regulation (Kim & Kang, 2010). Education and information need to be provided to small companies where shift workers are in place and many cases of CVD have occurred. Moreover, nurses in occupational setting should be active in advising blue-collar workers at small companies to change unhealthy lifestyle like heavy alcohol consumption.
It is possible that the identified links between work-related factors and CVD risk perception may occur among other occupational groups such as white-collar workers. Further research is needed to validate the findings of this relationship with different occupational groups.
Korean blue-collar workers participating in this study were, primarily, at moderate risk for CVD. The majority had limited CVD knowledge and had an inaccurately low level of perceived risk for CVD. Predictors of CVD risk perception included actual risk, CVD knowledge, perceived health status, and alcohol consumption. In addition, work-related factors such as decision latitude and shift work had an important contribution to risk perception.
The results of the present study fill an important gap in the research examining the relationship between CVD risk perception and work related factors, particularly among blue-collar workers employed at small companies. Currently in Korea, all blue-collar workers are required to undergo the KOSHA CVD risk assessment. Any workers who are considered at high risk, is required to have a follow-up and health promotion program according to the regulation. However, occupational professionals are not enough available to follow up workers at small companies due to no onsite occupational health nurses at small companies. Although this shows an effort to combat the issue of CVD incidence and prevalence among this population, more of opportunities by onsite occupation health nurses need to be made on primary prevention, as opposed to tertiary prevention, at small companies.
Figures and Tables
Table 1
KOSHA CVD Risk Assessment Classification Criteria and Risk Group
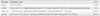
Source: KOSHA (Korea Occupational Safety and Health Agency) Code H-46-2008(KOSHA, 2008); CVD=Cardiovascular disease.
KOSHA CVD risk factors; age≥55 years in men or age≥65 years in women, total cholesterol≥240 mg/dL or LDL≥160 mg/dL, smoking, HDL≤35 mg/dL, family history of CVD,
Body Mass Index≥30 kg/m2or lack of physical activity, and the presence of LVH.
Notes
References
1. Barnhart JM, Wright ND, Freeman K, Silagy F, Correa N, Walker EA. Risk perception and its association with cardiac risk and health behaviors among urban minority adults: The Bronx CoronaryRisk Perception study. Am J Health Promot. 2009. 23:339–342. http://dx.doi.org/10.4278/ajhp.07072574.
2. Becker DM, Levine DM. Risk perception, knowledge, and lifestyles in siblings of people with premature coronary disease. Am J Prev Med. 1987. 3:45–50.
3. Burström B, Fredlund P. Self rated health: Is it as good as a predictor of subsequent mortality among adults in lower as well as in higher social classes? J Epidemiol Community Health. 2001. 55:836–840. http://dx.doi.org/10.1136/jech.55.11.836.
4. Choi S, Rankin S, Stewart A, Oka R. Perceptions of coronary heart disease risk in Korean immigrants with type 2 diabetes. Diabetes Educ. 2008. 34:484–492. http://dx.doi.org/10.1177/0145721708316949.
5. Christian AH, Mochari HY, Mosca LJ. Coronary heart disease in ethnically diverse women: Risk perception and communication. Mayo Clin Proc. 2005. 80:1593–1599. http://dx.doi.org/10.4065/80.12.1593.
6. Eum KD, Li J, Jhun HJ, Park JT, Tak SW, Karasek R, et al. Psychometric properties of the Korean version of the job content questionnaire: Data from health care workers. Int Arch Occup Environ Health. 2007. 80:497–504. http://dx.doi.org/10.1007/s00420-006-0156-x.
7. Fan LB, Blumenthal JA, Hinderliter AL, Sherwood A. The effect of job strain on nighttime blood pressure dipping among men and women with high blood pressure. Scand J Work Environ Health. 2013. 39:112–119. http://dx.doi.org/10.5271/sjweh.3294.
8. Frijling BD, Lobo CM, Keus IM, Jenks KM, Akkermans RP, Hulscher ME, et al. Perceptions of cardiovascular risk among patients with hypertension or diabetes. Patient Educ Couns. 2004. 52:47–53. http://dx.doi.org/10.1016/S0738-3991(02)00248-3.
9. Homko CJ, Santamore WP, Zamora L, Shirk G, Gaughan J, Cross R, et al. Cardiovascular disease knowledge and risk perception among underserved individuals at increased risk of cardiovascular disease. J Cardiovasc Nurs. 2008. 23:332–337.
10. Hwang WJ. Philosophical and ethical perspectives on cardiovascular disease risk in low-wage workers. Public Health Nurs. 2011. 28:168–175. http://dx.doi.org/10.1111/j.1525-1446.2010.00922.x.
11. Hwang WJ, Hong O. Work-related cardiovascular disease risk factors using a socioecological approach: Implications for practice and research. Eur J Cardiovasc Nurs. 2012. 11:114–126. http://dx.doi.org/10.1177/1474515111430890.
12. Hwang SY, Lee JH. Comparison of cardiovascular risk profile clusters among industrial workers. J Korean Acad Nurs. 2005. 35:1500–1507.
13. Janz NK, Becker MH. The health belief model: A decade later. Health Educ Q. 1984. 11:1–47.
14. Jones DE, Weaver MT, Friedmann E. Promoting heart health in women: A workplace intervention to improve knowledge and perceptions of susceptibility to heart disease. AAOHN J. 2007. 55:271–276.
15. June KJ, Hong O, Cho TR. Occupational health nursing practice, education, and research in Korea. An international update. AAOHN J. 2003. 51:65–71.
16. Kang MG, Koh SB, Cha BS, Park JK, Baik SK, Chang SJ. Job stress and cardiovascular risk factors in male workers. Prev Med. 2005. 40:583–588. http://dx.doi.org/10.1016/j.ypmed.2004.07.018.
17. Karasek R, Brisson C, Kawakami N, Houtman I, Bongers P, Amick B. The Job Content Questionnaire (JCQ): An instrument for internationally comparative assessments of psychosocial job characteristics. J Occup Health Psychol. 1998. 3:322–355. http://dx.doi.org/10.1037/1076-8998.3.4.322.
18. Kim DS, Kang SK. Work-related cerebro-cardiovascular diseases in Korea. J Korean Med Sci. 2010. 25:Suppl. S105–S111. http://dx.doi.org/10.3346/jkms.2010.25.S.S105.
19. Korea National Statistical Office. Korean standard industrial classification. 2007. Retrieved April 24, 2010. from http://kostat.go.kr/kssc/board_notice/BoardAction.do?method=list&board_id=11&catgrp=kssc&catid1=kssc06&catid2=kssc06c.
20. Korea National Statistical Office. Cause of death statistics. 2010. Retrieved January 14, 2010. from http://www.kosis.kr/domestic/theme/do01_index.jsp.
21. Korea Occupational Safety and Health Agency. Risk assessment for the prevention of cardiocerebrovascular disease at workplace (KOSHA Code H-46-2008). 2008. Retrieved June 28, 2010. from http://www.kosha.net/shdb/code/list.jsp.
22. Korea Occupational Safety and Health Agency. Occupational accidents and diseases statistics. 2010. Retrieved September 17, 2012. from http://www.kosha.or.kr/index.jsp.
23. Leon DA, Shkolnikov VM, McKee M, Kiryanov N, Andreev E. Alcohol increases circulatory disease mortality in Russia: Acute and chronic effects or misattribution of cause? Int J Epidemiol. 2010. 39:1279–1290. http://dx.doi.org/10.1093/ije/dyq102.
24. Meischke H, Kuniyuki A, Yasui Y, Bowen DJ, Andersen R, Urban N. Information women receive about heart attacks and how it affects their knowledge, beliefs, and intentions to act in a cardiac emergency. Health Care Women Int. 2002. 23:149–162. http://dx.doi.org/10.1080/073993302753429022.
25. Oliver-Mcneil S, Artinian NT. Women's perceptions of personal cardiovascular risk and their risk-reducing behaviors. Am J Crit Care. 2002. 11:221–227.
26. van der Weijden T, van Steenkiste B, Stoffers HE, Timmermans DR, Grol R. Primary prevention of cardiovascular diseases in general practice: Mismatch between cardiovascular risk and patients' risk perceptions. Med Decis Making. 2007. 27:754–761. http://dx.doi.org/10.1177/0272989X07305323.
27. Ware JE Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992. 30:473–483.
28. Whitworth JA. 2003 World Health Organization (WHO)/International Society of Hypertension (ISH) statement on management of hypertension. J Hypertens. 2003. 21:1983–1992. http://dx.doi.org/10.1097/00004872-200311000-00002.
29. World Health Organization. World Health Organization statistics. 2008. Retrieved November 20, 2010. from http://www.who.int/mediacentre/factsheets/fs311/en/index.html.
30. Xu W, Zhao Y, Guo L, Guo Y, Gao W. Job stress and coronary heart disease: A case-control study using a Chinese population. J Occup Health. 2009. 51:107–113. http://dx.doi.org/10.1539/joh.L8060.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download